Medicines Q&As
Q&A 17.6 Can acetarsol be used to treat proctitis?
Prepared by UK Medicines Information (UKMi) pharmacists for NHS healthcare professionals Before using this Q&A, read the disclaimer at www.ukmi.nhs.uk/activities/medicinesQAs/default.asp (Date prepared: April 2015)
Background
Acetarsol (an organic arsenic derivative) was formerly given orally in the treatment of intestinal amoebiasis and vaginally in the treatment of trichomoniasis. The use of arsenic compounds is now largely superseded.(1) However, acetarsol suppositories for intractable proctitis, still has a place in therapy when other treatments have failed.(2)
Answer
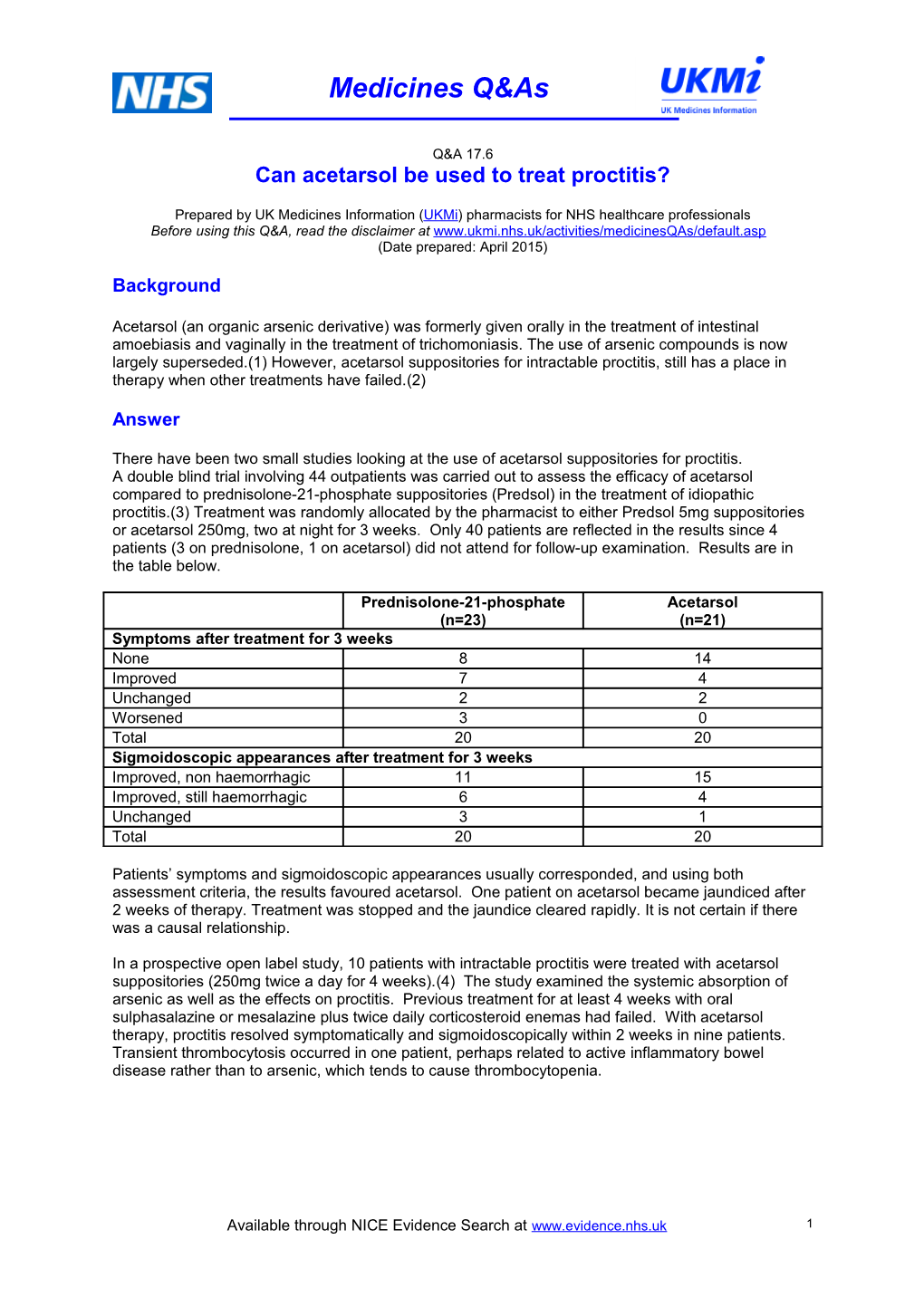
There have been two small studies looking at the use of acetarsol suppositories for proctitis. A double blind trial involving 44 outpatients was carried out to assess the efficacy of acetarsol compared to prednisolone-21-phosphate suppositories (Predsol) in the treatment of idiopathic proctitis.(3) Treatment was randomly allocated by the pharmacist to either Predsol 5mg suppositories or acetarsol 250mg, two at night for 3 weeks. Only 40 patients are reflected in the results since 4 patients (3 on prednisolone, 1 on acetarsol) did not attend for follow-up examination. Results are in the table below.
Prednisolone-21-phosphate Acetarsol (n=23) (n=21) Symptoms after treatment for 3 weeks None 8 14 Improved 7 4 Unchanged 2 2 Worsened 3 0 Total 20 20 Sigmoidoscopic appearances after treatment for 3 weeks Improved, non haemorrhagic 11 15 Improved, still haemorrhagic 6 4 Unchanged 3 1 Total 20 20
Patients’ symptoms and sigmoidoscopic appearances usually corresponded, and using both assessment criteria, the results favoured acetarsol. One patient on acetarsol became jaundiced after 2 weeks of therapy. Treatment was stopped and the jaundice cleared rapidly. It is not certain if there was a causal relationship.
In a prospective open label study, 10 patients with intractable proctitis were treated with acetarsol suppositories (250mg twice a day for 4 weeks).(4) The study examined the systemic absorption of arsenic as well as the effects on proctitis. Previous treatment for at least 4 weeks with oral sulphasalazine or mesalazine plus twice daily corticosteroid enemas had failed. With acetarsol therapy, proctitis resolved symptomatically and sigmoidoscopically within 2 weeks in nine patients. Transient thrombocytosis occurred in one patient, perhaps related to active inflammatory bowel disease rather than to arsenic, which tends to cause thrombocytopenia.
Available through NICE Evidence Search at www.evidence.nhs.uk 1
Medicines Q&As
The table below shows the blood and urine arsenic concentrations (microgram/L, medians and ranges).
Sample Blood Urine Prior to treatment <10 (0-13) 26 (7-70) After 1 week of treatment 48 (18-123) 6550 (1440-12580) After 4 weeks of treatment 18 (2-160) 1380 (38-6080) 1 week after completing 9 (4-15) 49 (29-69) treatment 4 weeks after completing 4 (1-6) 45 (41-78) treatment
The maximum blood concentration observed was 160µg/L at 4 weeks in a single patient, but the highest level was observed at 1 week, when the rectal mucosa remained obviously inflamed. Six patients had a urinary inorganic arsenic level considered hazardous in forensic practice (>200µg/L) after 1 week’s therapy. This remained hazardous in two patients after 4 weeks but both blood and urinary arsenic concentrations fell rapidly after treatment was stopped. This showed that arsenic is absorbed systemically from acetarsol suppositories. The fall in blood and urine concentrations between weeks 1 and 4 suggest that absorption, initially facilitated by permeable inflamed mucosa, is limited as the proctitis resolved. Adverse effects from arsenic concentration are unknown. Forbes et al did not find any clinical consequence from this but long-term therapy is not recommended.
Summary
The precise mechanism of action of acetarsol in proctitis is unknown. Acetarsol suppositories have been used for proctitis for many years at St Mark’s Hospital (Specialist Gastrointestinal unit). Proctitis can affect both patients with Crohn’s disease and ulcerative colitis in principle but proctitis is more likely in ulcerative colitis.(5) The usual dose used is 250mg bd (up to 3-4 weeks), after other treatments have failed. Arsenic is absorbed systemically but reduces as the proctitis resolves. No monitoring is necessary for short term treatment.(2)
Limitations
The evidence is limited: there are only 2 small trials, the most recent of which is from 1989, and included very few patients.
References
(1) Sweetman SC. Martindale: The Complete Drug Reference (online). Acetarsol (date of monograph revision 23/09/2011). London: Pharmaceutical Press, 2015. (2) MiDatabank enquiries: 42467, 44678, 45525, 50150, 55384, 93014,106123 (3) Connell AM, Lennard-Jones JE, Misiewicz JJ. Comparison of acetarsol and prednisolone-21- phosphate suppositories in the treatment if idiopathic proctitis. The Lancet 1965; i:238-239. (4) Forbes A, Britton TC, House IM et al. Safety and efficacy of acetarsol suppositories in unresponsive proctitis. Aliment Pharmacol Therap 1989; 3:553-556. (5) Pharmacy Manager (J Eastwood), St Marks Hospital. April 2015. Personal communication
Available through NICE Evidence Search at www.evidence.nhs.uk 2
Medicines Q&As
Prepared by Shaheen Sidik [based on earlier work by Wynn Pevreal and Caroline Fletcher], London Medicines Information Service (Northwick Park Hospital)
Date Prepared Updated April 2015
Checked by Varinder Rai, London Medicines Information Service (Northwick Park Hospital).
Date of check May 2015
Contact [email protected]
Search strategy Medline – 1950 to date. [acetarsol.af] [Limit to: Human and English Language and Publication Year 2013-current] Embase – 1980 to date [ACETARSOL] [Limit to: Human and English Language and Publication Year 2013-current] MiDatabank – acetarsol (past enquiries) NHS Evidence www.evidence.nhs.uk Clinical Specialist: Jackie Eastwood, Pharmacy Manager, St Marks Hospital.
Available through NICE Evidence Search at www.evidence.nhs.uk 3