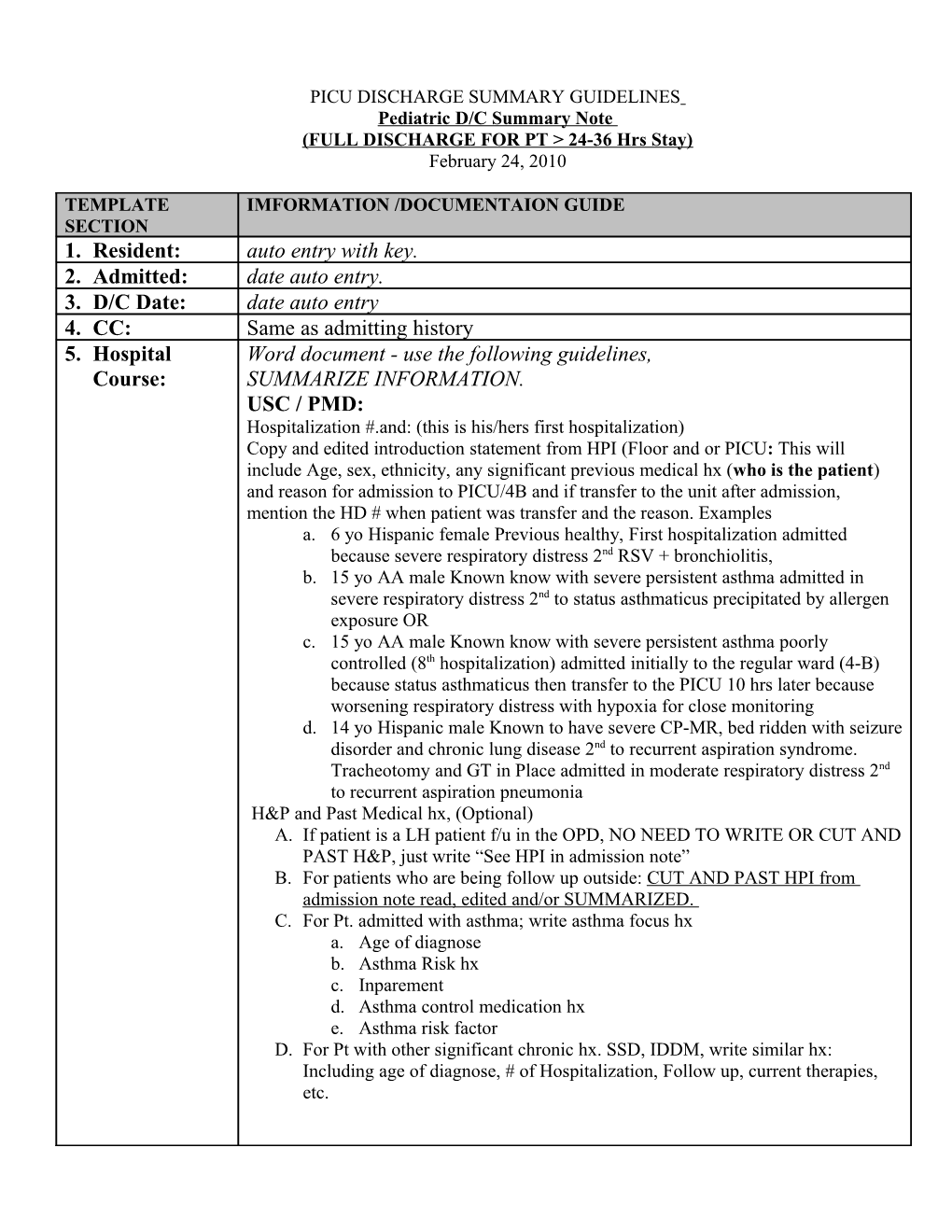
PICU DISCHARGE SUMMARY GUIDELINES Pediatric D/C Summary Note (FULL DISCHARGE FOR PT > 24-36 Hrs Stay) February 24, 2010
TEMPLATE IMFORMATION /DOCUMENTAION GUIDE SECTION 1. Resident: auto entry with key. 2. Admitted: date auto entry. 3. D/C Date: date auto entry 4. CC: Same as admitting history 5. Hospital Word document - use the following guidelines, Course: SUMMARIZE INFORMATION. USC / PMD: Hospitalization #.and: (this is his/hers first hospitalization) Copy and edited introduction statement from HPI (Floor and or PICU: This will include Age, sex, ethnicity, any significant previous medical hx (who is the patient) and reason for admission to PICU/4B and if transfer to the unit after admission, mention the HD # when patient was transfer and the reason. Examples a. 6 yo Hispanic female Previous healthy, First hospitalization admitted because severe respiratory distress 2nd RSV + bronchiolitis, b. 15 yo AA male Known know with severe persistent asthma admitted in severe respiratory distress 2nd to status asthmaticus precipitated by allergen exposure OR c. 15 yo AA male Known know with severe persistent asthma poorly controlled (8th hospitalization) admitted initially to the regular ward (4-B) because status asthmaticus then transfer to the PICU 10 hrs later because worsening respiratory distress with hypoxia for close monitoring d. 14 yo Hispanic male Known to have severe CP-MR, bed ridden with seizure disorder and chronic lung disease 2nd to recurrent aspiration syndrome. Tracheotomy and GT in Place admitted in moderate respiratory distress 2nd to recurrent aspiration pneumonia H&P and Past Medical hx, (Optional) A. If patient is a LH patient f/u in the OPD, NO NEED TO WRITE OR CUT AND PAST H&P, just write “See HPI in admission note” B. For patients who are being follow up outside: CUT AND PAST HPI from admission note read, edited and/or SUMMARIZED. C. For Pt. admitted with asthma; write asthma focus hx a. Age of diagnose b. Asthma Risk hx c. Inparement d. Asthma control medication hx e. Asthma risk factor D. For Pt with other significant chronic hx. SSD, IDDM, write similar hx: Including age of diagnose, # of Hospitalization, Follow up, current therapies, etc. PICU DISCHARGE SUMMARY GUIDELINES Pediatric D/C Summary Note (FULL DISCHARGE FOR PT > 24-36 Hrs Stay) February 24, 2010
HOSPITAL / PICU course: uncomplicated OR complicated HD # System by system, (For each system start with Patients presenting condition in the ED, treatments, studies, response to therapy and condition on admission to the PICU and carry on course mentioning Only relevant abnormal values / studies. Mention if any consults and recommendations given and condition on d/c) 1. NEUROLOGY (Neurosurgery if trauma). 2. RESPIRATORY. 3. CARDIOVASCULAR 4. FEN (mention admitting and discharge weight if small infants and/or prolonged hospitalization.) / Can combine FEN/GI if no significant problems / issues 5. HEMATOLOGY 6. GI 7. GU (Renal). Need to mention UA 8. INFECTION. (Need to mention Immunization review/update. 9. PSYCHOSOCIAL (mentions parents’ involvement. Pt seen by Soxial Services if any social issues address by SW. . 10. Others (Such as specific trauma / accidents / drug overdose related)
Example: (patient with status asthmaticus) NEUROLOGY: Since arrival to the ED pat. Has remained alert and active. Day of discharge, ambulating back to him/hersef RESPIRATORY: Patient presented to ER in severe respiratory distress RR 60 /min with significant desaturations (80 % in RA), treated aggressively with bronchodilators and MgS. With mild improving only transferred to PICU for further management. CxR did showed significant hyperinflation and PBT only. ABG if applicable. On admission to the PICU pt was improved by still in moderate respiratory distress RR 55 O2 Sat 95% on 50% aerosolized mask, lung exam with fair entry and diffuse wheeze. Pt was started on continue Albuterol treatment, IV Steroids and Oxygen. Initially he required 50 % given by aerosolized mask to keep saturations > 95 %. ABG showed ……., Required Bi-PAP support for 24 hrs. He gradually improved on Hosp Day # he was oxygenating well on RA, PEFR improved from 120 to 350. He did have productive cough and nasal discharge. Day of d/c he’s breathing comfortable RR 15, Lungs auscultation shows etc etc. PEFR. Started on control therapy with Flovent ….. CARDIOVASCULAR: on arrival to the ED Pt tachycardic HR 150, normal BP well perfuse. Tachycardia resolved as respiratory distress improved, no other issues FEN: Initially NPO for respiratory distress, on IV Fluids. Mild transient hypokalemia with K of 3.1 most likely 2nd to frequent albuterol treatments, improved on IV fluids with KCL. Last K 4.3. Maintained good urine output. No other issues. except for transients Hyperglycemia. HEMATOLOGY: mildly elevated WBC, no shift but eosinophylia. Normal H/H GI: no issues, initially NPO and on Ranitidine for GI prophylaxis. Day of discharge tolerating full PO well. GU /Renal: no issues, normal urine output. Normal BUN and Cr. Normal UA. PICU DISCHARGE SUMMARY GUIDELINES Pediatric D/C Summary Note (FULL DISCHARGE FOR PT > 24-36 Hrs Stay) February 24, 2010
INFECTION: remained afebrile but had productive and signs of infected rhinitis, treated with Zytromax. Immunization record reviewed, up to date. PSYCHOSOCIAL: Single mother on public assistance. Had problems with insurance and was unable to fill out prescriptions for control therapy. MGM smokes at home. Patient referred to social services. VN requested. OTHERS. If needed.
ASSESSMENT : 17 yo African American male with early onset severe persistent allergic asthma, poorly controlled (5th hospitalization 1st PICU admission) admitted with: 1.- Status asthmaticus with severe respiratory distress and hypoxia requiring BI-PAP support for 24 hrs. Respiratory distress and hypoxia resolved 2.- LLL collapse, resolved 3.- Allergic / Infected rhinitis, early sinusitis (clinically) improving on antibiotics
Plan: 1. D/C home with mother and VNS Services 2. Asthma education reinforced, AAP given and explained 3. Albuterol 2 puffs Q 4 hrs for 5 days then as needed as per asthma action plan 4. Prednisone 60 mg QD for 2 more days only 5. Complete 10 days of Antibiotics. Augmentin…. 6. Continue control therapy with: Flovent (220) 2 puff BID with spacer, Singulair 10 mg QHS 7. F/U in the Asthma /Chest clinic in 5 days and PMD in x days Seen and discussed with attending Dr. (WRITE NAME)