1
THE MAHARAJAH ANALYSIS: A MANAGEMENT PERSPECTIVE ON INDIA’S HEALTH CARE SYSTEM
GROUP MEMBERS Sireesha Bobbili 002227122 Say Khounborind 001236231 Caroline Lam 002128676 Karen Naik 001236884 Joy Tanega 001224260
SUMMARY
“Amidst the acceleration of a converging world, the inequities and disparities become strikingly evident. Whether in terms of educational opportunities, scientific and industrial technologies, communications networks or agricultural development, the gap of quality and accessibility, which exists between world societies, constitutes one of the major crises facing the human community. Nowhere is this gap broader and more complicated than in the field of health care.”
John H. Morgan, 1983 Notre Dame, Indiana
The objective of this report is to examine the developing trends to present the status of basic health care services in India with particular attention directed to the health care system. This is a general overview of India’s health care system. This report presents demographics that illustrate the physical state of India and its health care situation. As a result of Canada being a first world country and India being a third world country, there are many distinct differences. This report analyzes the similarities and differences as well as presents some advantages and disadvantages. Although India is still a developing country, there are some management practices they can offer which can be applied to help improve Canada’s health care system. If India expects to move forward in health care, they need to restructure their health care system to integrate sectors and to provide better health care to poor and rural communities. Finally, this report recommends some changes that will lead India’s health care system toward an effective and efficient reform that will increase the population health of India, now, and for generations to come. 2
In the past twenty-five years, India has made progress in improving the health status of its population. Between 1970 and 1993, life expectancy at birth increased from 50 to 61 years and infant mortality decreased from 137 to 74 per 1000 live births (The World Bank Group Operations Evaluation Department, 1997). India’s health policy during this period has been based on the assumption that primary health care is a basic right to which people should not be denied despite their inability to pay or for other socio-economic reasons. Therefore, India has public funding because they recognize the health care needs of the public. However, these services do not always address public health issues such as proper drinking water. At the same time, many health services have been inaccessible to the poorest rural and most vulnerable sections of the population because many services are privately funded. As a result, gaps remain in the effective delivery and quality of health services.
DEMOGRAPHICS AND HEALTH CARE INDICATORS
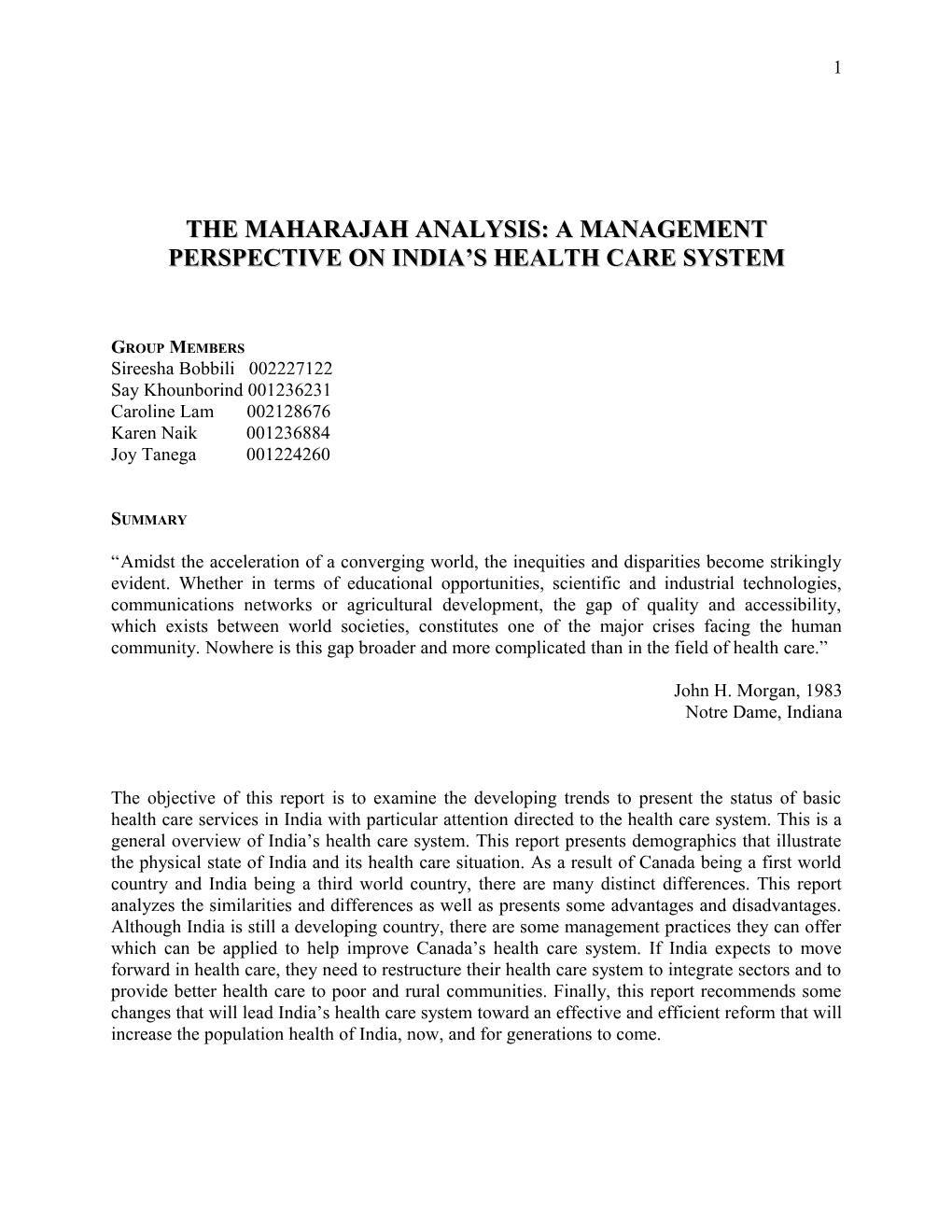
Population The Asian country of India is home to the world’s tenth largest economy in 1993 with a Gross National Product (GNP) of U.S.$290 per capita and in 2000 the world’s second largest population of 1,022,021,000 (Statistics: India, 2001). India is made up of 25 various states and 7 union territories, which are relatively diverse (Census of India, 1991). The country remains predominantly rural, with just 26% of its people living in urban communities. Yet in 1995 it had over 30 cities of one million or more residents including three of the world’s 20 largest cities— Bombay, Calcutta and Delhi—according to the United Nations estimates (Environmental Health Perspectives, 1996). Males make up 51.9% of the total population while females make up 48.1% (Census of India, 1991). Figure 1 shows that approximately 37% of the people are under age 15. The median age of both males and females range from 15-19.
Figure 1. Age Structure of Population
0-4 10-14 20-24
e
g 30-34 n
a Fem ale
R 40-44
e Male
g 50-54 A 60-64 70-74 80+
0 2 4 6 8 10 12 14 16 Percentage of Total Population
Caste System Where Canada has a class system, India has a caste and tribe system that is similar to the class system. Those in the higher castes (upper class) only associate with other high castes in society. 3
Those in the lower castes are left to try to advance among other low caste people in a very segmented society and are left at a disadvantage overall. Therefore the higher castes are given more opportunities in life while those of the lower caste are struggling to progress as the gap between high and low castes widen. The higher castes will rarely help the lower castes, which will increase the gap between those who have and those who have not. It is evident how this has and will continue to lead to many social and financial problems for certain groups while others groups enjoy a very high quality of life.
Health Indicators The Infant Mortality Rate per 1000 population (IMR) has steadily decreased over several decades and is still decreasing. According to the latest statistics, the IMR was 74 in 1995, 72 in 1996 and decreased to 71 in 1997. From 1995 to 1997 the Birth Rate per 1000 population has been steady near 27.5 and the Death Rate per 1000 population has been steady at 9.0 (Census of India, 1995- 97). Disability-Adjusted Life Years (DALYs) per 1000 population lost to Mortality and Disability in India was 235 and 103 respectively in 1990 (World Bank Operations Evaluation Department, 1999). The Disability Adjusted Life Expectancy (DALE) summarizes the expected number of years to be lived in what might be termed the equivalent of “full health”, overall India has a DALE of 53.2 years, males have a DALE of 52.8 compared to females with 53.5 (World Health Organization). The Major Causes of Death per 100,000 population in 1990 are: diseases of the circulatory system 227; infections and parasitic diseases 215; diseases of the respiratory system 108; certain conditions originating in the perinatal period 108; and accidents, homicides and other violence 102. A significant health problem in India is the number of people living with Human Immunodeficiency Virus (HIV); at 4 million people this is the highest incidence of HIV in the world (World Health Organization, 2000). In India the physician-patient ratio was 1 to 2,211, in other words 1 physician to every 2,211 patients in 1991. In 2000, the nurse-patient ratio was 1 to 2,083 in, which means that there is 1 nurse for every patient. The hospital bed-patient ratio was 1 to 1,357 in 1992, which means that there was 1 hospital bed for every 1,357 patients. Literacy has a significant influence on health and health practices in India, in 1991: 64.1% of males and 39.3% of females were literate (Statistics: India, 2001).
RURAL POPULATIONS
India is mostly rural with only 26% of its population living in urban settings (Rahman, 1996). Furthermore, one-third of India is living in tribal and hilly areas where health services are inaccessible. As a result, the population in these areas has a critical health status. Their health problems are associated with issues of food securities, underdevelopment and lack of infrastructure. A serious problem in rural communities is unsafe drinking water (Rahman, 1996). They do not have proper sanitation and infrastructure to supply proper drinking water to communities and the water is contaminated with bacteria and viruses. Another problem is that rural populations’ lack qualified primary health care physicians because most doctors choose to practice in urban areas. Many physicians do not want to practice in rural areas. In fact, physicians choose to become unemployed in urban centres rather than practising in rural areas because the majority of doctors come from urban sectors and if they pursue a rural community, it is considered a backward step in their profession. 4
THE ROLE OF GOVERNMENT
The state is responsible to provide and organize public health care. This includes central state and local governments, where health care is a state responsibility in terms of service delivery (The World Bank Group Operations Evaluation Department, 1997). The health care management system at the state level is inefficient and ineffective. Some of the problems are duplicating services of the different tiers of the health system and lack of coordination and integration between them. One of the government’s health care strategies is based on population-size norms and it is not specific health needs at the community level. Health problems at the community level are due to culture, religion, language and infrastructure. For example, Cholera is prevalent and it is a result of insufficient sanitary conditions and unclean drinking water. If proper drinking water is in place many health problems and health costs could be eliminated.
The government is currently addressing issues on the roles of public and private sectors because only 22% of health care is publicly funded; the availability of health care is a constraint on the population (The World Bank Group Operations Evaluation Department, 1997). Ill people are not receiving health care. Budget and resource allocation, management of health services, quality of care and work force are also being examined by the government because in order for India to move forward in health care, these areas need restructuring and development. Indians need affordable, advanced health care. For that reason, health care managers need to design quality management programs for health care facilities.
HEALTH CARE ORGANIZATION FUNDING
The health care organizations are funded in two ways: through government funding and private sectors. The government publicly funds health services throughout the country, encompassing primary health centres to hospitals. The services provided are preventative and they include immunization, natal care and infectious disease control. These services are free of cost to the consumer. In addition, they account for 22% of total health spending and 1.3% of Gross Domestic Product (GDP) of government spending (The World Bank Group Operations Evaluation Department, 1997). The immunization programs introduced by the government and by United Nations have been successful. Polio, diphtheria and whooping cough have a reduced incidence reported; however, communicable diseases such as tuberculosis, malaria and HIV are still prevalent in India. The government also spends funds on the Indigenous Systems of Medicines (ISM). The ISM practitioners practice a mixed form of medicine that uses both primary and alternative health care. The average spending of ISM is around 2% of the health budget.
Health centres and hospitals are located in urban areas; therefore, rural residents who do not have access to health centres do not receive adequate health care. Since only a few health services are publicly funded, private funding exists and is dominant.
A private sector of for-profit, fee-for service practitioners is the dominant role in individual care in India. “The private sector accounts for 78% of overall health expenditures and 4.71 of the GDP” (The World Bank Group Operations Evaluation Department, 1997). Per capita private 5 health spending in India is amongst the highest for developing countries. Because a large percentage of health spending is private, only those people who can afford to pay for health care acquire it while less fortunate people (low SES) suffer with sickness.
PAYMENT OF HEALTH SERVICES
In general, health expenditure per capita in India is very low. Nationwide health care utilization rates show that the majority of India’s health care system is privately funded. The public sector is funded through government taxes and the physicians are salaried. Nevertheless about 30% to 40% use some type of insurance plan whether it is through employment or private insurance. Health services are directed mainly at primary health care and are financed almost entirely from patients through out-of pocket expenses. The reliance on such a high proportion of funds from out-of-pocket sources in India has placed a monetary burden on the poor.
THE LINK AMONG HEALTH CARE PROVIDERS
Because India lacks technical efficiency, the link among health care providers is weak. Procedures are duplicated and other processes are out of date. Thus, this creates a problem because this increases costs for the patients in a privately run health system. Panchayati Raj Institute (PRI) is the local administration system and it is used from the village to the district to ensure intersectorial collaboration (Revamping Primary Health Care in India, 2001). To improve the effectiveness of the health care system, a computer-compatible health management information system was designed with 12 participating states. This idea started in 1992 –1993 and presently it is operating in 2 states and the others are in the process of implementation (Country Health Profile, 2001).
HEALTH CARE PROFESSIONALS
India has many physicians, but it lacks infrastructure to integrate health care delivery between health care institutions. Furthermore, most health care fees are spent on professional salaries. “Almost 80% of payments are spent on salaries and the other 20% are available for drugs, equipment and other necessary supplies” (Revamping Primary Health Care in India, 2001). Since the majority of payments are spent on salaries, most physicians choose to practice in urban settings due to high population densities of wealthier people who can afford health care.
ALTERNATIVE HEALTH CARE IN INDIA
Since the second millennium BC, indigenous systems of medicine have been widely practiced. The art of healing holds a vitally important place in Indian culture and societal belief systems. Alternative health care practitioners are popular and integral parts of health care in rural communities. Traditional health care practices such as Ayuverdic medicine, homeopathy and naturopathy still play a significant role in maintaining the health of the majority of the population.
The most dominant category of India’s indigenous health care system is Ayuverdic medicine. Ayuverdic medicine is rooted in the books of the ancient Vedas, which are composites of Greek, 6
Muslim, Arab, and Persian writings that not only delineate the causes of disease but also are broadly consistent with more general Hindu philosophy (Morgan, 1983). Ayuverda, meaning the “science of life”, originated in the belief that health is dependent on a balanced state of all elements in the body (Discover India, 2001). This balanced state is measured both quantitatively and qualitatively with respect to all aspects affecting the individual. Due to Ayuverdic medicine’s strong foundation on religious beliefs associated with Hinduism and Islam, devout Hindus and Muslims are encouraged to seek health care from a variety of traditional folk practitioners. This type of practice hence flourishes in the specialization of its practitioners to the religious backgrounds of their patients.
A subcategory of Ayuverdic medicine is known as Unani, which is the Muslim form. In this type of practice, alternative health care providers carry out procedures that are consistent with the religious and philosophical components of Islam (Discover India, 2001). Similarly, another sector of Ayuverdic medicine customizes their practices in congruence with the lifestyle and culture of Hindu patients; encompassing such elements as dietary habits, prescribed remedies and treatment plans for their patients. Today, there are approximately 95 Ayuverdic and 16 Unani training centers functioning in the country (Discover India, 2001).
Outside of religious specialization, Indigenous Medical Practitioners (IMPs) with Ayuverdic training may also be treating patients by using homeopathic and naturopathic techniques. Homeopathy, introduced in India through British influence, is rooted in the principle that “like cures like” (Morgan, 1983). Naturopathy, on the other hand, relies on the curative forces of nature to both combat disease and promote health (Morgan, 1983). These principles are put into practice in alternative institutions called “nature cure ashrams” literally translated as “monastic center for retreat”. The Ashram translates Ayuverdic theories to medical regimens based on naturopathic techniques of “diet, quiet, merriment, and rest”. Since ashram institutions and IMPs, do not rely on expensive equipment and technology; it remains an attractive alternative to India’s poorer population. As a result, IMPs are more dominant in rural areas in providing health care than their allopathic counterparts.
DIFFERENCES BETWEEN THE HEALTH CARE SYSTEMS IN INDIA AND CANADA
India and Canada are countries at very different stages of development. India is a developing nation with a large, young population where infrastructure still needs to be developed in a majority of the country. In comparison, Canada is a well-developed nation, with an older population where a larger percentage is within the 50 - 65 age group.
Due to the countries apparent differences, each one has initiated health policies according to the major issues at hand. For example, India has initiated various programs to deal with problems associated with improper sanitation, nutrition, housing and poverty. These are also problems in Canada, although not to the extent that they exist in India. Therefore, there will be many differences between the two health care systems. Only differences dealing with the system and not the conditions of the country will be highlighted.
1. Health Insurance Canada’s health care system is continually referred to as a ‘single payer system’. It has a publicly funded insurance system where both physicians and hospitals control costs. There is only one 7
‘payer’, which is the government. There are no alternative programs, such as private health insurance, that are available to Canadians with respect to basic health care.
Under this mandate, Canadians can receive treatment from any physician or hospital in the country. A health insurance card that is issued to all eligible residents of a province must be presented at each visit. Therefore, they are not required to fill out forms for insured services and Canadians are not billed directly for these services.
Although each province and territory in Canada has its own system and has developed its own method of financial support, there is a consensus between provinces. It states that the health care system will provide treatment of any Canadian citizen, regardless of location. This adheres to the basic principles of universality and portability in the Canada Health Act.
Those in high and middle SES have no alternative to this public insurance; therefore it is guaranteed that it is funded adequately. Additionally, cost controls insure that everyone including the poor who use the same system will receive the same quality of care.
Supplementary health benefits, such as prescription drugs, dental and vision care, assistive equipment and appliances (i.e. prostheses, wheelchairs), and allied health professionals (i.e. Chiropractors) are partially covered under the public insurance system. These services are mainly privately financed, although provinces and territories provide some additional benefits. The out- of-pocket expenses may be dependent on income or ability to pay. People usually acquire private health insurance through an employment based group insurance plan. However, these insurance plans are restricted from offering coverage that duplicates that of the government’s public programs.
In comparison, India’s system of insurance is predominantly private. Private health insurance is controlled by a set of non-competitive corporations, which are owned by the state. These corporations are poorly regulated and exclude many consumers. Private policies only account for 3 million of India’s population. Therefore Indians are required to pay for health care out of their own pockets unless they are covered by a social insurance plan.
With only 3 percent of India’s citizens being covered by social insurance schemes, such as the Employee State Insurance Scheme (ESIS) and the Central Government Health Scheme (CGHS), there is restricted coverage of the population. ESIS operates as an independent organization, covering 7 million employees and is the largest mandatory insurance program that covers only a fraction of eligible employees (Perspectives On Health Care in India, 2001). It does not function as an insurer, but as a health service for lower income workers. CGHS is run by the Ministry of Health and Welfare and covers 3.5 million beneficiaries (Perspectives On Health Care in India, 2001). Due to insufficient social insurance, individuals contribute to 78 percent of health care spending. This results in a high burden of costs for most segments of the population, with the household expenditures on heath care ranging for 2% to 8% of monthly income. The government offers free health care for lower SES, but all SES groups usually exploit it. The Indian government lacks an effective administration mechanism to monitor free medical services to the disadvantaged population or to collect user charges from the higher SES population. As a result, wealthier patients utilize services disproportionately. 8
The large difference between India and Canada is the millions of people with lack of or insufficient coverage in India. Additionally, India’s citizens are losing everything and becoming destitute just to cover medical expenses. In Canada, the benefits to the entire population certainly indicate that this health care approach should be observed and considered by India’s policy makers.
2. Technological Implementation Programs A recent initiative of the Canadian government is the implementation of the Telehealth program. According to Industry Canada, Telehealth is “the use of communications and information over large and small distances”. This new program would be beneficial to rural communities by advising and supporting rural health workers in dealing with problems that would otherwise require patients to travel long distances to access specialized health care in urban centers. It is also advantageous because it would integrate information and overcome obstacles created by geography and differing information systems that are currently in use. The program was initiated in 1999 and the implementation is currently in progress. There are different components that Telehealth incorporates. They are as follows. 1. Telemedicine: Consultations in dermatology, radiology, cardiology and psychology Diabetes education Rehabilitation 2. Tele-education for health professionals, patients and public Physician and nursing education, Patient and consumer information via Internet, telephone and CD Rom 3. Telemonitoring, Telehomecare, Emergency networks Monitoring of hemodialysis and cardiac patients Remote controlled infusion for oncology patients Assisted home care for the elderly Emergency systems linking houses to the hospital 4. Electronic patient records and information Collection of all of an individual’s relevant interactions with the health care system Available to health care professionals at any location in the country Disclosure of information is in control of the patient Duplication of tests and procedures is limited Health records are linked within a network that is accessible to relevant facilities (i.e. pharmacies, clinics).
India’s health care system has developed a computer compatible health management system. Infomatics was implemented as a key tool and strategy for development. The main purpose of the system is to maintain personal health records and files that consist of summaries of health indicators and interventions for the community. An obstacle that India faces is the files of health interventions are passed up the hierarchical ladder and therefore difficult to obtain. In addition, few private facilities actually keep patient records for their clients. Facilities run by the government assumes that the patients are responsible for their own records. Yet others maintain patient records at the health care delivery site. Infomatics was designed with 12 participating 9 states and initiated in 1992. Presently, it is only operating in 2 states, which shows the difficulty in attaining records as well as resources to implement the system in a large population (Perspectives of Health Care In India, 2001).
India’s Infomatics system is not as advanced as Canada’s Telehealth system because it would require a great deal of resources and infrastructure to implement. Currently, India does not posses these resources to successfully implement a more advanced system.
It is very difficult to acquire medical records in India because patients are responsible for their own records. Canadian medical records are more readily available because they are kept within the facilities where they were originally established. Therefore the method of medical record keeping in India has hindered the process of implementing a technologically advanced program.
3. Funding Health care in Canada is financed primarily through provincial and federal taxes (i.e. personal and corporate income taxes). Some provinces use auxiliary funding methods, such as sales taxes, payroll levies, and lottery proceeds that supplement health care funding. In these cases, they are not marked specifically for health and are added to the central revenues of the province; they play a minor role in health care financing.
The federal government’s contribution to provincial health programs are provided in a single block transfer, called the Canada health and social transfer. Federal funding is transferred as cash contributions and tax points. This represents 70 percent of Canada’s total health expenditures, while the remaining 30% is financed privately through supplementary insurance, employer-sponsored benefits, or directly out of the pockets of the individuals.
In contrast, India’s health care system is highly privatized. The overall health spending as a percentage of the Gross Domestic Product (GDP) is 5.6% (Development of the Health System). This is substantially high when compared to other developing nations. The government’s role in health care is extremely low, and accounts for 22% of total health care spending in India. As a percentage of GDP, India’s government expenditures on health is about 1.3% of GDP as compared to an average of 2.2% of GDP in other developing nations (Perspectives of Health Care in India, 2001).
The remaining health spending is comprised of private providers that are mainly small independent facilities (i.e. hospitals) and they are largely urban based. The private sector has grown in a fragmented manner with services being delivered from many small dispensaries, nursing homes and hospitals.
The Canadian federal government provides 70% of Canada’s health expenditures, which leaves only 30% to be covered by private funds. The government cares for Canadian health programs and facilities; less emphasis is on acquiring funds from the private sector. India’s health care system depends largely on private contributions because the government only provides 22% of health expenditures. This may be a contributing factor to the inaccessibility to lower SES groups. 10
4. Provincial Rural Incentive Plans In Canada, the majority of medical graduates are from urban centers and have been trained in urban hospitals. Approximately 90% of graduates decide to enter into urban practices (Understanding the Canadian Health Care System, 2001). A characteristic that is unique to Canada is the practice of offering incentives to physicians. These physicians practice in rural areas with a deficient number of health care personnel. The province has monetary incentives for physicians who decide to move to rural and remote areas. Most provinces rely on this system to draw physicians to smaller communities. The system has been successful in attracting individuals, but has been unsuccessful in retaining them in appointed areas. Therefore the gap between rural and urban services grows.
India is comprised mainly of rural communities and also faces the problem of attracting physicians to rural and remote areas. India does not offer any incentives for physicians to move to rural areas. Therefore, it is extremely difficult to draw physicians to rural areas because of lower expected wages, isolation and the social norm of practicing in urban centers.
Canada has an incentive program that appeals to physicians to practice in rural communities. Conversely, India has no such program. This could account for the lack of health care personnel in rural regions across India. Although Canada has a difficulty in retaining these practitioners in rural locations, the incentive program is a step in the right direction. India’s policy makers must take this into account in order to close the rural-urban disparity in health care personnel.
INDIA’S MANAGEMENT STRATEGY IN A CANADIAN CONTEXT
1. Primary Health Care A management strategy that Canada can adopt from India is their commitment to primary health care, health promotion and health prevention. Both Federal and State governments in India emphasize primary health care as a way to decrease health expenditure that would be lost to tertiary care if primary care were not supported. By preventing disease or infirmity from occurring, a large proportion of health resources saved in tertiary care may be redirected to address other health needs. Canada should consider adopting this strategy to maximize the efficiency of its health care budget. Canada places too much emphasis on tertiary care, for example drug treatments make up the largest percentage of Canada’s Health Care expenditure. If both the Canadian Federal and Provincial governments allocated more resources towards primary care—such as in health promotion, education and prevention—less of the budget may be needed for tertiary care, consisting of drug treatment and surgery. Increased promotion and prevention will not have immediate results, but the long-term advantages identified in India will also be beneficial to Canadians in further improving the health status of the Canadian population (Revamping Primary Health Care in India, 2001).
2. Indigenous Systems of Medicine Another management practice practised in India that can be applied to the Canadian health care system is the Indigenous Systems of Medicines (ISM). Most ISM practitioners in India practice a mixed form of medicine that includes both indigenous and primary health care. India uses ISM practitioners to provide low cost medical services to rural areas (Perspectives on Health Care in 11
India, 2001). ISM can be applied to Canada because these practitioners can be used in isolated rural communities where a physician is unavailable.
As a developing country, India’s health care management strategies are currently developing. Their health care system has not yet achieved the level of care present in Canada, a developed country. According to the World Health Organization (WHO) ranking by DALE—which summarizes the expected number of years to be lived in what might be termed the equivalent of “full health”—Canada ranked 12th with a DALE of 72.0 while India was ranked 134th with a DALE of 53.2 overall (World Health Organization, 2001). Since India’s health care system is not as advanced as Canada’s system, there is a limited amount of management practices that Canada would be able to adopt from India to improve Canada’s current health care system. As a result, it is difficult to identify any additional management techniques from India, other than the one stated above, that may be beneficial to progress the Canadian health care system.
EVALUATION OF INDIA’S HEALTH CARE SYSTEM
ADVANTAGES
1. Government recognition that health care is a basic right for the people The government of India recognizes and that health care is critical and essential to help maintain a relatively healthy lifestyle. In assuming that health care should be provided regardless of SES (eg. financial distress), the government presents a public funding health care system that is available to those who are unable to participate in the private health care system. This serves as a very valuable resource for the population of India because many people live in poverty and are seriously in need of health care. As a result of their poverty, they are denied access to or participation in the private health care system due to financial instability. Although publicly funded physicians may not represent a very large portion of the overall number of practitioners, this establishes that the government has recognized and attempted to restructure this part of the delivery system.
2. Public health services are focused on prevention Although the public sector is very small in terms of the entire health care system, the main focus is aimed at prevention, which is the core of the problem. India is recognized as a third world country, where acute illnesses such as infectious and parasitic diseases are the second most common cause of death. As a result, providing vaccinations to protect against preventable ailments has shown significant results in decreasing the number of deaths due to simple illnesses. Other primary health care measures that have been taken are in areas of natal care and infectious disease control. Each of these primary health care strategies have been successful in decreasing overall mortality rate and more importantly, decreasing the IMR.
3. Government recognition of health care unavailability to those in lower SES The public sector represents 22% of the health care budget, while the remainder is comprised of various private practices. This small percentage of public health care is insufficient to serve the portion of the population who live in poverty, therefore those who need it most. The unbalanced distribution of public and private services aimed to deliver 12
health care to those of lower SES and higher SES groups respectively, have left a void in the delivery of public health care. Although the government originally addressed this issue by implementing a public health care system funded by the government, they have come to the realization that there are still insufficient health care resources available to the lower socio-economic groups. As a result, the government is further addressing the issues of public and private health care to accommodate the lack of service delivery.
DISADVANTAGES
1. Publicly funded services do not always address public health issues (eg. quality of drinking water) Although publicly funded services are focused on prevention and primary care, there is not enough focus placed on public health issues, which are the root causes of illness in India. The quality of water is relatively poor and unsuitable for drinking. The higher socioeconomic groups bypass this problem by purchasing bottled water that has been filtered, therefore protecting themselves from contaminated water. However, lower socio- economic groups do not have the financial resources to purchase bottled water. Thus, the use of the contaminated water further aggravates any infections they may have, and contributes to the lack of hygiene present in their system. If public health issues are addressed and eliminated, individuals of lower SES will be able to rely on basic needs to help improve their health.
2. Due to privatization, majority of health care is inaccessible to the poor The private health care system represents 78% of health care expenditures, which is disproportionate to the population who can afford private health care. As a result, most of the health care provided is not accessible to those who need it most, namely the poor. The poor are the most vulnerable to acute diseases, however private health care is not available to them due to lack of monetary funds. This conveys that the majority of the population (those who are poor) are unable to use the majority of the health care system (the private sector).
3. Major health centres are located in urban areas In India, 74% of the population is distributed across rural areas, while only 26% are in urban areas. However, health centres and hospitals are located in urban areas, which limits access to the population that lives in rural areas. This is unfortunate because the poor tend to reside in rural areas, thus decreasing their likeliness to be able to access the health care system. Aside from the lack of funds to use the privatized health care system, they also lack the necessary transportation that will enable them to reach the health units in urban settings.
4. Physician practicing in both the public and private sector The health care system in India allows physicians to practice in both the public and private sectors; consequently, they take advantage of doing so. The distribution of time spent in each sector is aimed towards freeing up high-volume times to practice in the private sector thereby maximizing their income. One such scenario would be physicians who practice in publicly-funded hospitals in the late hours of the night until early morning, then transferring to private hospitals in the afternoon and evenings when they 13
are expecting a higher volume of patients to require their expertise. This acts as a restraint to the public health care system because these hospitals may only be open for a portion of the day, and during the times when accessing the hospital is most difficult.
RECOMMENDATIONS FOR INDIA’S HEALTH CARE SYSTEM
In response to the challenges faced in the health sector in India, it would be important for the Indian government to undertake a series of measures to increase the effectiveness of their health care system and initiate a process of reform. All aspects that shape the health care system such as environmental, social, structural, and governmental sectors are significant in addressing modifications in India’s health care system. The following are specific recommendations that can be implemented in the different sectors of India’s health care system.
ENVIRONMENTAL SECTORS A critical problem in most third world countries such as India is poor environmental conditions. This leads to common parasitic diseases that are most prevalent amongst the lower SES populations due to lack of sanitation. Therefore, changes in the environment are significant and integral in the improvement of the overall health status of the country. We recommend addressing two major environmental issues:
1. Water Pollution: Action should be taken to clean up sewage systems and sources of drinking water. This is especially the case in rural communities where most of the poorer populations reside; they cannot afford electricity to sterilize water or buy bottled water. As a result of inadequate water conditions, common parasitic diseases such as malaria, cholera and diarrheal dehydration emerge in rural communities. Parasitic diseases from water contamination are the second leading cause of disease in India. By increasing water quality, common diseases caused by bacteria and poor water conditions can be prevented.
2. Air Pollution: Action should be taken to minimize air pollution. Although policies are in place to minimize car emissions and the amount of air pollution that is caused by industrial companies, many regulations are not enforced due to inefficiencies in governmental management. Legislation and regulations should be created to enforce and promote such environmental awareness. Given that industrial companies and motor vehicles are components of urban communities, most of the problems associated with air pollution are most apparent in the urban population. Since, respiratory infections are the third leading cause of death in India, minimizing air pollution is very critical in increasing the health of the population. Specifically, decreasing air pollution can decrease the occurences of chronic eye irritations, bronchitis and respiratory problems in the urban sector. For younger children suffering from malnutrition, these respiratory problems are magnified by poor sanitation. Indirectly, air pollution affects rural populations because it causes acid rain, which in turn, affects the quality of water.
SOCIAL SECTORS Social issues are also significant in modifying India’s health care system. Since health care philosophies and attitudes are rooted in the society’s belief systems, the modification of social beliefs and paradigms should also be addressed: 14
3. Change the Philosophy and Education of Health Care Providers. Education of health care professionals should be geared towards primary and secondary rather than tertiary care. This will fulfill the country’s need for preventative (primary) rather than curative (tertiary) health care delivery practices. Also, training auxiliary workers and non-skilled medical workers in rural areas to have more responsibility in primary health care would eliminate problems in rural communities where physicians are scarce. They can be trained to follow standardized protocols in curing common ailments within communities. This greater emphasis on preventative care would decrease the incidence and burden of acute illnesses in India. These programs would also increase accessibility in rural communities.
4. Encourage the importance and credibility of Alternative health care practices such as Ayuverdic medicine, Unani, and local health traditions in curing common ailments. This can also be another form of disease prevention and health care promotion, which can be beneficial if implemented into the health care system. Since alternative healers are more common in rural communities, they can be the first source of health care in preventing and curing common diseases as a means of health promotion in rural populations. This will maximize the use of local resources and encourage the public to rely on community support rather than professionals. In addition, this allows the responsibility of the overall social welfare and health to be distributed amongst two models of health care delivery within India.
5. Promote active participation of people to manage their own health. Common disease prevention and health promotion programs can be offered to enable the public to manage their own health. By putting more responsibility of health status at the individual level, we can encourage self-reliance on using preventative measures. Since most of the lower SES populations are illiterate, other forms of communication can be used to educate the public. The use of media and word of mouth can be adopted in the goal of increasing the program’s effectiveness. Unlike their western counterparts, most of the populations in India are easily influenced by popular culture and the media. These persuasive tactics can be used as an advantage to persuade the public and also as a means to change individual and collective beliefs.
GOVERNMENTAL AND POLITICAL SECTORS The system needs to have a suitable governing body that can control, regulate, and evaluate the performance of the whole system. This can bring about an evidence-based approach to the system and an effective way to reform deficiencies within the system. This can be executed with the following recommendations:
6. Decentralize state planning and health care delivery to community level organizations. Decentralized governance and local level participation can improve the health care system through better monitoring of health system functions at the local level. Credible community level organizations such as the PRIs can be used to deliver basic health care services customized according to the unique needs of each community. Since India’s population is so diverse, each region of the country will have special needs and varying 15
diseases. This strategy will allow each state and each community to have the opportunity to deliver health care in the most efficient way by targeting their specific needs.
7. Strengthen the linkages between Governmental and Non-Governmental Organizations (NGOs) such as volunteer organizations. NGOs can be used to deliver primary health care and as a first-referral service in rural communities where they are most prevalent. The Government, which is the major provider of the public health care system, can increase its coverage in collaboration with NGOs and PRIs as its influential body. Non-Governmental agencies can be a means of disseminating public health messages by involving them in information, education and communication practices in changing societal attitudes of health.
8. Re-evaluate priorities within the health care budget. Modify the allocation of resources between primary, secondary, and tertiary levels of care according to a need-based approach. It is evident that primary and secondary health care requires more emphasis and financing. Since a greater proportion of the population is located in rural areas, the allocation of funds needs to be redirected from the urban to the rural sector to accommodate population distribution. The overall state finances can be improved by reducing overall public expenditures on subsidies, salaries and poorly targeted welfare programs. In this way, the state can redirect these funds to the public health sector and use the allocated budget more effectively.
9. Increase opportunities for contracting out to private agencies that offer support services and mainstream diagnostic and clinical services. A means of increasing efficiency and effectiveness is to contract out mainstream services such as laundry, sanitation, dietary, and mainstream diagnostic services. Contracting out to credible for-profit agencies is an efficient way to maximize the effectiveness of the system and allow the health care providers to concentrate on the actual health care of the patient. This would also free up time for health care providers to service more patients within their time frame. In addition to health service benefits, this strategy would also lead to successful management of the system because it would present a means in monitoring the system and a way to eliminate inefficient staff.
10. Increase Government capacity to monitor and regulate health care provision, and health policies. The government can take an active role in enforcing the legislations and policies for the health care system. They can setup standards for health care providers and create effective means in evaluating the performance of the health care system. Regulation can be administered in different levels of the system such as the state level, community level and through the means of a professional body (Indian Medical Association). Also, the government can enforce greater fines for any deviant behaviors inconsistent with the health care reform plan. Another way to control the system is by community policing. This would make healthy behavior mainstream in the higher SES class that consequently creates societal standards for the rest of the population. In this way, society will be operating in a form of self-surveillance, which can monitor and minimize deviant behaviors. This can be used in creating new social norms amongst the public with respect to health care and disease prevention. This can eventually lead to creation of new laws 16
and legislation in improving the health status of the population. An example of this is smoking in Canada. It is no longer acceptable to practice in most social settings, which lead to the implementation of regulations prohibiting smoking by municipal by laws
STRUCTURE OF INDIA’S HEALTH CARE SYSTEM The analysis of the foundation and the structure in revamping India’s health care system is an obvious requirement. Concerns such as integration and workforce issues between the rural and urban sectors are significant in attempting to implement change in the health sector. We propose the following recommendations in improving the infrastructure:
11. Reorient health care strategies to integrate a need-based approach with the population- size based approach. In order to enhance effectiveness, efficiency and accessibility of health care services, states should integrate the current population based approach with an approach, which addresses the health care needs of each community, rooted in disease patterns within each community. In any way possible, local administration should be included in planning programs based on basic health services as a means to reflect the needs in the community level. This would allocate resources in the most organized way and would serve those of the population that are most in need of health services.
12. Increase communication amongst health care institutions in order to decrease duplication of services. Enhance communication technology that can help health care providers communicate amongst each other and therefore lead other auxiliary health care providers in rural communities, regardless of location. Information technology services can be strengthened in order to increase collaboration amongst health care institutions and reach primary health care centers in rural communities. For example, this type of technology can be a means for physicians to acquire updated medical records. The problem of limited scope of health care services can be alleviated by investing in technology that can integrate all the elements in delivering health care to communities. Also, this can reduce cost and increase efficiency by minimizing the duplication of services amongst health care providers. It is interesting to note that Canada also needs to address this issue as well.
13. Increase effectiveness of primary and secondary rather than tertiary health care. Since common diseases in India can be prevented, increased emphasis is needed on preventative rather than curative medicine. Initial investment would be needed in order to implement a widespread program that can, for example, administer vaccinations in order to eliminate common diseases. It is a considerable short-term investment that can result in long-term benefits for the health care system as a whole. This is cost-effective because it can induce permanent change for public health and in the use of the health care system in the future.
WORKFORCE ISSUES
14. Create incentives for health care providers to work in rural communities. These incentives can include monetary as well as non-monetary benefits. Monetary benefits can include an increased salary for health care providers that work in the rural 17
sector and free education for students who guarantee working in the rural sector for a period of time after graduating. Non-monetary benefits can include preferential school admissions for children in rural communities and also required practice for internship in the rural sector for a certain time period as a requirement for graduation. These incentives are geared to attract more health care providers in rural and remote communities where they are most needed. Also, the mandatory practice in the rural sector as graduation requirements can guarantee health service in rural communities for as long as there are health care providers in school.
15. Increase the professional status, control and involvement of auxiliary workers in health care delivery. India’s health system has an hourglass structure. There is a surplus of physicians, deficiency of auxiliary workers and another surplus in non-skilled workers. Increasing the attractiveness of the auxiliary health care provider’s profession is needed in allowing the responsibility of health care to be redistributed equally amongst professions in the health system. By increasing the professional status of auxiliary workers, health care service can be administered by a partnership between the physician, auxiliary worker and the non- skilled worker. Using a tiered referral system where the non-skilled worker is trained in primary health care to treat common illnesses by using protocols, the health care system can use this team of staff to encompass all of primary, secondary and tertiary levels of health care.
Finally, it is essential that an ongoing program of evaluation of these recommendations should be carried out covering various sectors—environmental, social, governmental, and structural—so as to determine their effectiveness and the need for reorganization of India’s Health Care System from time to time. 18
BIBLIOGRAPHY
1. Harrison, M. Public Health in British India. New York: Cambridge University Press, 1994.
2. Zurbrigg, S. Rakku’s Story: Structure of Ill-Health and the Source of Change. Madras, India: George Joseph, 1984.
3. Morgan, J.H. Third World Medicine and Social Change. New York: University Press of America Inc., 1983.
4. Hetzel, B.S. Basic Health Care in Delivery Countries – An Epidemiological Perspective. New York: Oxford University Press, 1976.
5. Saltman, R.B. The International Handbook of Health – Care Systems. New York: Greenwood Press, 1988.
6. Chen, L.C., Gupta, M. D., and Krishnan, T.N. Health, Poverty and Development in India. Delhi: Oxford University Press, 1996.
7. Sharma, A.N. Modern Trends in Anthropology: Some Socio-Demographic and Nutritional Aspects of Health. New Delhi: Northern Book Centre, 1989.
8. Chen L.C. Disaster in Bangladesh. New York: Oxford University Press, 1973.
9. John Hopkins University Department of International Health. The Functional Analysis of Health Needs and Services. New York: Asia Publishing House, 1976.
10. Choudhuri, S.R. Sickness Insurance in India and Britain. Calcutta: The World Press Private Ltd., 1966.
11. Gangulee, N. Health and Nutrition in India. London: Faber and Faber Ltd., 1939.
12. Rahman, Q. “Focus: The Anguish of India.” Environmental Health Perspectives. Mar. 1996: 104(3). 18 Nov. 2001
13. World Health Organization. Emergency and Humanitarian Action: Baseline Statistics for India. 2000. 20 Nov. 2001
14. World Health Organization. Transmittable Diseases. 2000. 20 Nov. 2001
15. World Health Organization. Healthy Life Expectancy Rankings. 2001. 20 Nov. 2001
16. Census of India. Table 2: Estimates of Birth Rate, Death Rate and Infant Mortality Rate for the latest three years, 1995-1997. 1998. 21 Nov. 2001 < http://www.censusindia.net/srsboct98table2.html>
17. Census of India. Table 7: Distribution of Population by Age and Sex 1991. 1991. 21 Nov. 2001
18. Nations of the World. Statistics: India. 21 Nov. 2001
19. Age Structure of Population. 21 Nov. 2001
20. Revamping Primary Health Care in India. 22 Nov. 2001
21. The World Bank Group Operations Evaluation Department. A Comparative Review of Health Sector Reform in Four States: an Operational Perspective. 1997. 23 Nov. 2001
22. The World Bank Group Operations Evaluation Department. Health Care in India: Learning From Experience. 1999. 23 Nov.2001
24. The World Bank Group. The World Bank Group and Health Sector Development and Disease Control in India. 23 Nov. 2001
25. Discover India. Social Issues in India – Health. 24 Nov. 2001
26. Country Health Profile. India: Development of the Health System. 24 Nov. 2001
27. Harvard Medical International. HMI Examples | Health Care Delivery in India. 24 Nov. 2001
28. Perspectives On Health Care In India. 24 Nov. 2001
29. Understanding the Canadian Health Care System. 24 Nov. 2001
30. Medical Device and Diagnostic Industry. India’s Medical Device Market Is Becoming Too Big Ignore. 24 Nov. 2001