Lexall Limited
Introduction
This report records the results of a Certification Audit of a provider of aged residential care services against the Health and Disability Services Standards (NZS8134.1:2008; NZS8134.2:2008 and NZS8134.3:2008).
The audit has been conducted by Health and Disability Auditing New Zealand Limited, an auditing agency designated under section 32 of the Health and Disability Services (Safety) Act 2001, for submission to the Ministry of Health.
The abbreviations used in this report are the same as those specified in section 10 of the Health and Disability Services (General) Standards (NZS8134.0:2008).
You can view a full copy of the standards on the Ministry of Health’s website by clicking here.
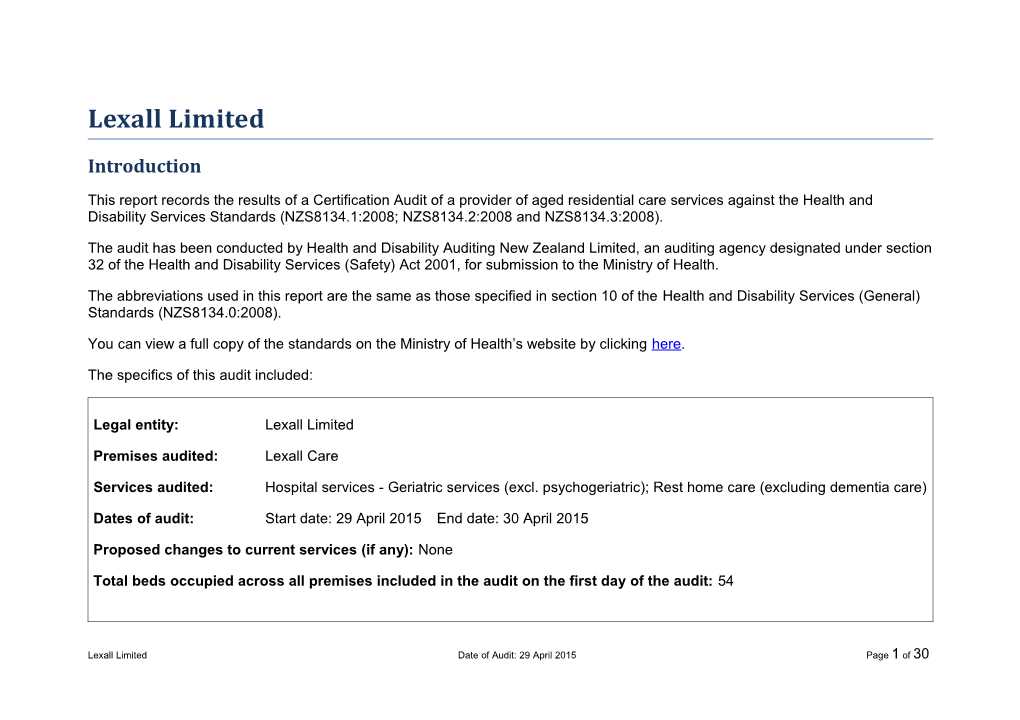
The specifics of this audit included:
Legal entity: Lexall Limited
Premises audited: Lexall Care
Services audited: Hospital services - Geriatric services (excl. psychogeriatric); Rest home care (excluding dementia care)
Dates of audit: Start date: 29 April 2015 End date: 30 April 2015
Proposed changes to current services (if any): None
Total beds occupied across all premises included in the audit on the first day of the audit: 54
Lexall Limited Date of Audit: 29 April 2015 Page 1 of 30 Executive summary of the audit
Introduction
This section contains a summary of the auditors’ findings for this audit. The information is grouped into the six outcome areas contained within the Health and Disability Services Standards:
consumer rights
organisational management
continuum of service delivery (the provision of services)
safe and appropriate environment
restraint minimisation and safe practice
infection prevention and control.
As well as auditors’ written summary, indicators are included that highlight the provider’s attainment against the standards in each of the outcome areas. The following table provides a key to how the indicators are arrived at.
Key to the indicators
Indicator Description Definition Includes commendable elements above the All standards applicable to this service fully attained with required levels of some standards exceeded performance Indicator Description Definition
No short falls Standards applicable to this service fully attained
Some minor shortfalls but no major deficiencies and required levels of Some standards applicable to this service partially performance seem attained and of low risk achievable without extensive extra activity A number of shortfalls Some standards applicable to this service partially that require specific attained and of medium or high risk and/or unattained action to address and of low risk Major shortfalls, significant action is Some standards applicable to this service unattained and needed to achieve the of moderate or high risk required levels of performance
General overview of the audit
Lexall Care provides rest home and hospital care for up to 58 residents. On the day of audit there were 54 residents.
This certification audit was conducted against the relevant Health and Disability Standards and the contract with the District Health Board. The audit process included the review of policies and procedures, the review of residents and staff files, observations, interviews with residents, family, management, staff and a general practitioner.
The facility is governed by a general manager and manager who are supported by an appropriately qualified and experienced clinical manager (registered nurse). Residents and families interviewed spoke positively about the care and services provided.
Lexall Limited Date of Audit: 29 April 2015 Page 3 of 30 Improvements are required around complaints management, residents meetings and surveys, completing the education plan, wound assessment, fridge temperature monitoring, and restraint documentation and monitoring.
Consumer rights Some standards Includes 13 standards that support an outcome where consumers receive safe services of an applicable to this appropriate standard that comply with consumer rights legislation. Services are provided in a service partially manner that is respectful of consumer rights, facilities, informed choice, minimises harm and attained and of low acknowledges cultural and individual values and beliefs. risk.
The staff at Lexall Care ensure that care is provided in a way that focuses on the individual, values, residents' autonomy and maintains their privacy and choice. The service functions in a way that complies with the Health and Disability Commissioner (HDC) Code of Health and Disability Services Consumers' Rights (the Code). Information about the Code and services is easily accessible to residents and families. Information on informed consent is included in the admission agreement and discussed with residents and relatives. Informed consent processes are followed and residents' clinical files reviewed evidence informed consent and advanced directives are documented. A complaints register is maintained.
Organisational management Some standards applicable to this Includes 9 standards that support an outcome where consumers receive services that comply service partially with legislation and are managed in a safe, efficient and effective manner. attained and of low risk. Lexall Care has a quality and risk management system in place that is implemented and monitored, which generates improvements in practice and service delivery. Key components of the quality management system link to relevant facility meetings. The service is active in analysing data to identify trends and areas for improvement. Corrective actions are identified and implemented. Health and safety policies, systems and processes are implemented to manage risk. Incidents and accidents are reported and appropriately managed. There is a comprehensive orientation programme that provides new staff with relevant and specific information for safe work practice. The in-service education programme covers relevant aspects of care and support. The staffing levels provide sufficient and appropriate coverage for the effective delivery of care and support. Staffing is based on the occupancy and acuity of the residents.
Lexall Care has a quality and risk management system in place that is implemented and monitored, which generates improvements in practice and service delivery. Key components of the quality management system link to relevant facility meetings. The service is active in analysing data to identify trends and areas for improvement. Corrective actions are identified and implemented. Health and safety policies, systems and processes are implemented to manage risk. Incidents and accidents are reported and appropriately managed. There is a comprehensive orientation programme that provides new staff with relevant and specific information for safe work practice. The in-service education programme covers relevant aspects of care and support. The staffing levels provide sufficient and appropriate coverage for the effective delivery of care and support. Staffing is based on the occupancy and acuity of the residents.
Continuum of service delivery Some standards Includes 13 standards that support an outcome where consumers participate in and receive applicable to this timely assessment, followed by services that are planned, coordinated, and delivered in a service partially timely and appropriate manner, consistent with current legislation. attained and of low risk.
There is a comprehensive admission procedure. A registered nurse assesses and reviews resident’s needs, outcomes and goals with the resident and/or family. Care plans are developed and demonstrate service integration. Changes to health status and
Lexall Limited Date of Audit: 29 April 2015 Page 5 of 30 interventions required are updated on the care plans to reflect the residents current health status. Resident files include notes by the GP and allied health professionals. Medication policies reflect legislative medicine requirements and guidelines. All staff responsible for administration of medication complete education and competencies. An activities programme is in place. The programme includes outings, entertainment and activities that meet the recreational preferences and abilities of the residents. All food is prepared on site. All residents’ nutritional needs are identified and documented. Choices are available. Meals are well presented and a dietitian has reviewed the menu plans.
Safe and appropriate environment Includes 8 standards that support an outcome where services are provided in a clean, safe Standards applicable environment that is appropriate to the age/needs of the consumer, ensure physical privacy is to this service fully maintained, has adequate space and amenities to facilitate independence, is in a setting attained. appropriate to the consumer group and meets the needs of people with disabilities.
Chemical are stored safely. The building holds a current warrant of fitness. Rooms are spacious and personalised. Communal areas are easily accessed with appropriate seating and furniture to accommodate the needs of residents. External areas are safe and well maintained. There adequate communal showers for the residents that don’t have ensuites. Fixtures, fittings and flooring are appropriate. Cleaning and laundry services are monitored through internal audits. Appropriate training, information and equipment for responding to emergencies have been provided. There is an approved evacuation scheme and emergency supplies for at least three days. Registered nurses hold a current first aid certificate. The temperature of the facility is comfortable. Electrical equipment is checked annually. Hot water temperatures are monitored. Restraint minimisation and safe practice Some standards applicable to this service partially Includes 3 standards that support outcomes where consumers receive and experience attained and of services in the least restrictive and safe manner through restraint minimisation. medium or high risk and/or unattained and of low risk.
There is a restraint policy that includes comprehensive restraint procedures and aligns with the standards. A register is maintained with all residents with restraint or enablers. There were nine residents requiring restraints and two residents using enablers. The service reviews restraint as part of the quality management and staff are trained in restraint minimisation. Not all restraint documentation is completed as per policy.
Infection prevention and control Includes 6 standards that support an outcome which minimises the risk of infection to consumers, service providers and visitors. Infection control policies and procedures are Standards applicable practical, safe and appropriate for the type of service provided and reflect current accepted to this service fully good practice and legislative requirements. The organisation provides relevant education on attained. infection control to all service providers and consumers. Surveillance for infection is carried out as specified in the infection control programme.
Infection control management systems are in place to minimise the risk of infection to consumers, service providers and visitors. Documented policies and procedures are in place for the prevention and control of infection and reflect current accepted good practice and legislative requirements. Infection control education is provided to all service providers as part of their orientation and
Lexall Limited Date of Audit: 29 April 2015 Page 7 of 30 also as part of the on-going in-service education programme. The type of surveillance undertaken is appropriate to the size and complexity of the organisation. Results of surveillance are acted upon, evaluated and reported to relevant personnel.
Infection control management systems are in place to minimise the risk of infection to consumers, service providers and visitors. Documented policies and procedures are in place for the prevention and control of infection and reflect current accepted good practice and legislative requirements. Infection control education is provided to all service providers as part of their orientation and also as part of the on-going in-service education programme. The type of surveillance undertaken is appropriate to the size and complexity of the organisation. Results of surveillance are acted upon, evaluated and reported to relevant personnel.
Summary of attainment
The following table summarises the number of standards and criteria audited and the ratings they were awarded.
Partially Partially Partially Partially Continuous Partially Attained Fully Attained Attained Attained Attained High Attained Critical Attainment Improvement Low Risk Rating (FA) Negligible Risk Moderate Risk Risk Risk (CI) (PA Low) (PA Negligible) (PA Moderate) (PA High) (PA Critical) Standards 0 43 0 6 1 0 0 Criteria 0 94 0 6 1 0 0
Unattained Unattained Low Unattained Unattained High Unattained Attainment Negligible Risk Risk Moderate Risk Risk Critical Risk Rating (UA Negligible) (UA Low) (UA Moderate) (UA High) (UA Critical) Standards 0 0 0 0 0 Criteria 0 0 0 0 0 Attainment against the Health and Disability Services Standards
The following table contains the results of all the standards assessed by the auditors at this audit. Depending on the services they provide, not all standards are relevant to all providers and not all standards are assessed at every audit.
Please note that Standard 1.3.3: Service Provision Requirements has been removed from this report, as it includes information specific to the healthcare of individual residents. Any corrective actions required relating to this standard, as a result of this audit, are retained and displayed in the next section.
For more information on the standards, please click here.
For more information on the different types of audits and what they cover please click here.
Standard with desired outcome Attainment Rating Audit Evidence
Standard 1.1.1: Consumer Rights During Service FA Discussions with staff confirmed their familiarity with the Health and Delivery Disability Commissioner (HDC) Code of Health and Disability Services Consumers’ Rights (the Code). Eight residents (four rest home and four Consumers receive services in accordance with hospital) and four relatives (one rest home and three hospital) were consumer rights legislation. interviewed and confirmed the services being provided are in line with the Code.
Standard 1.1.10: Informed Consent FA Informed consent and advanced directives were recorded as evidenced in the eight resident files reviewed (three rest home and five hospital). Consumers and where appropriate their Advised by staff that family involvement occurs with the consent of the family/whānau of choice are provided with the resident. Residents interviewed confirmed that information was information they need to make informed choices provided to enable informed choices and that they were able to decline and give informed consent. or withdraw their consent. Resident admission agreements were signed.
Lexall Limited Date of Audit: 29 April 2015 Page 9 of 30 Standard 1.1.11: Advocacy And Support FA Contact numbers for advocacy services are included in the policy, in the resident information folder and in advocacy pamphlets that are available Service providers recognise and facilitate the right at reception. Discussions with relatives identified that the service of consumers to advocacy/support persons of their provides opportunities for the family/EPOA to be involved in decisions. choice.
Standard 1.1.12: Links With Family/Whānau And FA Residents and relatives confirmed that visiting can occur at any time. Other Community Resources Key people involved in the resident’s life have been documented in the care plans. Residents and relatives verified that they have been Consumers are able to maintain links with their supported and encouraged to remain involved in the community. family/whānau and their community. Entertainers have been invited to perform at the facility.
Standard 1.1.13: Complaints Management PA Low A complaints policy and procedures have been implemented and residents and their family/whanau have been provided with information The right of the consumer to make a complaint is on admission. Complaint forms are available at the entrance of the understood, respected, and upheld. service. Staff are aware of the complaints process and to whom they should direct complaints. A complaints register has been maintained, however, not all complaints on the register have an accompanying complaints form or evidence of communication, investigation or documentation of resolution as per policy. There are seven documented concerns or complaints received in 2015. There was no evidence of documented response to or follow up in regard to these. Residents and family members advised that they are aware of the complaints procedure and how to access forms.
Standard 1.1.2: Consumer Rights During Service FA The service provides information to residents that include the Code, Delivery complaints and advocacy. Information is given to the family or the enduring power of attorney (EPOA) to read to and/or discuss with the Consumers are informed of their rights. resident. Residents and relatives interviewed identified they are well- informed about the code of rights. Resident meetings and a resident and family survey have not been undertaken in the last two years to provide the opportunity to raise concerns (link# 1.2.3.6). Advocacy and code of rights information is included in the information pack and are available at reception. Standard 1.1.3: Independence, Personal Privacy, FA Staff interviewed were able to describe the procedures for maintaining Dignity, And Respect confidentiality of resident records, resident’s privacy and dignity. House rules and a code of conduct are signed by staff at commencement of Consumers are treated with respect and receive employment. services in a manner that has regard for their Interdenominational church services are held every second Thursday as dignity, privacy, and independence. well as a Catholic service on a Sunday and a Korean Catholic service on the first Thursday of the month. Resident files include cultural and spiritual values. Contact details of spiritual/religious advisors are available to staff. Residents and relatives interviewed reported that residents are able to choose to engage in activities and access community resources. There is an elder abuse and neglect policy and staff education and training on abuse and neglect has been provided.
Standard 1.1.4: Recognition Of Māori Values And FA The service has a Maori heath plan and an individual’s values and Beliefs beliefs policy which includes cultural safety and awareness. Discussions with staff confirmed their understanding of the different Consumers who identify as Māori have their health cultural needs of residents and their whānau. There was one resident at and disability needs met in a manner that respects Lexall Care who identifies as Maori at the time of the audit. The service and acknowledges their individual and cultural, has established links with local Maori and staff confirmed they are values and beliefs. aware of the need to respond appropriately to maintain cultural safety.
Standard 1.1.6: Recognition And Respect Of The FA Care planning includes consideration of spiritual, psychological and Individual's Culture, Values, And Beliefs social needs. Residents interviewed indicated that they are asked to identify any spiritual, religious and/or cultural beliefs. The facility had Consumers receive culturally safe services which ten Korean and one Chinese resident at the time of audit, interpreters recognise and respect their ethnic, cultural, are available and the residents specific cultural needs are identified. spiritual values, and beliefs. Relatives reported that they feel they are consulted and kept informed and family involvement is encouraged.
Standard 1.1.7: Discrimination FA The staff employment process includes the signing of house rules and a service code of conduct. Job descriptions include responsibilities of the Consumers are free from any discrimination, position and ethics, advocacy and legal issues. The orientation coercion, harassment, sexual, financial, or other programme provided to staff on induction includes an emphasis on exploitation.
Lexall Limited Date of Audit: 29 April 2015 Page 11 of 30 dignity and privacy and boundaries. Registered nursing staff have completed training around professional boundaries.
Standard 1.1.8: Good Practice FA The quality programme has been designed to monitor contractual and Consumers receive services of an appropriate standards compliance and the quality of service delivery in the facility. standard. Staffing policies include pre-employment, and the requirement to attend orientation and on-going in-service training. The Clinical Manager is responsible for coordinating the internal audit programme. A variety of staff meetings are conducted. Residents and relatives interviewed spoke very positively about the care and support provided. Staff have a sound understanding of principles of aged care and state that they feel supported by the nurse manager. Care staff complete competencies relevant to their practice.
Standard 1.1.9: Communication FA Residents and family members interviewed stated they are informed of changes in health status and incidents/accidents. Residents and family Service providers communicate effectively with members also stated they were welcomed on entry and were given time consumers and provide an environment conducive and explanation about services and procedures. Resident/relative to effective communication. meetings had not occurred for two years (link#1.2.3.6). The managers have an open-door policy. Residents and family are advised in writing of their eligibility and the process to become a subsidised resident should they wish to do so. The service has policies and procedures available for access to interpreter services for residents (and their family/whānau). If residents or family/whanau have difficulty with written or spoken English the interpreter services are made available.
Standard 1.2.1: Governance FA Lexall Care is privately owned and managed by the owners (general manager and manager) who are supported by a full time clinical The governing body of the organisation ensures manager (RN). The service provides care for up to 58 residents at services are planned, coordinated, and hospital and rest home level care. On the day of the audit, there were appropriate to the needs of consumers. 54 residents in total (21 residents at rest home level, including one respite and 33 residents at hospital level including one receiving interim care). The experienced clinical manager has been in the role for two years since the hospital opened and was previously the nurse manager of the facility for 14 years. The current strategic plan and quality and risk management plans are being implemented. The service has a long term goal to gain resource consent to extend additional 55 beds. Advised, that this is a 2-3 year plan.
Standard 1.2.2: Service Management FA The clinical manager covers any absence of the manager and general manager. A charge nurse covers any clinical manager absence. The organisation ensures the day-to-day operation of the service is managed in an efficient and effective manner which ensures the provision of timely, appropriate, and safe services to consumers.
Standard 1.2.3: Quality And Risk Management PA Low The quality manual and the business, quality, risk and management Systems planning procedure describe the Lexall Care’s quality improvement processes. The risk management plan describes objectives, The organisation has an established, documented, management controls and assigned responsibility. Progress with the and maintained quality and risk management quality and risk management programme is being monitored through the system that reflects continuous quality quality improvement meeting, and the various facility meetings. Monthly improvement principles. and annual reviews have been completed for all areas of service. Meeting minutes have been maintained and staff were expected to read the minutes and sign off when read. Minutes for all meetings have included actions to achieve compliance where relevant. Discussions with registered nurses and care workers confirmed their involvement in the quality programme. Resident/relative meetings have not been held for two years. Resident satisfaction surveys to gather feedback on the service provided have not been undertaken for two years. Data is collected on complaints, accidents, incidents, infection control and restraint use. The internal audit schedule for 2014 has been completed. Areas of non-compliance identified at audits have been actioned for improvement. Specific quality improvements have been identified. The service has implemented a health and safety management system. There are implemented risk management, and health and safety policies and procedures in place including accident and hazard management. The service has comprehensive policies/ procedures to support service delivery. Policies and procedures align with the client care plans. A document control policy outlines the system implemented whereby all
Lexall Limited Date of Audit: 29 April 2015 Page 13 of 30 policies and procedures are reviewed regularly. Falls prevention strategies are implemented for individual residents.
Standard 1.2.4: Adverse Event Reporting FA Incident and accident data has been collected and analysed. Discussions with the service confirmed that there is an awareness of the All adverse, unplanned, or untoward events are requirement to notify relevant authorities in relation to essential systematically recorded by the service and notifications. A sample of resident related incident forms for April 2015 reported to affected consumers and where were reviewed. All forms and corresponding resident files reviewed appropriate their family/whānau of choice in an evidence that appropriate clinical care has been provided following an open manner. incident. The incident reporting policy includes definitions, and outlines responsibilities including immediate action, reporting, monitoring and corrective action to minimise and debriefing. The service benchmarks incident data with other facilities.
Standard 1.2.7: Human Resource Management PA Low The recruitment and staff selection process requires that relevant checks have been completed to validate the individual’s qualifications, Human resource management processes are experience and veracity. A copy of practising certificates are kept. Nine conducted in accordance with good employment staff files were reviewed and included all appropriate documentation. practice and meet the requirements of legislation. Staff turnover was reported as low, with some staff having been employed since the facility opened 15 years ago. The service has a comprehensive orientation programme that provides new staff with relevant information for safe work practice. Staff interviewed were able to describe the orientation process and stated that they believed new staff were adequately orientated to the service. Care workers are orientated by ‘preceptors’. Annual appraisals are conducted for all staff. The in-service calendar for 2013-14 was not fully completed. Care workers have completed either the national certificate in care of the elderly or have completed or commenced an aged care education programme. The clinical manager and registered nurses attend external training including conferences, seminars and education sessions with the local DHB.
Standard 1.2.8: Service Provider Availability FA Lexall Care has a four weekly roster in place which provides sufficient staffing cover for the provision of care and service to residents. There is Consumers receive timely, appropriate, and safe at least one registered nurse on duty at all times. The full time clinical service from suitably qualified/skilled and/or manager is also a registered nurse. Caregivers and residents and experienced service providers. family interviewed advised that sufficient staff are rostered on for each shift. All registered nurses have been trained in first aid and CPR.
Standard 1.2.9: Consumer Information FA The resident files are appropriate to the service type. Residents Management Systems entering the service have all relevant initial information recorded within 24 hours of entry into the resident’s individual record. Residents' files Consumer information is uniquely identifiable, are protected from unauthorised access by being locked away in the accurately recorded, current, confidential, and nurses’ stations. Information containing sensitive resident information accessible when required. are not displayed in a way that can be viewed by other residents or members of the public. Record entries are legible, dated and signed by the relevant staff member. Individual resident files demonstrate service integration. Medication charts have been stored in a separate folder. Archived records are stored securely on site.
Standard 1.3.1: Entry To Services FA The service has information for potential residents and information which they give to residents on admission. This information includes all Consumers' entry into services is facilitated in a relevant aspects of the service and residents and family/whanau are competent, equitable, timely, and respectful provided with associated information such as the Health and Disability manner, when their need for services has been Code of Rights and how to access advocacy. All potential admissions identified. are checked to ensure they have a completed needs assessment and the service can provide the level of care. The two charge nurses interviewed stated that there is good liaison and communication with needs assessors, social workers, mental health team and general practitioners and nurse practitioners. There is an admission policy and procedure. The service has recently reviewed and updated their admission agreement and this aligns with a) - k) of the ARC contract. The eight admission agreements sighted had all been signed within the required time frame.
Standard 1.3.10: Transition, Exit, Discharge, Or FA There is a policy and procedure for death, discharge and transfer. Transfer When transferring all relevant documentation is written on a transfer form accompanied with medication sheets and recent GP notes.
Lexall Limited Date of Audit: 29 April 2015 Page 15 of 30 Consumers experience a planned and coordinated Resident transfer information is communicated to the receiving health transition, exit, discharge, or transfer from provider or service. There is documented family notification of services. appointments and transfers. Relatives interviewed stated they were kept informed of the resident’s condition.
Standard 1.3.12: Medicine Management PA Low Medications are managed appropriately in line with accepted guidelines. Registered nurses administer medications, at times senior medication Consumers receive medicines in a safe and timely competent caregivers administer medications under RN direction. All manner that complies with current legislative staff administering medications have completed an annual medication requirements and safe practice guidelines. competency. The service uses a robotic roll system for medications. All medications are checked on delivery against the medication chart and any discrepancies are fed back to the supplying pharmacy. There is a small stock of hospital stock kept in a locked cupboard in the medication room. Medication fridges do not have their temperature monitored. All controlled drugs are checked weekly. Self-medication residents are managed in line with accepted guidelines. The sixteen medication charts sampled included photo ID and allergies. The charts were clear and charted correctly. The signing sheets corresponded to the medication chart. All medication charts sampled showed evidence of being reviewed by the GP three monthly. Standing orders complied with accepted guidelines.
Standard 1.3.13: Nutrition, Safe Food, And Fluid FA All food is cooked on site in the main kitchen. The food is transported to Management dining rooms in bain maries. The temperature of the food is checked before leaving the kitchen. There are two cooks who rotate shifts. They A consumer's individual food, fluids and nutritional are supported by a kitchen hand. Both cooks have a current food safety needs are met where this service is a component and hygiene certificate. The kitchen hand has completed food safety of service delivery. and hygiene in-service. There is a kitchen manual and cleaning schedule. There are seasonal menus on a four weekly cycle and these have been approved by a consultant dietitian. The cooks receive dietary information for new residents and are notified of any dietary changes, weight loss or other dietary requirements. Special diets and allergies are on laminated notices on the fridge door. Normal and moulied meals are provided. On a Friday, the Korean residents receive a Korean meal. Fridge and freezer temperatures are recorded daily. Temperatures are recorded on all chilled and frozen deliveries. All food in the chiller, fridges and freezers are dated. There is sufficient food stored to last for at least three days in an emergency. Stock is rotated by date. The kitchen is well equipped, clean and tidy. Residents and relatives interviewed said the food was mainly satisfactory. No evidence of resident satisfaction surveys since 2013 (link1.2.3.6).
Standard 1.3.2: Declining Referral/Entry To FA The service records the reason (no bed available or unable to meet the Services acuity/level of care) for declining admission to the service. Potential residents are referred back to the referring agency if declined. Where referral/entry to the service is declined, the immediate risk to the consumer and/or their family/whānau is managed by the organisation, where appropriate.
Standard 1.3.4: Assessment FA Files reviewed identified that falls risk, pressure area risk, nutritional, continence, patient handling and activities assessments were completed Consumers' needs, support requirements, and on admission. Pain and challenging behaviours assessments were preferences are gathered and recorded in a timely completed as required. The outcomes of risk assessments were manner. reflected in the eight care plans sampled and interventions identify required support. However restraint assessments were not undertaken prior to commencement (link 2.2.2.1)
Standard 1.3.5: Planning FA Care plans reviewed were comprehensive and demonstrated service integration with input from allied staff. The exception to this was Consumers' service delivery plans are consumer restraint where care plans did not detail what restraint/enabler is used focused, integrated, and promote continuity of and the associated risks or minimisation strategies (link 2.2.3.4). service delivery. Residents interviewed confirm care delivery and support by staff is consistent. There is documented evidence on the care plan and in the family contact notes of family involvement in the care plan process. Acute care plans are in use for short term needs and changes in health.
Lexall Limited Date of Audit: 29 April 2015 Page 17 of 30 Standard 1.3.6: Service Delivery/Interventions PA Low The long term care plan is readily available for caregivers. When a resident’s health status changes the registered nurse will review the Consumers receive adequate and appropriate resident and if required will ask the GP or other health professionals for services in order to meet their assessed needs a consultation. There is documented evidence on the family contact and desired outcomes. sheet of family notification when a resident’s health status changes. All relatives interviewed stated that staff were approachable if they needed to discuss their relative’s health at any time. Dressing supplies are available and dressing trolleys were well stocked in each treatment room. Continence products are available and it is recorded in the care plans reviewed which product is needed and when. Wound assessments reviewed were incomplete. However, there were explicit guidelines for staff including diagrams in wound care plans. There is GP involvement in wound care as necessary and for one pressure area on an ankle there is wound care specialist involvement. Acute care plans are in place. Monitoring forms are in use as directed by the registered nurses. Restraint monitoring is incomplete (link 2.2.2)
Standard 1.3.7: Planned Activities FA There is one qualified diversional therapist who works 33 hours from Monday to Saturday. The monthly activity programme is displayed on Where specified as part of the service delivery noticeboards. The theme of the month at the time of audit was Kiwiana. plan for a consumer, activity requirements are There is a range of activities to meet most needs including appropriate to their needs, age, culture, and the entertainment, bingo, bowls, craft and games. Community groups such setting of the service. as choirs visit frequently. Group exercises are held daily and the physiotherapist has input into these. There is a van outing every Friday. The van is hired. Church services are held every second Thursday. There is a Catholic service on a Sunday and a Korean Catholic service on the first Thursday of the month. The diversional therapist states that the programme changes according to the mix of residents. Variations to the programme are notified to the residents. The diversional therapist has one on one time with residents who are unable or who choose not to participate in the programme. On the days of audit activities were seen to be taking place and most residents were actively engaged. Special occasions and birthdays are celebrated, for example Anzac Day. All residents are encouraged to participate. The diversional therapist completes an individual activity plan on admission which includes previous hobbies, community links, family and interests. Residents feedback on activities to the diversional therapist and changes are made as required.
Standard 1.3.8: Evaluation FA Care plan evaluations reviewed were documented by the registered nurses six monthly or as necessary. There were acute care plans Consumers' service delivery plans are evaluated in available to focus on acute and short term issues. These were a comprehensive and timely manner. evaluated regularly. The GP completes three monthly reviews including medications. Family are invited to attend and have input into the reviews.
Standard 1.3.9: Referral To Other Health And FA Referral to other health and disability services was evident in the sample Disability Services (Internal And External) group of resident files. The service facilitates access to other medical and non-medical services. Referral documentation was maintained on Consumer support for access or referral to other resident files. Examples of referrals sighted were to dietitian, wound health and/or disability service providers is care specialist and mental health services. appropriately facilitated, or provided to meet consumer choice/needs. Discussions with registered nurses identified that the service has access to GP’s, ambulance/emergency services, allied health, dietitian, wound specialists and social workers.
Standard 1.4.1: Management Of Waste And FA There is a waste and hazardous substance safety policy. Management Hazardous Substances of waste and hazardous substances is covered during orientation. Chemical safety training has not been completed in the last year (link Consumers, visitors, and service providers are 1.2.7.5). All chemicals are stored in locked cupboards. Safety data protected from harm as a result of exposure to sheets and product wall charts are available. Approved sharps waste, infectious or hazardous substances, containers are used. These are easily identifiable. Gloves, aprons and generated during service delivery. face shields are available for staff use and staff were observed wearing appropriate protective equipment when carrying out their duties.
Standard 1.4.2: Facility Specifications FA The building holds a current warrant of fitness. Reactive and preventative maintenance occurs. There are two maintenance people Consumers are provided with an appropriate, on staff who are also responsible for the garden. Outside contractors
Lexall Limited Date of Audit: 29 April 2015 Page 19 of 30 accessible physical environment and facilities that check and calibrate medical equipment annually and hoist six monthly. are fit for their purpose. Hot water temperatures are monitored and recorded. They are maintained between 43-45 degrees Celsius. There are contractors for essential services available and on call. Electrical testing and tagging has been completed April, 2015. The living areas are carpeted and vinyl surfaces exist in bathrooms/toilets. The corridors are very wide in the new area and adequate in the old area. There are handrails in all corridors which promotes safe mobility. Residents were observed moving freely around the areas with mobility aids if required. The external areas and gardens are well maintained and easily accessible (including wheelchairs). There is outdoor furniture and seating and shaded areas. There is a large picture window in one of the lounges and residents were observed enjoying the view. The registered nurses interviewed stated that they have all the equipment referred to in care plans necessary to provide care.
Standard 1.4.3: Toilet, Shower, And Bathing FA All resident rooms in the new area have ensuites. In the old area there Facilities are toilets and hand basins in each room and adequate numbers of communal shower rooms. There is appropriate signage, easy clean Consumers are provided with adequate flooring and fixtures and handrails appropriately placed. Shower rooms toilet/shower/bathing facilities. Consumers are are private. The residents interviewed reported that privacy is assured privacy when attending to personal maintained at all times. hygiene requirements or receiving assistance with personal hygiene requirements.
Standard 1.4.4: Personal Space/Bed Areas FA There is one double room which has a dividing wall down the middle. The rest of the rooms are single. All rooms are spacious and it is easy Consumers are provided with adequate personal for staff to manoeuvre transferring and mobility equipment to safely space/bed areas appropriate to the consumer deliver care. Residents are encouraged to personalise their rooms. group and setting.
Standard 1.4.5: Communal Areas For FA There are spacious lounges in each area and there are also smaller Entertainment, Recreation, And Dining areas where residents can sit alone or in small groups. Each area has a dining room. There is a café with tea/coffee making facilities for staff Consumers are provided with safe, adequate, age and residents. All lounge/dining areas are accessible and appropriate, and accessible areas to meet their accommodate the equipment required for the residents. Residents are relaxation, activity, and dining needs. able to move freely and furniture is arranged to facilitate this. The lounges/dining rooms can accommodate lounge chairs. There is adequate space to allow maximum freedom of movement while promoting safety for those that wander.
Standard 1.4.6: Cleaning And Laundry Services FA There is a cleaning policy and cleaning schedules in place. There is a laundry policy and schedule. Only personal washing is done on site. All Consumers are provided with safe and hygienic chemicals are labelled. Personal protective equipment is available and cleaning and laundry services appropriate to the easily accessible for cleaners and laundry staff. Cleaning trolleys are setting in which the service is being provided. locked in cupboards when not in use or have all chemicals removed from them. Safety data sheets are in the sluice rooms, chemical storage cupboard, cleaner’s cupboard and laundry. Cleaning and laundry staff were observed wearing appropriate protective wear when carrying out their duties. Cleaning of carpets is carried out as required. There were adequate linen supplies sighted. Linen is washed off site.
Standard 1.4.7: Essential, Emergency, And FA Appropriate training information and equipment for responding to Security Systems emergencies is provided. All registered nurses have a current first aid certificate. There is an approved fire evacuation scheme. Fire Consumers receive an appropriate and timely evacuations are held six monthly. There is a civil defence and response during emergency and security emergency policy and procedure in place. The facility has an situations. emergency civil defence kit – kept in the upstairs treatment room and maintained by the registered nurses. There is a spills kit. The facility has emergency lighting. There are gas barbeques that can be used for cooking. Emergency food supplies sufficient for three days are kept in the kitchen. There are extra blankets available. There are sufficient stocks of continence products and personal protective equipment. In the event of a power failure residents on oxygen concentrators can be switched to oxygen cylinders and there are back up batteries and torches. The call bell system operates in all areas. Staff ensure the building is secure overnight. Reception monitors visitor entry by day.
Standard 1.4.8: Natural Light, Ventilation, And FA All communal rooms and resident rooms are well ventilated and light.
Lexall Limited Date of Audit: 29 April 2015 Page 21 of 30 Heating The temperature of the facility is comfortable and can be increased or decreased as necessary. All resident rooms have external windows that Consumers are provided with adequate natural let in natural light. light, safe ventilation, and an environment that is maintained at a safe and comfortable temperature.
Standard 3.1: Infection control management FA Lexall Care has an established infection control (IC) programme. The infection control programme has been appropriate for the size, There is a managed environment, which minimises complexity and degree of risk associated with the service and has been the risk of infection to consumers, service linked into the incident reporting system. A registered nurse has been providers, and visitors. This shall be appropriate to appointed as the designated infection control officer with support from the size and scope of the service. the clinical manager (infection control co-ordinator). The IC matters are reviewed at facility quality meetings. Minutes are available for staff. Regular audits have been conducted and education has been provided for staff. The infection control programme has been reviewed annually.
Standard 3.2: Implementing the infection control FA There are adequate resources to implement the infection control programme programme at Lexall Care. The infection control co-ordinator has maintained her practice by attending infection control updates. The There are adequate human, physical, and infection control team is representative of the facility. External information resources to implement the infection resources and support are available when required. Infection control programme and meet the needs of the prevention and control is part of staff orientation and induction. Hand organisation. washing facilities are available throughout the facility and alcohol hand gel is freely available.
Standard 3.3: Policies and procedures FA The infection control manual outlines a comprehensive range of policies, standards and guidelines and includes roles, responsibilities, Documented policies and procedures for the procedures, the infection control team and training and education of prevention and control of infection reflect current staff. The policies are reviewed and updated at least two yearly. accepted good practice and relevant legislative requirements and are readily available and are implemented in the organisation. These policies and procedures are practical, safe, and appropriate/suitable for the type of service provided.
Standard 3.4: Education FA The facility is committed to the on-going education of staff and residents. Education is facilitated by the infection control nurse with The organisation provides relevant education on support from the infection control officer. All infection control training infection control to all service providers, support has been documented and a record of attendance has been maintained. staff, and consumers. Visitors are advised of any outbreaks of infection and were advised not to attend until the outbreak had been resolved. Information was provided to residents and visitors that are appropriate to their needs and this was documented in medical records. Education around infection prevention and control has been provided in 2014.
Standard 3.5: Surveillance FA Infection surveillance and monitoring is an integral part of the infection control programme and is described in infection monitoring policy. The Surveillance for infection is carried out in clinical manager is the infection control co-ordinator and is supported by accordance with agreed objectives, priorities, and a registered nurse who is the infection control officer. Monthly infection methods that have been specified in the infection data is collected for all infections based on signs and symptoms of control programme. infection. Individual resident infection forms are completed which includes signs and symptoms of infection, treatment, follow up, review and resolution. Surveillance of all infections is entered on to a monthly facility infection summary and staff were informed. The data has been monitored and evaluated monthly and annually. An outbreak of norovirus in February 2014 affecting 17 residents was appropriately managed, with notification to the relevant authority.
Standard 2.1.1: Restraint minimisation FA The service is committed to restraint minimisation and safe practice. Restraint minimisation is overseen by a restraint coordinator who is the Services demonstrate that the use of restraint is clinical manager. There were nine residents requiring bedrails as actively minimised. restraint and one of these also utilises a lap belt when in a wheelchair. Two hospital residents were using bedrails as enablers. The use of enablers is voluntary, requested by the resident. A full restraint assessment is required to be completed prior to implementing the enablers (link 2.2.2.1). There is evidence of the residents consenting to the enabler. In addition, there is evidence of monitoring of residents who were using enablers.
Standard 2.2.1: Restraint approval and processes FA The restraint coordinator is the clinical manager (registered nurse). Assessment and approval process for a restraint intervention included
Lexall Limited Date of Audit: 29 April 2015 Page 23 of 30 Services maintain a process for determining the restraint coordinator, registered nurse, resident/or representative approval of all types of restraint used, restraint and medical practitioner processes (including policy and procedure), duration of restraint, and ongoing education on restraint use and this process is made known to service providers and others.
Standard 2.2.2: Assessment PA Low The service has a policy that directs staff to complete comprehensive assessments for residents who require restraint or enabler interventions. Services shall ensure rigorous assessment of These are undertaken by suitably qualified and skilled staff in consumers is undertaken, where indicated, in partnership with the family/whanau. The restraint coordinator, restraint relation to use of restraint. officer, the resident and/or their representative and a medical practitioner are involved in the assessment and consent process. In the four files reviewed (two restraint and two enabler), assessments were not fully completed. Consent for the use of restraint was completed with family/whanau involvement and a specific consent for enabler / restraint form was used to document approval.
Standard 2.2.3: Safe Restraint Use PA Moderate The restraint minimisation manual identified that restraint is only put in place where it was clinically indicated and justified and approval Services use restraint safely processes. There is an assessment form/process that is to be completed for all restraints and enablers. The four care plans reviewed did not detail that a restraint or enabler was in use or the associated risks/minimisation strategies. Monitoring forms were in use but these did not evidence the two hourly monitoring reported by staff, the monitoring forms had times the restraint/enabler was put on and off only. The files reviewed had a consent form detailing the reason for restraint/enabler and the restraint/enabler to be used. The service has a restraint and enablers register which is updated each month.
Standard 2.2.4: Evaluation FA The service has documented evaluation of restraint every three months. In the files reviewed, evaluations had been completed with the resident, Services evaluate all episodes of restraint. family/whanau, restraint co-ordinator and medical practitioner. Restraint practices are reviewed on a formal basis every month by the facility restraint co-ordinator at quality and staff meetings meeting. Evaluation timeframes are determined by risk levels.
Standard 2.2.5: Restraint Monitoring and Quality FA The service actively reviews restraint as part of the internal audit and Review reporting cycle. Reviews are completed three monthly or sooner if a need is identified by the restraint co-ordinator. Any adverse outcomes Services demonstrate the monitoring and quality are included in the restraint co-ordinators monthly reports and are review of their use of restraint. reported at the monthly meetings. There are six monthly restraint meetings held.
Lexall Limited Date of Audit: 29 April 2015 Page 25 of 30 Specific results for criterion where corrective actions are required
Where a standard is rated partially attained (PA) or unattained (UA) specific corrective actions are recorded under the relevant criteria for the standard. The following table contains the criterion where corrective actions have been recorded.
Criterion can be linked to the relevant standard by looking at the code. For example, a Criterion 1.1.1.1: Service providers demonstrate knowledge and understanding of consumer rights and obligations, and incorporate them as part of their everyday practice relates to Standard 1.1.1: Consumer Rights During Service Delivery in Outcome 1.1: Consumer Rights.
If there is a message “no data to display” instead of a table, then no corrective actions were required as a result of this audit.
Criterion with desired outcome Attainment Audit Evidence Audit Finding Corrective action required Rating and timeframe for completion (days)
Criterion 1.1.13.3 PA Low A complaints register is in place and There was no documentation Ensure all complaints completed for all concerns and on file to support registered in the complaint An up-to-date complaints register is complaints. acknowledgement, log include documentation to maintained that includes all complaints, investigation or follow up of support follow up action. dates, and actions taken. complaints.
90 days
Criterion 1.2.3.6 PA Low The quality manual and the There was no evidence of Ensure satisfaction surveys business, quality, risk and resident meetings or and resident meetings are Quality improvement data are management planning procedure satisfaction surveys being undertaken to gather collected, analysed, and evaluated and describe the Lexall Care’s quality undertaken in the last two feedback on the service the results communicated to service improvement processes. The risk years. provided. providers and, where appropriate, management plan describes consumers. objectives, management controls and assigned responsibility. 90 days Progress with the quality and risk management programme has been monitored through the quality improvement meeting, and the various facility meetings
Criterion 1.2.7.5 PA Low An education plan is in place to The education plan for 2013- Ensure the education plan is ensure staff receive compulsory 2014 was not fully completed as per schedule A system to identify, plan, facilitate, education sessions as well as other completed. Cultural, and all compulsory training is and record ongoing education for relevant training to enable them to continence, sexuality and undertaken by staff. service providers to provide safe and care for the residents in the service. intimacy and chemical safety effective services to consumers. training have not been provided in the last two 90 days years.
Criterion 1.3.12.1 PA Low All medications are prescribed Temperatures of medication Ensure temperatures of the correctly. Robotic medications are fridges were not being medication fridges are A medicines management system is checked on arrival and any monitored or documented. monitored and recorded implemented to manage the safe and pharmacy errors recorded and fed appropriate prescribing, dispensing, back to the supplying pharmacy. administration, review, storage, The two medication rooms were 60 days disposal, and medicine reconciliation in checked. No medication fridges are order to comply with legislation, having temperatures recorded. protocols, and guidelines. Staff sign for the administration of medications on medication sheets held with the prescribing sheet. Signing sheets correspond to instructions on the medication chart and all charts sampled evidenced that medication had been signed for. There is a list of specimen signatures in each medication area.
Criterion 1.3.6.1 PA Low Wound assessments and wound Wound assessments Ensure wound assessment care plans were developed for all reviewed were incomplete documentation is fully The provision of services and/or wounds. Interventions and with no description of the
Lexall Limited Date of Audit: 29 April 2015 Page 27 of 30 interventions are consistent with, and evaluations were well documented. wound, no skin tear category completed for all wounds. contribute to, meeting the consumers' There were explicit guidelines for stated and in some assessed needs, and desired staff including diagrams. incidences no wound site outcomes. stated. 60 days
Criterion 2.2.2.1 PA Low The service has a policy that directs The four files reviewed (two Ensure assessments are staff to complete comprehensive restraint and two enablers), completed In assessing whether restraint will be assessments for residents who assessments were not fully used, appropriate factors are taken into require restraint or enabler completed. consideration by a suitably skilled interventions. 90 days service provider. This shall include but is not limited to: (a) Any risks related to the use of restraint; (b) Any underlying causes for the relevant behaviour or condition if known; (c) Existing advance directives the consumer may have made; (d) Whether the consumer has been restrained in the past and, if so, an evaluation of these episodes; (e) Any history of trauma or abuse, which may have involved the consumer being held against their will; (f) Maintaining culturally safe practice; (g) Desired outcome and criteria for ending restraint (which should be made explicit and, as much as practicable, made clear to the consumer); (h) Possible alternative intervention/strategies.
Criterion 2.2.3.4 PA A restraint register is completed for The four care plans reviewed Ensure all restraint Each episode of restraint is Moderate all restraint use and is current. did not detail that a restraint documentation is completed documented in sufficient detail to Documentation is available to or enabler was in use or the within set timeframes. provide an accurate account of the ensure all restraints and enablers associated risks/minimisation indication for use, intervention, are minimised, consented, detailed strategies. Monitoring was duration, its outcome, and shall include on the care plan, monitored and not documented as 60 days but is not limited to: evaluated. undertaken two hourly as per (a) Details of the reasons for initiating policy. the restraint, including the desired outcome; (b) Details of alternative interventions (including de-escalation techniques where applicable) that were attempted or considered prior to the use of restraint; (c) Details of any advocacy/support offered, provided or facilitated; (d) The outcome of the restraint; (e) Any injury to any person as a result of the use of restraint; (f) Observations and monitoring of the consumer during the restraint; (g) Comments resulting from the evaluation of the restraint.
Lexall Limited Date of Audit: 29 April 2015 Page 29 of 30 Specific results for criterion where a continuous improvement has been recorded
As well as whole standards, individual criterion within a standard can also be rated as having a continuous improvement. A continuous improvement means that the provider can demonstrate achievement beyond the level required for full attainment. The following table contains the criterion where the provider has been rated as having made corrective actions have been recorded.
As above, criterion can be linked to the relevant standard by looking at the code. For example, a Criterion 1.1.1.1 relates to Standard 1.1.1: Consumer Rights During Service Delivery in Outcome 1.1: Consumer Rights
If, instead of a table, these is a message “no data to display” then no continuous improvements were recorded as part of this of this audit.
No data to display
End of the report.