Globalizing Leprosy
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

January 26, 2020 Towards a Leprosy-Free Country
China CDC Weekly Announcements Preplanned Studies The 67th World Leprosy Day Towards a Leprosy-Free — January 26, 2020 Country — China, 2011−2018 1,# 1 1 Meiwen Yu ; Peiwen Sun ; Le Wang ; Hongsheng World Leprosy Day was proposed by French Wang1; Heng Gu1; Xiangsheng Chen1 humanitarian Raoul Follereau in 1954 (1) and has been annually observed around the world on the last Sunday of each January with the aim of raising Summary global awareness and knowledge about this What is already known about this topic? ancient disease and calling attention to the fact Leprosy is a chronic infectious disease that is endemic that leprosy can be prevented, treated, and cured. in several countries. Control of leprosy has had targets Since 1988, the China Leprosy Association set by World Health Organization’s (WHO) Global initiated China Leprosy Day on the same day. Strategy 2016–2020 and by China through a national Although leprosy has been declared leprosy-control plan (2011–2020). “eliminated” as a public health problem at a global What is added by this report? level by the World Health Organization (WHO) Data from the Leprosy Management Information in 2005, around 200,000 new cases are reported System in China was analyzed and showed a national globally each year (2). In 2011, the Chinese prevalence of 0.178 per 100,000 and detection rate of Ministry of Health, together with 11 other 0.037 per 100,000 residents in 2018. In addition, all ministries, implemented the “National Strategic the main targets for 2020 have been met by 2018 Plan for Eliminating Harm of Leprosy, except for the proportion of counties or cities to reach a 2011–2020 in China”, aiming to reduce both the prevalence of less than 1/100,000 and the proportion rate of grade 2 disability (G2D) and severe adverse of children cases with grade 2 disability (G2D). -

550 Leprosy in China: a History. by Angela Ki-Che Leung. New York
550 Book Reviews / T’oung Pao 96 (2011) 543-585 Leprosy in China: A History. By Angela Ki-che Leung. New York: Columbia Uni- versity Press, 2009. 373 pp. Index, bibliography, ill. Angela Leung’s new book adds a very important case study that historicizes the recent “modernist” works on the history of public health in China by Ruth Rogaski,1 Carol Benedict,2 and Kerrie Macpherson.3 Unlike the above three works, which all focus on “modernity” and have rightly been well-received, Leung presents a highly original, postcolonial history of leprosy in China, which was known in antiquity as li/lai, wind-induced skin ailments, or mafeng, “numb skin.” ese symptoms were subsequently combined during the Song dynasty into a single etiology of skin ailments , i.e., dafeng/lai. Leung’s pioneering account successfully provincializes the European narrative of leprosy and public health by presenting: 1) the longer historical memory of “leprosy” in China since antiquity; 2) the important public health changes that occurred during the Song dynasty (960-1280); and 3) how the skin illnesses we call leprosy were reconceptualized during the Ming and Qing dynasties. Leung then concludes her manuscript with two fi nal chapters that successfully parallel but revise the accounts in Rogaski, Benedict, and Macpherson. Leung describes Chinese political eff orts since the nineteenth century to develop not simply a “modern” and “Western” medical regime but a “hybrid,” Sino-Western public health system to deal with the disease. e book reveals overall the centrality of China in the history of the leprosy, and it shows how leprosy played out as a global threat, which provides lessons for dealing with AIDS, SARS, and bird viruses today. -

Epidemiological Scenario of Leprosy in a Province in China: Long Delay in Diagnosis and High Rate of Deformity
Epidemiological Scenario of Leprosy in a Province in China: Long Delay in Diagnosis and High Rate of Deformity. Ge Li Shaanxi Provincial Institute for Endemic Disease Control Qing-Ping Zhang Shaanxi Provincial Institute for Endemic Disease Control Zhao-Xing Lin Shaanxi Provincial Institute for Endemic Disease Control Ping Chen Shaanxi Provincial Institute for Endemic Disease Control Chao Li ( [email protected] ) Fourth Military Medical University https://orcid.org/0000-0002-6175-5701 Research article Keywords: Leprosy, Mycobacterium leprae, China, Epidemiology Posted Date: June 24th, 2020 DOI: https://doi.org/10.21203/rs.3.rs-34383/v1 License: This work is licensed under a Creative Commons Attribution 4.0 International License. Read Full License Version of Record: A version of this preprint was published on November 25th, 2020. See the published version at https://doi.org/10.1186/s12889-020-09933-6. Page 1/11 Abstract Background: This ecological study aimed to analyze both the tendency and the characteristics of leprosy in an endemic province in the Chinese Northwest. Methods: The medical records of leprosy in the province of Shaanxi, China, 1998-2018 were collected from the leprosy management information system in China (LEPMIS). Epidemiological variables were analyzed in this study. Results: 477 new cases were diagnosed between 1998-2018 in this area. The average rate of annual detection was 0.070/100,000, and the average annual prevalence was 0.305/100,000. The mean age of new patients was 46.71 years, and the ratio of male to female was 2.46:1. There were 399 cases (83.6%) of multibacillary (MB) forms. -

International Journal of Leprosy
INTERNATIONAL JOURNAL OF LEPROSY VOL. 3 OCTOBER-DECEMBER, 1935 No.4 ORIGINAL ARTICLES REPORT OF THE PHILIPPINE LEPROSY COMMISSION PRESENTED TO THE GOVERNOR-GENERAL W' SEPTEMBER, 1935 - INTRODUCTION Of late there has been increasing evidence of dissatisfaction on . the part of certain elements of the people with the present manner of leprosy control, with special reference to the system of segregation and conditions of parole. This led recently to a movement on the part of the Philippine Legislature to modify the system, in conse quence of which His Excellency, Governor-General Frank Murphy, on July 23, 1935, appointed a commission "to study and report upon the problem of leprosy control in the Philippines. " The instructions to the Commission were as follows: The Commission will conduct its investigations in the light of the scientific knowledge regarding the control and treatment of leprosy acquired during recent years and make a thorough study of the scientific, public health, social and eco nomic aspects of the problem. The Commission will include in ita report recom mendations with the purpose of improving the present methods of controlling leprosy in the Philippines. The personnel of the Commission was selected to represent those concerned with the legislative, administrative and technical aspects b£ leprosy work in the Philippine Islands, and comprised a number of influential public-spirited members of the lay public. Including certain persons appointed at later dates, the Commission consisted of the following: 389 390 International Jou'rnal of Lep1'Osy 1936 Dr. G. C. Dunham (Major, M.C., U.S.A.), Technical Adviser to the Governor· General on Public Health, Chairman; Mrs. -

Die Beteiligung Jüdischer Ärzte an Der Entwicklung Der Dermatologie Zu Einem Eigenständigen Fach in Frankfurt Am Main
Aus der Klinik und Poliklinik für Dermatologie und Allergologie der Ludwig-Maximilians-Universität München Direktor: Prof. Dr. med. Dr. med. h. c. Thomas Ruzicka Die Beteiligung jüdischer Ärzte an der Entwicklung der Dermatologie zu einem eigenständigen Fach in Frankfurt am Main Dissertation zum Erwerb des Doktorgrades der Zahnheilkunde an der Medizinischen Fakultät der Ludwig-Maximilians-Universität zu München Vorgelegt von Dr. med. Henry George Richter-Hallgarten aus Schönbrunn 2013 1 Mit Genehmigung der Medizinischen Fakultät der Universität München Berichterstatter: Prof. Dr. med. Rudolf A. Rupec Mitberichterstatter: Prof. Dr. med. Wolfgang G. Locher Prof. Dr. med. Dr. phil. Johannes Ring Prof. Dr. med. Joest Martinius Mitbetreuung durch den promovierten Mitarbeiter: Dekan: Prof. Dr. med. Dr. h.c. M. Reiser, FACR, FRCR Tag der mündlichen Prüfung: 16.10.2013 2 Henry George Richter-Hallgarten Die Geschichte der Dermato-Venerologie in Frankfurt am Main Band 1: Die Vorgeschichte (1800 – 1914) und der Einfluss jüdischer Ärzte auf die Entwicklung der Dermatologie zu einem eigenständigen Fach an der Universität Frankfurt am Main 3 Henry George Richter-Hallgarten Dr. med. Der vorliegenden Publikation liegt die Inauguraldissertation: „Die Beteilig- ung jüdischer Ärzte an der Entwicklung der Dermatologie zu einem eigen- ständigen Fach in Frankfurt am Main“ zur Erlangung des Doktorgrades der Zahnheilkunde an der Medizinischen Fakultät der Ludwig-Maximilians- Universität München zugrunde. 4 Karl Herxheimer Scherenschnitt von Rose Hölscher1 „Die Tragödie macht einer Welt – so abscheulich, daß der eigene Vater, den Dingen ihren Lauf in den Abgrund lassend, sie verleugnete – den Prozeß.“ Alfred Polgar 1 Rose Hölscher: Geboren 1897 in Altkirch, gestorben in den 1970-er Jahren in den USA. -

LEPROSY in NORWAY by TH
LEPROSY IN NORWAY by TH. M. VOGELSANG WE do not know when leprosy invaded Norway, nor where it came from. It seems most probable that the disease spread from the British Isles in Viking times. The Norwegian Vikings were in active contact with the other North Sea people, and had settlements in Ireland, the Scottish Islands, the Faroe Islands, Iceland and Greenland. The Vikings brought home not only goods and gold, but also captives of both sexes. Irish women are said to have been especially attractive to the Norwegian Vikings, and it is known that as early as the tenth century leprosy was widespread in Ireland. Indeed the first recorded leper hospital in the British Isles was founded in Ireland in about the seventh century.1 It appears that the Norsemen knew and feared the disease: 'At home in Denmark and Norway nobody had as yet founded hospitals for the lepers, but in England and especially in Ireland, the Norsemen had learnt to look at leprosy as a horrible disease which they had to combat with all their might and main. In 921 when King Gudrod of Dublin plundered Armagh in Ulster he spared, as the Irish Year Books state, "the houses of the prayer where the men of God and the lepers stayed".'2 Soon after these leper hospitals were founded in the Viking settlements around the Irish Sea. In the south of Cumberland on the Furness peninsula is a place called Loppergarth. Traditionally there was a leper hospital here which was probably of Norse origin. Loppergarth is a Nordic name derived from Lobragaard-the first syllable being the old Irish 'lobran' (Gaelic 'lobbrar') meaning sick, especially leprous, while the last syllable is the Norwegian word for a house. -
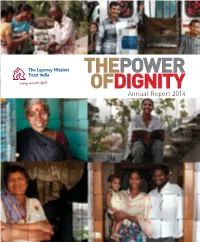
Annual Report 2014 THEME of TLMTI ANNUAL REPORT 2014: the POWER of DIGNITY Introduction to the Theme
THEPOWER OFDIGNITY Annual Report 2014 THEME OF TLMTI ANNUAL REPORT 2014: THE POWER OF DIGNITY Introduction to the theme We all have an innate human longing to be full potential. The power of dignity is the about leprosy among the general public treated with dignity. It has been universally power that makes us complete as human is the biggest obstacle for the people acknowledged that dignity is a basic beings, complete as a society. affected by the disease to claim their human right, and hence, Article 1 of the dignity. It is a major challenge for all who Sadly, even today leprosy is associated Universal Declaration of Human Rights work in the fi eld of leprosy to clear away with stigma, resulting in discrimination (UDHR) says, “All human beings are born the cobwebs of ignorance around leprosy and social exclusion of people affected free and equal in dignity and rights”. Yet, and to facilitate a dignifi ed life for people by the disease. They are still shunned by violation of human dignity is rampant in affected by leprosy. the mainstream society to a sub-human our society, leading to alienation of people existence at the fringes. By not treating In this report, we have put an effort to and communities whose dignity has been them with dignity, the society has pushed highlight how TLMTI, while working with compromised. them to a corner where they experience people affected by leprosy, has brought Dignity is fundamental to human well- lack of self-worth, self-respect, and dignity into their lives. So dear readers, being and social thriving. -

Hansen's Bacillus
s p e c i a l f e a t u r e – h i s t o r y o f n e u r o l o g y Hansen’s bacillus mice developed the disease. Koch announced in 1876 that he had proved this bacterium JMS Pearce MD, FRCP caused anthrax. He went on to identify the Emeritus Consultant Neurologist, Department of Neurology, Hull Royal Infirmary, UK. bacterial causes of tuberculosis (1882), and cholera(1883). Correspondence to: Gerhard Armauer Hansen (1841-1912) J.M.S. Pearce, 304 Beverley Road Anlaby, East Yorks, HU10 7BG, UK. worked at St. Jørgen’s hospital in Bergen, Email: [email protected] striving to find the cause of leprosy. Importantly, Hansen’s identification of M. leprae preceded Conflict of Interest statement: None declared. Koch’s seminal investigations.5 Leprosy is a Date first submitted: 23/1/18 chronic mycobacterial infection that affected Acceptance date: 4/2/18 millions of people, mainly in Brazil, India, and To cite: Pearce JMS, ACNR 2018;17(4);16-18 Indonesia. The Tuberculoid or paucibacillary type shows well-expressed cell-mediated immunity that controls bacillary multiplication by forming Figure 2: Gerhard Armauer Hansen. 1900s Abstract epithelioid-cell granulomas. The lepromatous (Photo by Mondadori Portfolio via Getty Images) Because of its gradually declining incidence or multibacillary type shows cellular anergy many UK physicians rarely encounter leprosy towards M. leprae, thus profuse bacillary Hansen also observed visual impairment which is thus easily overlooked. Hansen’s multiplication. Between these is a continuum, or blindness now known to result either from discovery of mycobacterium leprae, the first varying from borderline tuberculoid, through mycobacterial infiltration of the anterior identified human bacterial infection, was borderline, to those with little cellular response, segment of the eye, or from trophic changes of crucial importance. -

Franz Nissl (1860-1919), Noted Neuropsychiatrist and Neuropathologist, Staining the Neuron, but Not Limiting It
Dement Neuropsychol 2019 September;13(3):352-355 History Note http://dx.doi.org/10.1590/1980-57642018dn13-030014 Franz Nissl (1860-1919), noted neuropsychiatrist and neuropathologist, staining the neuron, but not limiting it Marleide da Mota Gomes1 ABSTRACT. Franz Alexander Nissl carried out studies on mental and nervous disorders, as a clinician, but mainly as a pathologist, probably the most important of his time. He recognized changes in glial cells, blood elements, blood vessels and brain tissue in general, achieving this by using a special blue stain he himself developed – Nissl staining, while still a medical student. However, he did not accept the neuron theory supported by the new staining methods developed by Camillo Golgi and Santiago Ramón y Cajal. Nissl had worked with the crème de la crème of German neuropsychiatry, including Alois Alzheimer, besides Emil Kraepelin, Korbinian Brodmann and Walther Spielmeyer. He became (1904), Kraepelin’s successor as Professor of Psychiatry and Director of the Psychiatric Clinic, in Heidelberg. Moreover, in 1918, the year before Nissl´s death, Kraepelin offered him a research position as head of the Histopathology Department of the newly founded “Deutsche Forschungsanstalt fur Psychiatrie” of the Max Planck Institute for Psychiatry, in Munich. Key words: Franz Nissl, neuropathology, staining method, neuron theory. FRANZ NISSL (1860-1919), NOTÁVEL NEUROPSIQUIATRA E NEUROPATOLOGISTA, TINGINDO O NEURÔNIO, MAS NÃO O LIMITANDO RESUMO. Franz Alexander Nissl realizou estudos sobre transtornos mentais e nervosos, como clínico, mas principalmente como patologista, provavelmente o mais importante de seu tempo. Ele reconheceu mudanças nas células gliais, elementos sangüíneos, vasos sangüíneos e tecido cerebral em geral, realizando-o por meio de um corante azul especial desenvolvida por ele mesmo – coloração de Nissl, ainda como estudante de medicina. -

Master Thesis
Bakteriologiens inntog i medisinutdanningen ved Det kongelige Frederiks universitet i Kristiania, 1885-1915 Helene Larsen Masteroppgave i historie Institutt for arkeologi, historie, kultur- og religionsvitenskap UNIVERSITETET I BERGEN Våren 2019 II Bakteriologiens inntog i medisinutdanningen ved Det kongelige Frederiks universitet i Kristiania, 1885-1915 III © Helene Larsen 2019 Bakteriologiens inntog i medisinutdanningen ved Det kongelige Frederiks universitet i Kristiania, 1885-1915 Helene Larsen https://bora.uib.no/ IV Abstract In 1885, the Norwegian medical education at the Royal Frederick University of Christiania (University of Oslo) became the subject of a reform debate that lasted for 30 years. This was a consequence of the fact that academic medicine had become increasingly scientific, systematic and specialized during the 19th century, which had led to the emergence of several new medical disciplines. One of these were the field of bacteriology (the study of bacteria and their relation to medicine). This thesis is based on a survey of the Norwegian reform debates on the education of medicine, with a special regard to bacteriology as a representative of the emergence of a more scientific, laboratory-based medicine. The overall aim of the thesis is to determine when bacteriology became established as a permanent part of the Norwegian medical education at the University, and to what extent this contributed to changing Norwegian medical practice. The debates took place at The Faculty of Medicine, as well as within the Norwegian Medical Association (‘Den norske Lægeforening’) and The Norwegian Medical Society (‘Det norske medicinske Selskab’). The period of my analysis concludes with the decision on a new examination regulation that was enacted in 1915. -

Several Springs, One Stream United Church of Christ in the Philippines
Several Springs, One Stream United Church of Christ in the Philippines Volume I: Heritage and Origins (1898-1948) T. Valentino Sitoy, Jr. ISBN 11-11-38-3 Copyright @ 1992 All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording, or otherwise, except in critical reviews, without the prior permission of the publisher. United Church of Christ in the Philippines 877 Epifanio de los Santos Avenue Quezon City, Philippines Several Springs, One Stream United Church of Christ in the Philippines Volume I: Heritage and Origins (1898-1948) T. Valentino Sitoy, Jr. United Church of Christ in the Philippines FOREWORD To capture in print a history of a people in their faith journey is itself a miracle! Indeed, it is the work of the Holy Spirit manifesting itself in the ingenuity and intellect of church scholars, such as this particular author. To be able to delve into the peculiarities of each of the uniting churches - each with its own particular historical journey - and weave them into one fabric of a United Church of Christ in the Philippines is indeed a work of genius. Leaping out of the pages are familiar names of persons, places and events as the stories of each of the denominational springs flow into the one stream of a church body, losing themselves into the one body. And as the names are read again and again, by individuals and groups of this volume, they will come to life and bring back memories of the many pioneers of the United Church of Christ in the Philippines, without whom we will not be what we are today, nor hope to be what we ought to be, in the future. -

International Symposium on Hansen's Disease/Leprosy History As
International Symposium on Hansen’s Disease/Leprosy History as Heritage of Humanity 22nd – 25th April 2017, Okayama, Japan Organised by Sasakawa Memorial Health Foundation, Japan In corporation with Setouchi City, Okayama, Japan Day 2@Yume Topia Osafune Cover 1. Wind Dance monument, National Sanatorium Oshima Seisho-en, Kagawa, Japan 2. Spinalonga, Greece 3. History Museum, National Sanatorium Nagashima Aisei-en, Okayama, Japan 1 2 3 4. The building that housed the former elementary and junior high school, National Sanatorium 4 5 6 Oku Komyo-en, Okayama, Japan 5. Old photo of Bergen, Norway, showing St. George's Hospital 6. Culion Island, Philippines International Symposium on Hansen’s Disease/Leprosy History as Heritage of Humanity 22nd – 25th April 2017, Okayama, Japan Organised by Sasakawa Memorial Health Foundation, Japan In corporation with Setouchi City, Okayama, Japan II Contents Foreword Page • Prof. Etsuko Kita .................................................................. IV Greetings • Prof. Kenzo Kiikuni, President, Sasakawa Memorial Health Foundation ................... 1 • Mr. Akinari Takehisa, Mayor, Setouchi City ............................................ 2 • Mr. Kazuo Mori, President, Residents committee, Oshima Seisho-en ...................... 3 • Mr. Takeshi Oku, Residents committee, Oku Komyo-en ................................. 4 Keynote Lecture • Dr. Tetsu Nakamura, Representative, Peshawar-kai in Pakistan and Afghanistan ........... 6 Session A “Preserving Materials & Testimonies” Lectures • Mr. Tomohisa Tamura