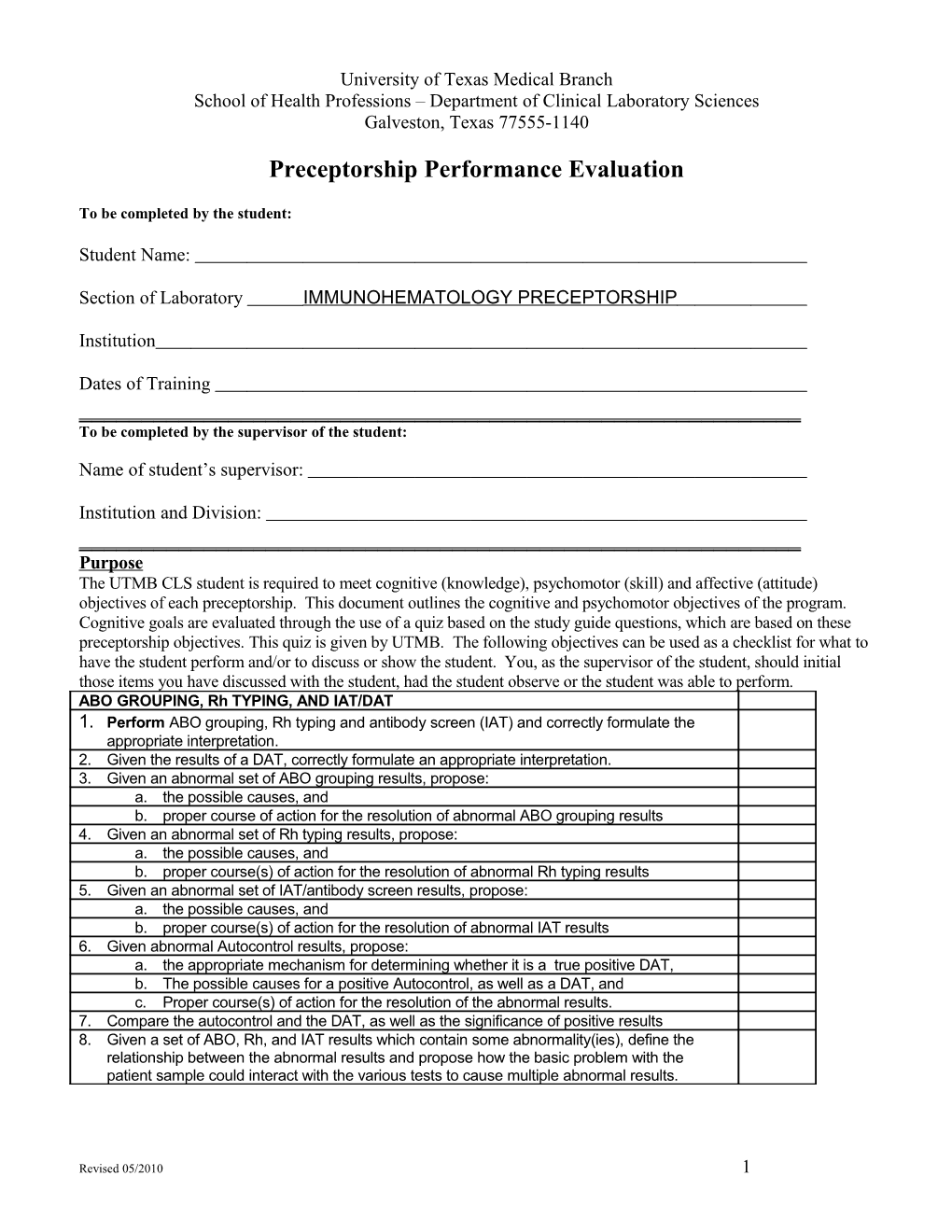
University of Texas Medical Branch School of Health Professions – Department of Clinical Laboratory Sciences Galveston, Texas 77555-1140
Preceptorship Performance Evaluation
To be completed by the student:
Student Name:
Section of Laboratory IMMUNOHEMATOLOGY PRECEPTORSHIP
Institution
Dates of Training ______To be completed by the supervisor of the student:
Name of student’s supervisor:
Institution and Division: ______Purpose The UTMB CLS student is required to meet cognitive (knowledge), psychomotor (skill) and affective (attitude) objectives of each preceptorship. This document outlines the cognitive and psychomotor objectives of the program. Cognitive goals are evaluated through the use of a quiz based on the study guide questions, which are based on these preceptorship objectives. This quiz is given by UTMB. The following objectives can be used as a checklist for what to have the student perform and/or to discuss or show the student. You, as the supervisor of the student, should initial those items you have discussed with the student, had the student observe or the student was able to perform. ABO GROUPING, Rh TYPING, AND IAT/DAT 1. Perform ABO grouping, Rh typing and antibody screen (IAT) and correctly formulate the appropriate interpretation. 2. Given the results of a DAT, correctly formulate an appropriate interpretation. 3. Given an abnormal set of ABO grouping results, propose: a. the possible causes, and b. proper course of action for the resolution of abnormal ABO grouping results 4. Given an abnormal set of Rh typing results, propose: a. the possible causes, and b. proper course(s) of action for the resolution of abnormal Rh typing results 5. Given an abnormal set of IAT/antibody screen results, propose: a. the possible causes, and b. proper course(s) of action for the resolution of abnormal IAT results 6. Given abnormal Autocontrol results, propose: a. the appropriate mechanism for determining whether it is a true positive DAT, b. The possible causes for a positive Autocontrol, as well as a DAT, and c. Proper course(s) of action for the resolution of the abnormal results. 7. Compare the autocontrol and the DAT, as well as the significance of positive results 8. Given a set of ABO, Rh, and IAT results which contain some abnormality(ies), define the relationship between the abnormal results and propose how the basic problem with the patient sample could interact with the various tests to cause multiple abnormal results.
Revised 05/2010 1 ANTIBODY IDENTIFICATION AND Hemolytic Disease of the Newborn 1. Perform routine antibody identification for single and multiple antibody problems including rule outs and antigen typing. .
Revised 05/2010 2 2. Given antibody panel results and the antigrams from a different set of panel cells, select cells required to determine the antibody specificity, given the initial panel reactions. 3. Given the results of regular and enzyme treated cells, determine antibody specificity/ies and additional specificities that may be ruled out on the reactions observed. 4. Discuss the use of Gel and Solid Phase technology. Interpret reactions based on these methodologies. 5. Diagram a plan for the use of auto absorption in resolving antibody problems. 6. Develop a strategy (why, when, how) for the use of chloroquine and EGA in resolving antibody problems. 7. Explain the application of the saline replacement technique in resolving antibody problems. 8. Perform and interpret antigen typing. 9. Given the results of an antigen typing, judge the accuracy. 10. Formulate a strategy for performing an elution using the elu-kit and Lui Freeze. 11. Determine what is done with an eluate: a. Compare the results of an elution with the serum/plasma panel b. Use of the results for component therapy. c. Determine the antigens present on patient cells 12. Given the results of ABO, Rh and other antigen typings, propose the most likely genotype and any alternate genotypes. 13. Correctly use the Fisher-Race and Weiner nomenclature, given the patient’s phenotype 14. Perform & interpret ABO grouping, Rh typing, and DAT on cord blood specimen 15. Identify & explain the possible causes for false results on cord blood specimen testing 16. Identify/explain the type of HDN, given the results of maternal & cord studies . 17. Perform testing & determine the eligibility of an individual for antenatal, postnatal and post-abortion Rh Immune Globulin 18. Identify & explain the possible causes for false result with the Fetal Bleed Screening Test 19. Perform & interpret the Fetal Bleed Screening Test
COMPATIBILITY TESTING: 1. Given the labeled specimen and blood request for a patient, correctly evaluate the acceptability of the specimen, its labeling, and accompanying documentation for purposes of compatibility testing. 2. Given the results of the ABO Grouping, Rh typing, IAT, and information from prior blood bank records on a patient, correctly determine the appropriate ABO Group and Rh type of units to be selected for transfusion and the type of crossmatch required. 3. Given a sample for compatibility testing, perform all required testing, read & record results, as well as interpret within the laboratory’s prescribed time limits for an entry level CLS. 4. Given a patient sample for which group specific units are not available, correctly select the appropriate ABO/Rh units for the patient. This should include appropriate selection of units given the laboratory’s blood inventory and other patients’ blood requirements. 5. Given a problem compatibility result, propose the proper course of action, in sequence to be taken in resolving the compatibility problem. 6. Given a patient with a clinically significant antibody, propose the proper steps to be taken in order to obtain units which are safe for infusion into the patient. 7. Given a request for release of units on a patient, correctly define the steps to ensure the release of appropriate units to the patient. 8. Delineate the appropriate steps to be taken in releasing blood for emergency transfusion when there is not time to determine the patient’s ABO group and Rh type. 9. Propose the correct steps to be taken in completing the laboratory testing and paper work on the units released to a patient for emergency transfusion. 10. Given a patient’s Type and Screen results and past history, assess whether an extended, immediate spin or a computerized crossmatch is acceptable.
EVALUATION OF POSSIBLE TRANSFUSION REACTIONS 1. Outline the procedure for the initial transfusion reaction work-up.
Revised 05/2010 3 2. Justify visual comparison of the pre-transfusion and post-transfusion serum/plasma. 3. Compare the major types of transfusion reactions and their causes. 4. Compare the possible significance of hemolysis in a post-transfusion specimen when not present in the pre-transfusion sample. 5. Explain the significance(s) of a positive DAT in a post-transfusion specimen. 6. Explain the significance(s) of a mixed field in a post-transfusion specimen. 7. Propose the most probable reason for an ABO transfusion reaction occurring. 8. Propose what, if any, additional work must be done, given the initial work-up of a transfusion reaction.
PREPARATION, QUALITY CONTROL & STORAGE OF COMPONENTS 1. List the residual white cell count for leukocyte-reduced RBCs by filtration. 2. Compare platelets combined from multiple single whole blood donor units versus an apheresis donation in terms of shelf life, concentration, and risk of immunization to platelet and HLA antigens. 3. List complications which have made fresh frozen plasma a less desirable component for volume expansion 4. Differentiate between the storage temperatures and shelf lives for packed RBCs, leukocyte-reduced RBCs by in-line filtration, pooled platelets, leukocyte-reduced pooled platelets, thawed fresh frozen plasma, pooled cryoprecipitate, deglycerized frozen RBCs and washed RBCs. 5. Determine the appropriate compatibility testing required for each of the components listed above 6. Differentiate between the shelf-life of CPDA-1, CPD, and additive preserved RBCs. 7. List the quality control criteria for concentration of “cells” in packed RBCs, leukocyte- reduced RBCs, frozen RBCs, and platelet concentrates. 8. Describe the quality control criteria for Factor VIII and fibrinogen in cryoprecipitate. 9. Differentiate the rational for using packed RBCs, washed RBCs, leukocyte-reduced RBCs, platelet concentrate, fresh frozen plasma, and cryoprecipitate. 10. Prepare a RBC unit for issue to a patient for transfusion. 11. Describe the preparation for issuing fresh frozen plasma, cryoprecipitate, platelet aliquots for neonates, and leukocyte-reduced components for transfusion. 12. Formulate a procedure for placing into inventory the blood and components received from the blood collection center.
QUALITY ASSURANCE and Quality Control 1. Compare and contrast Quality Control versus Quality Assurance. 2. Identify the items that must be quality controlled; include the frequency of performance and range limits. 3. List the quality control required on blood instruments, ie centrifuges, refrigerator alarms, pipettes, cell washes, sterile connecting devices, automated cell and serum typing instruments. 4. Given reagent reactions, recommend a course of action which will confirm the source(s) of error. 5. Determine the laboratories standards for maintaining required records. 6. Differentiate between record, document and form in terms of Quality Assurance. 7. Perform reagent Quality Control.
Scale:
Revised 05/2010 4 3 = exceeds entry level requirements (>80%) – produces work of high quality 2 = Meets entry level requirements (70%) – requires little duplication of instruction and makes few errors 1 = does not meet entry level requirements (<70%) - improvement needed.
) ) y
l l r s
Criteria: please circle the box which you feel represents this % % e e t t 0 0 v v n n 8 7 e e e e ( l student’s ability during and/or after this preceptorship rotation. l
>
t ( s m y ) y e t e s r r e n t r t t % i e n n n m 0 u e e e m 7
q T s e s m < e t r ( d e O i e R e r
e u i N l e
q u e c s M e v x q e r e e o E l R D
Technical Knowledge and Competence 1. Recalled the scientific principles of laboratory test procedures 3 2 1 2. Discussed technical and procedural concepts 3 2 1 3. Detected the need for and used problem solving procedures 3 2 1 4. Integrated and practiced safety regulations 3 2 1 5. Explained the principles of quality assurance and quality control 3 2 1 6. Discussed scientific information and the application of principles 3 2 1 as they related to tests performed/sent to reference lab by this area. 7. Recognized abnormal laboratory data and made correlations with 3 2 1 associated pathology 8. Confirmed the validity of test results and selected additional test 3 2 1 procedures 9. Performed and interpreted diagnostic tests with accuracy 3 2 1 10. Used quality control procedures 3 2 1 11. Calibrated instruments or determined QC requirements for 3 2 1 instruments. 12. Evaluated computer generated data 3 2 1 13. Effectively analyzed malfunctions and trouble shoots instruments 3 2 1 and/or procedures 14. Selected appropriate samples and test methods 3 2 1 15. Selected appropriate reagents/ blood products and instruments. 3 2 1 16. Evaluated laboratory Data 3 2 1
Revised 05/2010 5 Please indicate your appraisal of the individual’s performance as a clinical laboratory science professional by checking one box:
EXCELLENT [ ] Average [ ] Below Average [ ]
Please provide examples of any marks of “Does not meet entry level Requirements” level 1 and/or any other comments you would like to make about this student:
Supervisor: Please sign below. Thank you for you appraisal of this student’s experience at your facility.
Signature: Date:
This evaluation may be given to the student to give to the Education Coordinator at UTMB or you may mail or fax:
University of Texas Medical Branch School of Health Professions Clinical Laboratory Sciences Department Preceptorship Coordinator 301 University Blvd Galveston, Texas 77555-1140
Fax: 409-772-9470
Revised 05/2010 6