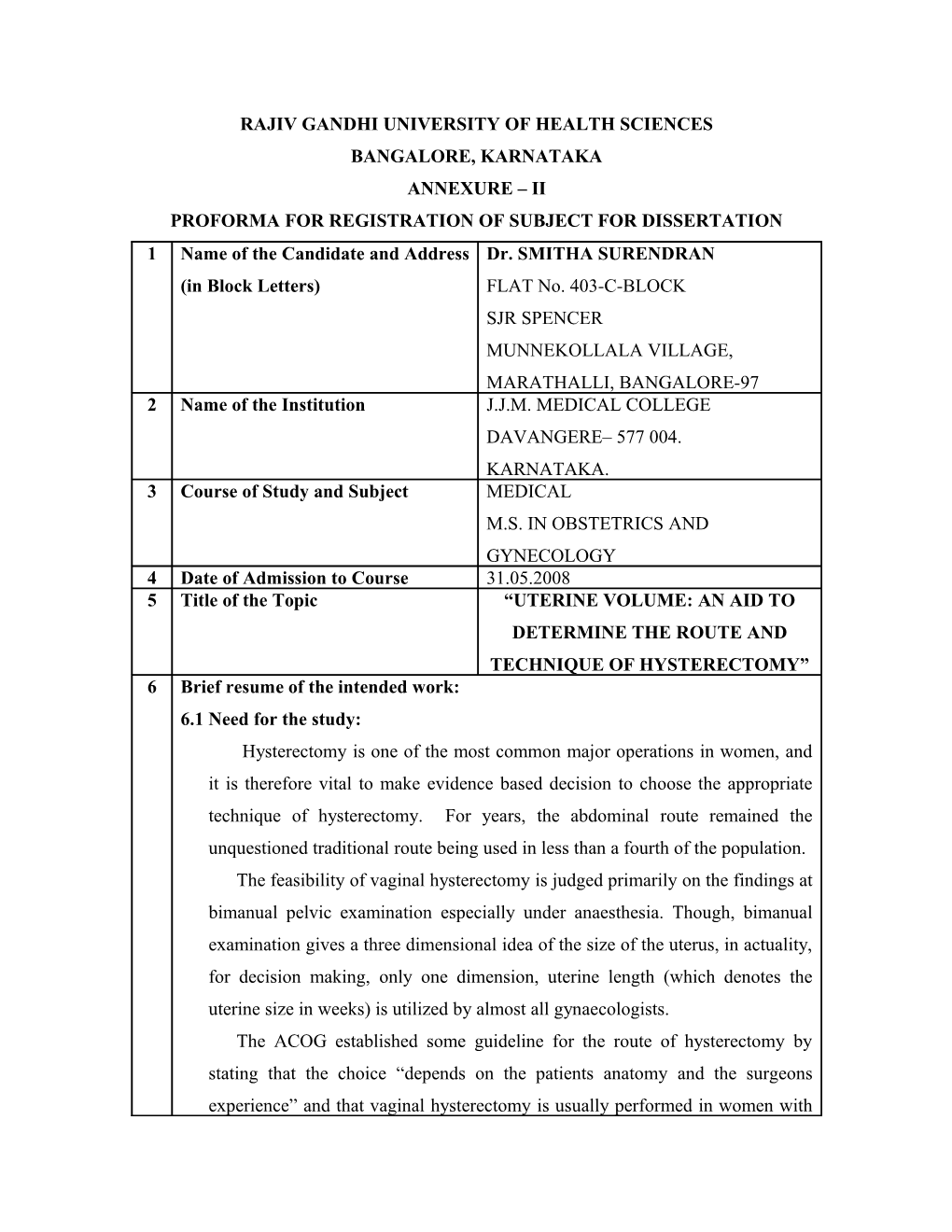
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES BANGALORE, KARNATAKA ANNEXURE – II PROFORMA FOR REGISTRATION OF SUBJECT FOR DISSERTATION 1 Name of the Candidate and Address Dr. SMITHA SURENDRAN (in Block Letters) FLAT No. 403-C-BLOCK SJR SPENCER MUNNEKOLLALA VILLAGE, MARATHALLI, BANGALORE-97 2 Name of the Institution J.J.M. MEDICAL COLLEGE DAVANGERE– 577 004. KARNATAKA. 3 Course of Study and Subject MEDICAL M.S. IN OBSTETRICS AND GYNECOLOGY 4 Date of Admission to Course 31.05.2008 5 Title of the Topic “UTERINE VOLUME: AN AID TO DETERMINE THE ROUTE AND TECHNIQUE OF HYSTERECTOMY” 6 Brief resume of the intended work: 6.1 Need for the study: Hysterectomy is one of the most common major operations in women, and it is therefore vital to make evidence based decision to choose the appropriate technique of hysterectomy. For years, the abdominal route remained the unquestioned traditional route being used in less than a fourth of the population. The feasibility of vaginal hysterectomy is judged primarily on the findings at bimanual pelvic examination especially under anaesthesia. Though, bimanual examination gives a three dimensional idea of the size of the uterus, in actuality, for decision making, only one dimension, uterine length (which denotes the uterine size in weeks) is utilized by almost all gynaecologists. The ACOG established some guideline for the route of hysterectomy by stating that the choice “depends on the patients anatomy and the surgeons experience” and that vaginal hysterectomy is usually performed in women with mobile uteri no larger than one at 12 weeks of gestation (i.e. 280gm). However much larger uteri can be removed vaginally if surgeon is experienced in reducing techniques, like morcellation, bivaling and coning. Although this guideline is a good beginning, more specific criteria are desirable Thus a preoperative sonographic estimation of uterine volume which give exact uterine size in 3 dimension could be of great help in the decision making for choice of the vaginal route as well as for anticipating problems during hysterectomy.
6.2 Review of Literature Shirlina D, Shirish S (2004) this study, women scheduled for hysterectomy with uterine volume ≤ 700cm3 were included. The route of hysterectomy was decided on the basis of sonographically estimated uterine volume, clinical examination and examination under anesthesia. When the uterine volume was < 300cm3 vaginal hysterectomy was feasible. Above 400cm3, debulking was required in all cases and trial of vaginal hysterectomy be considered. Seth SS, Shan NM (2002) in this study, preoperative sonographic estimation of the uterine volume was carried out in 380 non pregnant women with non malignant mobile uteri of up to 18-20 weeks size scheduled for VH. No difficulties were encountered to the trial basis particularly where volume < 200cm3. For >400cm3, debulking was required. VH failed in 4 cases with volume of 500 -700cm3. VH should be considered on a trial bases particularly when volume > 400cm3. Kovac R (1995) 617 women were assigned to a route of hysterectomy on the basis of uterine size (greater than or less than 280gm), presumptive risk factors and uterine or adnexal immobility or in accessibility. VH alone or in conjunction with laparoscopy was successful in 99.5% of women. In 94% of those in whom vaginal route was successful included those whose uterine weight exceeded 280gm. Kung FT, Chang SY (19996) study was done to assess the correlation between the estimated volume based on ultrasonic measurement in vivo and the actual weight of the diseased uterus after hysterectomy and then retrospectively tried to establish a simple equation to convert the volume into weight in grams. A total of 105 women with non malignant diseased, uteri which were prepared to undergo laparoscopy – assisted VH had preoperative USG to estimate the uterine size. Uterine volume was calculated and correlation coefficient determined. There was a close, positive correlation between the estimated uterine volume and actual uterine weight. Magos A (1996), study was done to assess the feasibility and safety of performing VH on enlarged uteri the equivalent of 14-20 weeks of gestation in size. The mean uterine size was 16.3 weeks (range 14-20 weeks). All hysterectomies were completed successfully by the vaginal route. The uteri weighed 380-1100gm, with a mean of 638.7gm. Bisection combined with myomectomy and morcellation were used in most cases to obtain reduction in uterine size, whereas coring was only utilized in 2 cases.
6.3 Objectives of the study: (1) To assess the value of uterine volume estimated ultrasonographically, indecision making for route and technique of hysterectomy. This of greater value when the uterine size is more than 8 to 10 weeks pregnancy.
7. MATERIALS AND METHODS 7.1 Source of data Cases undergoing hysterectomy for benign disorders in the hospitals attached to J.J.M. Medical College, namely, Bapuji Hospital, Davangere Chigateri General Hospital, Davangere Women and Children Hospital, Davangere
7.2 Method of collection of data (including sample procedure if any) Design : prospective study No of cases: 50 Duration of study: November 2008 to November 2010
Inclusion Criteria: Women scheduled for hysterectomy with uterine volume ≤700cm3. Indications were benign disorders like DUB, fibroids, adenomyosis.
Exclusion Criteria: Uterine volume > 700cm3 or uterine size 18-20 weeks Factors like restricted uterine mobility, presence of adnexal pathology.
Procedure of the study: For women scheduled for hysterectomy, the route of hysterectomy would be decided on the basis of sonographically estimated uterine volume, clinical examination and examination if required under anaesthesia. The uterine volume will be calculated by measuring the three dimensions including length (L – measured from the fundus to the internal os of the cervix), width (w – transverse diameter at the level of the cornua) and anteroposterior diameter (AP – at the level of cornua and perpendicular to the width), by the use of formula or multiplying L x W x AP x 0.542. The estimates were withheld from the authors until after operation. Clinical estimation of the uterine size, route taken for hysterectomy, ease or difficulties encountered during hysterectomy and time taken to operate would be carefully recorded. Post operative uteri will be weighed and compared with uterine volume estimated preoperatively. Women studied should have pelvic sonography at the same centre by the same sonologists.
7.3 Does the study require any investigations or interventions to be conducted on patients or other humans or animals? If so describe briefly. Yes Investigations include: Routine blood – Hb%, RBS, Blood Urea, Serum Creatinine Urine anlaysis ECG HIV, HBsAg Ultrasonogram Transabdominal, Transvaginal.
7.4 Has ethical clearance been obtained from your institution in case of 7.3? Yes
8. LIST OF REFERENCE 1) Shiriline D, Shirish S. Uterine volume: An aid to determine the route and technique of hysterectomy. J Obstet and Gynec India 2004; 54 (1): 68-72.
2) Sheth SS, Shah NM. Preoperative sonographic estimation of uterine volume: An aid to determine the route of hysterectomy. J Gynecol Surg 2002; 18 (1): 13.
3) Kovac SR. Guideline to determine the route of hysterectomy. Obstet and Gynecol 1995; 85 (1): 18-22.
4) Kung FT, Chang SY. The relationship between ultrasonic volume and actual weight of pathologic uterus. Gynecology and Obstetric Investigation 1996; 42 (1): 35-38.
5) Magos A, Bournas N, Sinha R. Vaginal hysterectomy for the large uterus. Br J Obstet Gynecol 1996; 103: 246-51. 9. Signature of the Candidate
This study is under taken to know the value of sonographic uterine volume 10. Remarks of the Guide measurement to decide for route and technique of hysterectomy for benign lesion of the uterus. 11. Name & Designation of (in Block letters) 11.1 Guide Dr. DHARMA REDDY MD, DGO PROFESSOR DEPARTMENT OF OBSTETRICS & GYNAECOLOGY, J.J.M. MEDICAL COLLEGE, DAVANGERE – 577 004.
11.2 Signature
11.3 Co-Guide (If any)
11.4 Signature
11.5 Head of the Department Dr. B.R. DAKSHAYANI MD, DGO. PROFESSOR & HOD, DEPARTMENT OF OBSTETRICS & GYNAECOLOGY, J.J.M. MEDICAL COLLEGE, DAVANGERE – 577 004.
11.6 Signature 12 12.1 Remarks of the Chairman & the Principal
12.2 Signature