09a826193e718c0be8c6b2f6224b6745.doc Page 1 of 23
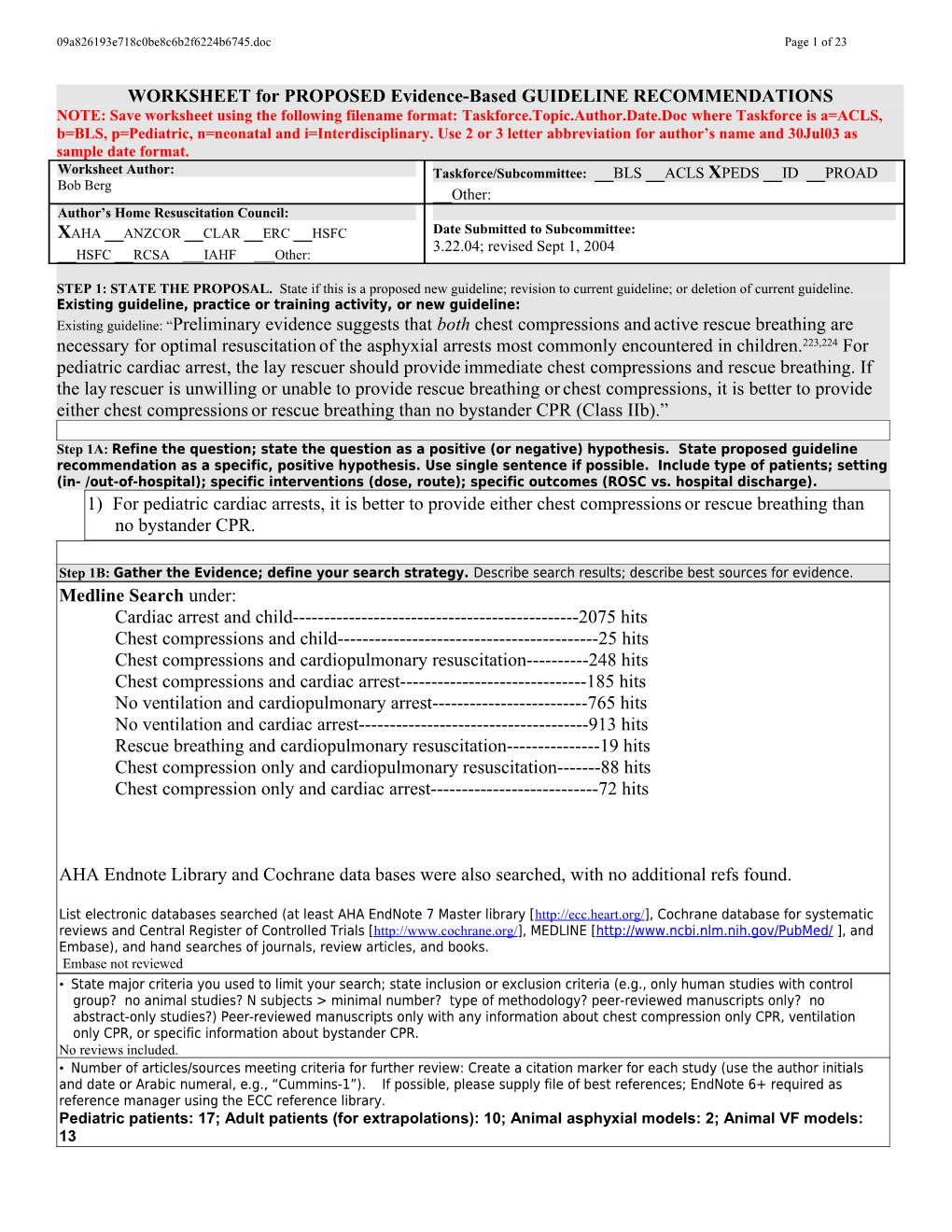
WORKSHEET for PROPOSED Evidence-Based GUIDELINE RECOMMENDATIONS NOTE: Save worksheet using the following filename format: Taskforce.Topic.Author.Date.Doc where Taskforce is a=ACLS, b=BLS, p=Pediatric, n=neonatal and i=Interdisciplinary. Use 2 or 3 letter abbreviation for author’s name and 30Jul03 as sample date format. Worksheet Author: Taskforce/Subcommittee: __BLS __ACLS XPEDS __ID __PROAD Bob Berg __Other: Author’s Home Resuscitation Council: XAHA __ANZCOR __CLAR __ERC __HSFC Date Submitted to Subcommittee: 3.22.04; revised Sept 1, 2004 __HSFC __RCSA ___IAHF ___Other:
STEP 1: STATE THE PROPOSAL. State if this is a proposed new guideline; revision to current guideline; or deletion of current guideline. Existing guideline, practice or training activity, or new guideline: Existing guideline: “Preliminary evidence suggests that both chest compressions and active rescue breathing are necessary for optimal resuscitation of the asphyxial arrests most commonly encountered in children.223,224 For pediatric cardiac arrest, the lay rescuer should provide immediate chest compressions and rescue breathing. If the lay rescuer is unwilling or unable to provide rescue breathing or chest compressions, it is better to provide either chest compressions or rescue breathing than no bystander CPR (Class IIb).”
Step 1A: Refine the question; state the question as a positive (or negative) hypothesis. State proposed guideline recommendation as a specific, positive hypothesis. Use single sentence if possible. Include type of patients; setting (in- /out-of-hospital); specific interventions (dose, route); specific outcomes (ROSC vs. hospital discharge). 1) For pediatric cardiac arrests, it is better to provide either chest compressions or rescue breathing than no bystander CPR.
Step 1B: Gather the Evidence; define your search strategy. Describe search results; describe best sources for evidence. Medline Search under: Cardiac arrest and child------2075 hits Chest compressions and child------25 hits Chest compressions and cardiopulmonary resuscitation------248 hits Chest compressions and cardiac arrest------185 hits No ventilation and cardiopulmonary arrest------765 hits No ventilation and cardiac arrest------913 hits Rescue breathing and cardiopulmonary resuscitation------19 hits Chest compression only and cardiopulmonary resuscitation------88 hits Chest compression only and cardiac arrest------72 hits
AHA Endnote Library and Cochrane data bases were also searched, with no additional refs found.
List electronic databases searched (at least AHA EndNote 7 Master library [http://ecc.heart.org/], Cochrane database for systematic reviews and Central Register of Controlled Trials [http://www.cochrane.org/], MEDLINE [http://www.ncbi.nlm.nih.gov/PubMed/ ], and Embase), and hand searches of journals, review articles, and books. Embase not reviewed • State major criteria you used to limit your search; state inclusion or exclusion criteria (e.g., only human studies with control group? no animal studies? N subjects > minimal number? type of methodology? peer-reviewed manuscripts only? no abstract-only studies?) Peer-reviewed manuscripts only with any information about chest compression only CPR, ventilation only CPR, or specific information about bystander CPR. No reviews included. • Number of articles/sources meeting criteria for further review: Create a citation marker for each study (use the author initials and date or Arabic numeral, e.g., “Cummins-1”). . If possible, please supply file of best references; EndNote 6+ required as reference manager using the ECC reference library. Pediatric patients: 17; Adult patients (for extrapolations): 10; Animal asphyxial models: 2; Animal VF models: 13 09a826193e718c0be8c6b2f6224b6745.doc Page 2 of 23
STEP 2: ASSESS THE QUALITY OF EACH STUDY Step 2A: Determine the Level of Evidence. For each article/source from step 1, assign a level of evidence—based on study design and methodology. Level of Definitions Evidence (See manuscript for full details) Level 1 Randomized clinical trials or meta-analyses of multiple clinical trials with substantial treatment effects Level 2 Randomized clinical trials with smaller or less significant treatment effects Level 3 Prospective, controlled, non-randomized, cohort studies Level 4 Historic, non-randomized, cohort or case-control studies Level 5 Case series: patients compiled in serial fashion, lacking a control group Level 6 Animal studies or mechanical model studies Level 7 Extrapolations from existing data collected for other purposes, theoretical analyses Level 8 Rational conjecture (common sense); common practices accepted before evidence-based guidelines
Step 2B: Critically assess each article/source in terms of research design and methods. Was the study well executed? Suggested criteria appear in the table below. Assess design and methods and provide an overall rating. Ratings apply within each Level; a Level 1 study can be excellent or poor as a clinical trial, just as a Level 6 study could be excellent or poor as an animal study. Where applicable, please use a superscripted code (shown below) to categorize the primary endpoint of each study. For more detailed explanations please see attached assessment form.
Component of Study and Rating Excellent Good Fair Poor Unsatisfactory Design & Highly appropriate Highly appropriate Adequate, Small or clearly Anecdotal, no sample or model, sample or model, design, but biased population controls, off randomized, proper randomized, proper possibly biased or model target end-points controls controls Methods AND OR OR OR OR Outstanding Outstanding accuracy, Adequate under Weakly defensible Not defensible in accuracy, precision, and data the in its class, limited its class, precision, and data collection in its class circumstances data or measures insufficient data collection in its or measures class
A = Return of spontaneous circulation C = Survival to hospital discharge E = Other endpoint B = Survival of event D = Intact neurological survival
Step 2C: Determine the direction of the results and the statistics: supportive? neutral? opposed?
DIRECTION of study by results & statistics: SUPPORT the proposal NEUTRAL OPPOSE the proposal Outcome of proposed guideline Outcome of proposed guideline Outcome of proposed guideline Results superior, to a clinically important no different from current inferior to current approach degree, to current approaches approach 09a826193e718c0be8c6b2f6224b6745.doc Page 3 of 23
Step 2D: Cross-tabulate assessed studies by a) level, b) quality and c) direction (ie, supporting or neutral/ opposing); combine and summarize. Exclude the Poor and Unsatisfactory studies. Sort the Excellent, Good, and Fair quality studies by both Level and Quality of evidence, and Direction of support in the summary grids below. Use citation marker (e.g. author/ date/source). In the Neutral or Opposing grid use bold font for Opposing studies to distinguish them from merely neutral studies. Where applicable, please use a superscripted code (shown below) to categorize the primary endpoint of each study. 09a826193e718c0be8c6b2f6224b6745.doc Page 4 of 23
Supporting Evidence For pediatric cardiac arrests, it is better to provide either chest compressions or rescue breathing than no bystander CPR e c
n Hallstrom’00, e
d Excellent Kouwenhoven ’60,
i Kouwenhoven ’60b,c Berg Circ ’00
v Bossaert ’89, van E
Hoeyweghen ’93 f o
y t i l
a Good Holmberg ’01, u Waalewijn ’01 Q
Berg ’93,* Chandra ’94,* Fair Mogayzel ’95, Sirbaugh ’99, Berg ’95,* Hickey ’95, Nichter ’89, Friesen Engoren ’97,* ’82, Biggart ’90, Christensen ’97, Noc ’95,* Fiser ’87, Quan ’90, Kemp ’91, Berg ’97a,* Kyriacou ’94, Schindler ’96, Berg’97b,* Kuisma ’95, Young ’99, Kern ’98,* Suominem ’02, Li ’99 Berg ’01,* Kern ’02,* Sanders ’02* 1 2 3 4 5 6 7 8 Level of Evidence A = Return of spontaneous circulation C = Survival to hospital discharge E = Other endpoint B = Survival of event D = Intact neurological survival *=VF animal models
Neutral or Opposing Evidence For pediatric cardiac arrests, it is better to provide either chest compressions or rescue breathing than no bystander CPR e c n e
d Excellent
i Berg CCM ’99 v E
f o
y t i l
a Good Cummins ’91, Wik u Idris ’95a, Idris ’95b ’94, Gallagher ’95 Q
Fair
1 2 3 4 5 6 7 8 Level of Evidence A = Return of spontaneous circulation C = Survival to hospital discharge E = Other endpoint B = Survival of event D = Intact neurological survival 09a826193e718c0be8c6b2f6224b6745.doc Page 5 of 23
STEP 3. DETERMINE THE CLASS OF RECOMMENDATION. Select from these summary definitions. CLASS CLINICAL DEFINITION REQUIRED LEVEL OF EVIDENCE Class I • Always acceptable, safe • One or more Level 1 studies are present (with rare Definitely recommended. Definitive, • Definitely useful exceptions) excellent evidence provides support. • Proven in both efficacy & effectiveness • Study results consistently positive and compelling • Must be used in the intended manner for proper clinical indications. Class II: • Safe, acceptable • Most evidence is positive Acceptable and useful • Clinically useful • Level 1 studies are absent, or inconsistent, or lack • Not yet confirmed definitively power • No evidence of harm • Class IIa : Acceptable and useful • Safe, acceptable • Generally higher levels of evidence Good evidence provides support • Clinically useful • Results are consistently positive • Considered treatments of choice • Class IIb: Acceptable and useful • Safe, acceptable • Generally lower or intermediate levels of evidence Fair evidence provides support • Clinically useful • Generally, but not consistently, positive results • Considered optional or alternative treatments Class III: • Unacceptable • No positive high level data Not acceptable, not useful, may be • Not useful clinically • Some studies suggest or confirm harm. harmful • May be harmful. • Research just getting started. • Minimal evidence is available Indeterminate • Continuing area of research • Higher studies in progress • No recommendations until • Results inconsistent, contradictory further research • Results not compelling
STEP 3: DETERMINE THE CLASS OF RECOMMENDATION. State a Class of Recommendation for the Guideline Proposal. State either a) the intervention, and then the conditions under which the intervention is either Class I, Class IIA, IIB, etc.; or b) the condition, and then whether the intervention is Class I, Class IIA, IIB, etc. Indicate if this is a __Condition or __Intervention Final Class of recommendation: __Class I-Definitely Recommended __Class IIa-Acceptable & Useful; good evidence X Class IIb-Acceptable & Useful; fair evidence __Class III – Not Useful; may be harmful __Indeterminate-minimal evidence or inconsistent
REVIEWER’S PERSPECTIVE AND POTENTIAL CONFLICTS OF INTEREST: Briefly summarize your professional background, clinical specialty, research training, AHA experience, or other relevant personal background that define your perspective on the guideline proposal. List any potential conflicts of interest involving consulting, compensation, or equity positions related to drugs, devices, or entities impacted by the guideline proposal. Disclose any research funding from involved companies or interest groups. State any relevant philosophical, religious, or cultural beliefs or longstanding disagreements with an individual. I'm a pediatric intensivist and my main conflict of interest is that I was the Chair of the AHA Peds Resuscitation Committee in 1999-2000 and a major participant in developing this particular pediatric resuscitation guideline. In addition, my animal work has focused on the risks and benefits of chest compression-only CPR in VF and asphyxial models.
REVIEWER’S FINAL COMMENTS AND ASSESSMENT OF BENEFIT / RISK: Summarize your final evidence integration and the rationale for the class of recommendation. Describe any mismatches between the evidence and your final Class of Recommendation. “Mismatches” refer to selection of a class of recommendation that is heavily influenced by other factors than just the evidence. For example, the evidence is strong, but implementation is difficult or expensive; evidence weak, but future definitive evidence is unlikely to be obtained. Comment on contribution of animal or mechanical model studies to your final recommendation. Are results within animal studies homogeneous? Are animal results consistent with results from human studies? What is the frequency of adverse events? What is the possibility of harm? Describe any value or utility judgments you may have made, separate from the evidence. For example, you believe evidence-supported interventions should be limited to in-hospital use because you think proper use is too difficult for pre-hospital providers. Please include relevant key figures or tables to support your assessment. This updated literature review continues to support the guideline and commentary from the Guidelines 2000 document (see below). The differential recommendations for children vs adults continue to emanate from the fact that most pediatric 09a826193e718c0be8c6b2f6224b6745.doc Page 6 of 23
arrests are precipitated by respiratory failure and shock rather than VF or other primary cardiac problem. Although respiratory failure is the most common cause of cardiac arrest, etiology-based therapy would make more sense pathophysiologically and, therefore therapeutically. Both children and adults with sudden collapse due to VF or VT need prompt defibrillation or prompt, forceful, uninterrupted chest compressions while awaiting defibrillation. In contrast, definitive care for asphyxial arrests (precipitated by acute respiratory illness, upper airway obstruction, near-drowning, etc) in both children and adults should be prompt ABC’s (rescue breathing and chest compressions).
Data included in Guidelines 2000
The strongest data for this recommendation come from limited pediatric clinical data, extrapolated adult data, and two animal studies. In the original description of closed-chest cardiac massage (Kouwenhoven ’60), 17 of the 20 patients did not have VF, 7/20 did not receive any rescue breathing, and at least 3 were children (the data reported are somewhat sketchy). All 20 attained ROSC, 14 were discharged alive “without neurological damage.” At least one well-described child survived with good outcome after CC-only CPR for an asphyxia-precipitated cardiac arrest.
In a prospective controlled trial, Hallstrom ’00 demonstrated that dispatcher-assisted CPR was at least as good with chest compressions (CC) only compared with CC plus mouth-to-mouth (MTM). With CC alone 35/240 (14.6%) survived to hosp discharge vs 29/278 (10.4%) with CC plus MTM (P=0.18). 44% and 42% had VF, respectively. CC was at least as good as CC+V (probably in part because of the difficulty teaching MTM rescue breathing over the phone); numerous other investigations have demonstrated that telephone-directed bystander CPR results in superior outcomes compared with no bystander CPR.
There are many animal studies demonstrating that CC is as good as CC+ventilation (V) for VF. However, most pertinent to the issue at hand are two animal studies specifically addressing the issue of CC vs CC+V in asphyxial models. In one controlled trial comparing chest compressions alone versus chest compressions plus assisted ventilation vs ventilation alone vs no simulated bystander CPR for 8 minutes after induction of asphyxial cardiac arrest (with loss of aortic pulsations), only chest compressions plus assisted ventilations improved 24-hour neurologically normal survival compared to no bystander CPR (7/10 CC+V pigs vs 1/14 CC pigs vs 1/7 V pigs vs 0/8 control pigs) (Berg CCM ‘99). However, at an earlier stage of the asphyxial process, CC and V each independently improved outcome from an asphyxial pulseless cardiac arrest (Berg Circ ‘00). In the latter experiment, the endotracheal tube was clamped until the aortic systolic blood pressure was <50mmHg, and simulated bystander CPR was again provided for 8 minutes until simulated paramedic arrival. 24-hour survival was attained in 8/10 CC+V animals, 5/10 CC animals, 6/10 V animals, and 0/10 no bystander CPR animals. Outcomes were statistically superior in all 3 experimental groups compared to the control group. Nearly all of the surviving animals in both experiments attained return of spontaneous circulation during the first minutes of simulated bystander CPR (prior to simulated paramedic arrival). These findings are consistent with the clinical studies above. Moreover, they support the recommendation that bystander CPR with chest compressions and assisted ventilation is the treatment of choice for asphyxial cardiac arrest, but either alone is better than no resuscitation attempt.
Adult out-of-hospital (OOH) arrest studies routinely demonstrate that bystander-initiated CPR improves survival to hospital discharge by 2-3-fold. Some of these studies have demonstrated that only good quality CPR improves outcome (Cummins’91, Wik’94, Gallagher’95, Bossaert’89, von Hoeyweghen’93), but the outcomes after poor quality CPR are no worse than that with no CPR. In addition, adult out-of-hospital (OOH) arrest studies consistently demonstrate that chest compression-only CPR results in similar outcomes compared with standard chest compression plus rescue breathing CPR. A comprehensive study in Belgium during the 1980s prospectively evaluated 3053 OOH cardiac arrests (Bossaert’89, von Hoeyweghen’93). Long-term survival occurred in 17/116 (15%) cardiac arrest victims treated with good quality chest compressions only-CPR, 71/443 (16%) treated with good quality chest compressions and mouth-to-mouth ventilation, 123/2055 (6%) with no bystander CPR, and 2/47 (4%) with MTM ventilation only (both good CC groups differed from the no CPR group and the ventilation only group [P<0.001], but not from each other).
Finally, outcomes are dismal when the child is still in cardiac arrest by the time EMS providers arrive, but excellent outcomes are typical when the child is successfully resuscitated prior to EMS provider arrival (Mogayzel ’95, Sirbaugh ’99, Hickey ’95, Nichter ’89, Friesen ’82, Biggart ’90, Christensen ’97, Fiser ’87, Quan ’90, Kemp ’91, Kyriacou ’94, Schindler ’96, Kuisma ’95, Young ’99). Successful resuscitation techniques have included mouth-to-mouth rescue breathing alone, chest compressions alone, and chest compressions plus mouth-to-mouth rescue breathing; however, authors have retrospectively questioned whether these patients needed resuscitation.
New data since 2000 09a826193e718c0be8c6b2f6224b6745.doc Page 7 of 23
Animal studies since 2000 (Berg ’01, Kern ’02, Sanders’02) provide further support to the value of chest compression-only CPR for VF. In addition, two of these studies further elucidate the importance of continuous, forceful chest compressions; and conversely the dangers inherent in chest compression interruptions (Berg ’01, Kern ’02).
Two OOH pediatric arrest studies also demonstrate that excellent outcomes occur when the child is successfully resuscitated prior to EMS provider arrival (Suominem ’02, Li ’99). They also suggest that these patients may not have initially been in full cardiac arrest, the typical assumption when prompt CPR is effective.
Holmberg ‘01 reported various factors modifying the effect of bystander CPR on survival from 9877 arrests in the Swedish Cardiac arrest registry. They again demonstrated that 1-month survival improved with bystander CPR compared with no bystander CPR (8.2% vs 2.5%; odds ratio 3.5, 95%CI 2.9-4.3). They also reported that “partial CPR” (chest compressions alone or MTM ventilation alone) was worse than “complete CPR,” chest compressions and MTM ventilation (46/902 [5.1%] vs 176/1812[9.7%], P<0.0001. However, most of that difference could be attributed to the poor outcome with ventilation only. Complete CPR resulted in 176/1812 [9.7%] 1-month survivors, CC-only 19/278 [6.8%], and MTM only 27/620 [4.3%] (MTM vs complete P<0.001, CC only vs complete P=0.12, both by my post-hoc chi-square analysis).
Waalewijn’01 also reported outcomes after bystander CPR in Amsterdam. They noted survival to hospital discharge in 61/437 (14%) after CC plus MTM, 6/41 (15%) after CC only, 1/15 (7%) after MTM only, and 26/429 (6%) after no bystander CPR [no bystander CPR vs MMV, P=0.97; no bystander CPR vs CC only, P=0.04; no bystander CPR vs MMV plus CC, P<0.005; CC only vs MMV plus CC, P=0.97; all by my post-hoc chi square analysis].
“ Guidelines 2000: Compression-only CPR
Clinical studies have established that outcomes are dismal when the pediatric victim of cardiac arrest remains in cardiac arrest until the arrival of EMS personnel. By comparison, excellent outcomes are typical when the child is successfully resuscitated before the arrival of EMS personnel.9,15,16,40,46,249-252 Some of these patients were apparently resuscitated with “partial CPR,” consisting of chest compressions or rescue breathing only. In some published surveys, healthcare providers have expressed reluctance to perform mouth-to-mouth ventilation for unknown victims of cardiopulmonary arrest.253-255 This reluctance has also been expressed by some surveyed potential lay rescuers,40,256 although reluctance has not been expressed about resuscitation of infants and children. The effectiveness of “compression-only” or “no ventilation” CPR has been studied in animal models of acute VF sudden cardiac arrest , in some epidemiological studies of adult out-of-hospital cardiac arrest (ie, some bystanders provided chest compression-only CPR), and in a clinical trial for telephone-assisted CPR in adult out-of-hospital cardiac arrest. Some evidence in adult animal models and limited adult clinical trials suggests that positive-pressure ventilation may not be essential during the initial 6 to 12 minutes of an acute VF cardiac arrest.33,257-263 Spontaneous gasping and passive chest recoil may provide some ventilation during that time without the need for active rescue breathing.259,260,262 In addition, cardiac output during chest compression is only approximately 25% of normal, so the ventilation necessary to maintain optimal ventilation-perfusion relationships may be minimal.264,265 However, it does not appear that these observations can be applied to resuscitation of infants and children. Well-controlled animal studies have established that simulated bystander CPR with chest compressions plus rescue breathing is superior to chest compressions alone or rescue breathing alone for asphyxial cardiac arrest and severe asphyxial hypoxic-ischemic shock (pulseless cardiac arrests). However, chest compression–only CPR and rescue breathing–only CPR have been shown to be effective early in animal models of pulseless arrest, and the application of either of these forms of “partial CPR” was found to be superior to no bystander CPR. Preliminary evidence suggests that both chest compressions and active rescue breathing are necessary for optimal resuscitation of the asphyxial arrests most commonly encountered in children.223,224 For pediatric cardiac arrest, the lay rescuer should provide immediate chest compressions and rescue breathing. If the lay rescuer is unwilling or unable to provide rescue breathing or chest compressions, it is better to provide either chest compressions or rescue breathing than no bystander CPR (Class IIb).” 09a826193e718c0be8c6b2f6224b6745.doc Page 8 of 23
Preliminary draft/outline/bullet points of Guidelines revision: Include points you think are important for inclusion by the person assigned to write this section. Use extra pages if necessary.
Publication: Chapter: Pages:
Topic and subheading: The previous Guidelines statement is well written and does not need to be changed, unless we wish to address the etiology-based CPR issue-----it could be argued that the approach for a child with a witnessed sudden collapse and no signs of circulation should be to call first (or use an AED, if available) and then focus on forceful, uninterrupted chest compressions.
The Suominem ’02 and Li ’99 refs can be added after the 2nd sentence quoted above. In the last sentence of that 1st paragraph, we could add the Japanese study indicating that MTM rescue breathing is a barrier to CPR (Shibata ’00).
Berg ’01, Kern ’02, and Sanders’02 can be added after the 2nd sentence of the next paragraph. In addition, after that sentence we could add that “Forceful, uninterrupted chest compressions are necessary for adequate myocardial, cerebral, and systemic perfusion, and, therefore, a critical component of effective CPR (refs Berg ’01, Kern ’02, Yu Circ ‘02).”
Holmberg ’01 and Waalewijn’01 can be added to the refs supporting CC only CPR as being effective (1st sentence, 2nd paragraph)
Attachments: . Bibliography in electronic form using the Endnote Master Library. It is recommended that the bibliography be provided in annotated format. This will include the article abstract (if available) and any notes you would like to make providing specific comments on the quality, methodology and/or conclusions of the study. 09a826193e718c0be8c6b2f6224b6745.doc Page 9 of 23
Citation List
Citation Marker Full Citation* Kouwenhoven, 1960 Kouwenhoven WB, Jude JR, Knickerbocker GG. Closed-chest cardiac massage. JAMA 1960;173:1064-1067. No abstract LOE:5 Mogayzel, 1995 Mogayzel C, Quan L, Graves JR, Tiedeman D, Fahrenbruch C, Herndon P. Out-of-hospital ventricular fibrillation in children and adolescents: causes and outcomes. Ann Emerg Med 1995;25(4):484-491. STUDY OBJECTIVE: To compare causes and outcomes of patients younger than 20 years with an initial rhythm of ventricular fibrillation versus asystole and pulseless electrical activity. DESIGN: Retrospective cohort study. SETTING: Urban/suburban prehospital system. PARTICIPANTS: Pulseless, nonbreathing patients less than 20 years who underwent out- of- hospital resuscitation. Patients with lividity or rigor mortis or who were less than 6 months old and died of sudden infant death syndrome were excluded. RESULTS: Ventricular fibrillation was the initial rhythm in 19% (29 of 157) of the cardiac arrests. Rhythm assessment was performed by the first responder in only 44% (69 of 157) of patients. All three rhythm groups were similar in age distribution, frequency of intubation (96%), and vascular access (92%); 93% of ventricular fibrillation patients were defibrillated. The causes of ventricular fibrillation were distributed evenly among medical illnesses, overdoses, drownings, and trauma, only two patients had congenital heart defects. Seventeen percent were discharged with no or mild disability, compared with 2% of asystole/pulseless electrical activity patients (P = .003). CONCLUSION: Ventricular fibrillation is not rare in child and adolescent prehospital cardiac arrest, and these patients have a better outcome than those with asystole or pulseless electrical activity. Earlier recognition and treatment of ventricular fibrillation might improve pediatric cardiac arrest survival rates. LOE:5
Sirbaugh, 1999 Sirbaugh PE, Pepe PE, Shook JE, Kimball KT, Goldman MJ, Ward MA, et al. A prospective, population-based study of the demographics, epidemiology, management, and outcome of out-of- hospital pediatric cardiopulmonary arrest [published correction appears in Ann Emerg Med. 1999;33:358]. Ann Emerg Med 1999;33(2):174-184. STUDY OBJECTIVEs: To perform a population-based study addressing the demography, epidemiology, management, and outcome of out-of-hospital pediatric cardiopulmonary arrest (PCPA). METHODS: Prospective, population-based study of all children (17 years of age or younger) in a large urban municipality who were treated by EMS personnel for apneic, pulseless conditions. Data were collected prospectively for 3(1/2) years using a comprehensive data collection tool and on-line computerized database. Each child received standard pediatric advanced cardiac life support. RESULTS: During the 3(1/2)-year period, 300 children presented with PCPA (annual incidence of 19. 7/100,000 at risk). Of these, 60% (n=181) were male (P =.0003), and 54% (n=161) were patients 12 months of age or younger (152,500 at risk). Compared with the population at risk (32% black patients, 36% Hispanic patients, 26% white patients), a disproportionate number of arrests occurred in black children (51.6% versus 26.6% in Hispanics, and 17% in white children; P <.0001). Over 60% of all cases (n=181) occurred in the home with family members present, and yet those family members initiated basic CPR in only 31 (17%) of such cases. Only 33 (11%) of the total 300 PCPA cases had a return of spontaneous circulation, and 5 of the 6 discharged survivors had significant neurologic sequelae. Only 1 factor, endotracheal intubation, was correlated positively with return of spontaneous circulation (P =.032). CONCLUSION: This population-based study underscores the need to investigate new therapeutic interventions for PCPA, as well as innovative strategies for improving the frequency of basic CPR for children. LOE:5 Hickey 1995 Hickey RW, Cohen DM, Strausbaugh S, Dietrich AM. Pediatric patients requiring CPR in the 09a826193e718c0be8c6b2f6224b6745.doc Page 10 of 23
prehospital setting. Ann Emerg Med 1995;25(4):495-501. STUDY OBJECTIVE: To determine the outcome of pediatric patients with prehospital cardiopulmonary arrest. DESIGN: Chart review of all patients with prehospital cardiopulmonary arrest who were subsequently admitted to a pediatric emergency department from January 1988 to January 1993. Cardiopulmonary arrest was considered to have been present if assisted ventilation and chest compressions were performed on an apneic, pulseless patient. SETTING: Pediatric ED. PARTICIPANTS: Pediatric patients in prehospital cardiac arrest. RESULTS: In all, 95 patients were identified. Fifty-six had initial hospital care at the pediatric ED (primary patients). The remaining 39 were transported to the pediatric ED after initial care of another institution (secondary patients). Forty-one percent of patients were younger than 1 year. Most arrests were respiratory in origin; asystole was the most common dysrhythmia. Fifteen patients (27%) survived to discharge. Fourteen of the survivors had return of spontaneous circulation before ED arrival. Thirty-three patients were in arrest on ED arrival; in 16 (48%) of these, return of spontaneous circulation subsequently developed in the ED, and 1 survived to discharge. Two survivors, including the survivor with return of spontaneous circulation in the ED, had severe neurologic sequelae. Ten (26%) of the secondary patients survived. All survivors had return of spontaneous circulation before arrival in the ED. Two survivors had severe neurologic sequelae. CONCLUSION: Most successfully resuscitated pediatric arrest victims are resuscitated in the prehospital setting and do not suffer severe neurologic injury. Most patients who present to the ED in continued arrest and survive to discharge have severe neurologic injury. LOE:5 Nichter, 1989 Nichter MA, Everett PB. Childhood near-drowning: Is cardiopulmonary resuscitation always indicated. Crit Care Med 1989;17:993-995. LOE:5 Friesen, 1982 Friesen RM, Duncan P, Tweed WA, Bristow G. Appraisal of pediatric cardiopulmonary resuscitation. Can Med Assoc J 1982;126(9):1055-1058. Sixty-six patients more than 30 days and less thant 16 years of age suffering an unexpected cardiac arrest in an 18-month period were included in a study of resuscitative measures in children. Six children survived to be discharged from hospital. Respiratory disease accounted for most (29%) of the cardiac arrests, but it also had the most favourable prognosis, 21% of the 19 patients surviving. None of the patients survived whose cardiac arrest was secondary to sepsis or trauma, even when the resuscitative efforts were initially successful. Only 1 of the 41 patients who had a cardiac arrest outside of hospital survived, and only 1 of the 34 patients who presented with asystole survived, and then with considerable damage to the central nervous system. The interval between cardiac arrest and application of basic life support was substantially shorter among the survivors. Also, most of the survivors did not present with asystole. The results of this study suggest that survival among resuscitated children is no better than that among adults but can be improved with early recognition and monitoring of children at risk. earlier application of basic and advanced life support, improved education of medical and lay personnel, and further research into pediatric resuscitative techniques. LOE:5 Biggart, 1990 Biggart MJ, Bohn DJ. Effect of hypothermia and cardiac arrest on outcome of near-drowning accidents in children. J Pediatr 1990;117(pt 1)(2):179-183. We conducted a retrospective review of 55 near-drowning victims (mean age 4.75 years) admitted to the intensive care unit during a 5-year period, to determine the factors that may influence survival both before and after hospital admission. All patients who remained comatose after resuscitation received ventilation for an initial 24 hour period, after which an assessment of central nervous system injury was made. Intracranial pressure was not monitored, and barbiturate therapy was used only for seizure control. Thirty-seven children survived and 18 died; five survivors had profound neurologic damage resulting in a persistent vegetative state: the remaining 32 (58%) survived intact. The major factors that separated intact survivors from those who died and from survivors in a persistent vegetative state were the presence of a detectable heartbeat and hypothermia (less than 33 degrees C) on examination in the emergency department. Thirteen patients with absent vital signs and a temperature of greater than 33 degrees C either died or survived in a persistent vegetative state. Fourteen patients had a combination of absent vital signs 09a826193e718c0be8c6b2f6224b6745.doc Page 11 of 23
and hypothermia and were resuscitated; eight died, two survived in a persistent vegetative state, and four survived intact. All intact survivors had been submerged in cold water for prolonged periods, and all underwent prolonged cardiopulmonary resuscitation. All patients with a detectable pulse, regardless of temperature, survived without neurologic sequelae. The 58% intact survival rate in this series compares favorably with the 50% we reported previously when high-dose barbiturate therapy and hypothermia were used to control intracranial pressure; at the same time, the number of survivors with a persistent vegetative state has been reduced by 50%. We conclude that prolonged in-hospital resuscitation and aggressive treatment of near-drowning victims who initially have absence of vital signs and are not hypothermic either results in eventual death or increases the number of survivors with a persistent vegetative state. LOE:5 Christensen, 1997 Christensen DW, Jansen P, Perkin RM. Outcome and acute care hospital costs after warm water near drowning in children. Pediatrics 1997;99:715-721. LOE:5 Fiser, 1987 Fiser DH, Wrape V. Outcome of cardiopulmonary resuscitation in children. Pediatr Emerg Care 1987;3(4):235-238. A study was undertaken in order to identify factors correlated with the outcome of pediatric cardiopulmonary resuscitation (CPR). A total of 35 children who experienced a total of 41 cardiopulmonary arrests were included. Sixteen of 41 patients (39%) could not be resuscitated; 16/41 (39%) were resuscitated temporarily but did not survive to discharge; 9/41 (22%) survived to discharge. Patients arresting outside the hospital who received early basic CPR at the scene were significantly more likely to be resuscitated, at least temporarily, than those who did not (8/8 vs 5/11; P = 0.02). A statistically significant difference in outcome was also demonstrated between patients with an initial arterial blood pH greater than 7.0 and those with an initial arterial blood pH less than 7.0 (P less than 0.05). We conclude that an initial arterial blood pH less than 7.0 predicts a poor outcome from cardiopulmonary arrest in children. Access to early basic CPR may improve the initial pH and the ability of the patient to be resuscitated. LOE:5 Quan, 1990 Quan L, Wentz KR, Gore EJ, Copass MK. Outcome and predictors of outcome in pediatric submersion victims receiving prehospital care in King County, Washington. Pediatrics 1990;86(4):586-593. Predictors of outcome in pediatric submersion victims treated by Seattle and King County's prehospital emergency services were studied. Victims less than 20 years old were identified from hospital admissions and paramedic and medical examiners' reports. The proportion of fatal or severe outcomes in patients were compared with various risk factors. Of 135 patients, 45 died and 5 had severe neurologic impairment. A subset of 38 victims found in cardiopulmonary arrest had a 32% survival rate, with 67% of survivors unimpaired or only mildly impaired. The two risk factors that occurred most commonly in victims who died or were severely impaired were submersion duration greater than 9 minutes (28 patients) and cardiopulmonary resuscitation duration longer than 25 minutes (20 patients). Both factors were ascertained in the prehospital phase of care. Submersion duration was associated with a steadily increasing risk of severe or fatal outcomes: 10% risk (7/67) for 0 to 5 minutes, 56% risk (5/9) for 6 to 9 minutes, 88% risk (21/25) for 10 to 25 minutes, 100% risk (4/4) for greater than 25 minutes. None of 20 children receiving greater than 25 minutes of cardiopulmonary resuscitation escaped death or severe neurologic impairment. Our rates for saving all victims, particularly victims in cardiopulmonary arrest, are considerably higher than has been reported before the children. Prompt prehospital advanced cardiac life support is the most effective means of medical intervention for the pediatric submersion victim. Prehospital information provided the most valuable predictors of outcome. LOE:5 Kemp, 1991 Kemp AM, Sibert JR. Outcome in children who nearly drown: a British Isles study. BMJ 1991;302(6782):931-933. OBJECTIVE--To determine the outcome in nearly drowned children in the British Isles and identify factors that might predict a poor prognosis. DESIGN--Study of drowned and of nearly drowned children aged less than or equal to 14. Information on nearly drowned children admitted to 09a826193e718c0be8c6b2f6224b6745.doc Page 12 of 23
hospital obtained from consultant paediatricians returning monthly notification cards through the British Paediatric Surveillance Unit. Information on drowned children obtained from Office of Population Censuses and Surveys and other national epidemiological offices. SETTING--British Isles, 1988 and 1989. SUBJECTS--330 children who had confirmed submersion incidents. 142 died before admission to hospital and 188 children were admitted after nearly drowning. MAIN OUTCOME MEASURES--Death, full recovery, or degree of handicap after near drowning and signs on admission to hospital. RESULTS--All of the children who were conscious on admission fully recovered. Of the 64 children unconscious on admission, 31 had normally reactive pupils and all but three (all of whom had severe preexisting neurological disease) recovered fully. Of the 33 children with fixed dilated pupils on admission, 10 fully recovered, 13 died, and 10 had severe neurological deficit. Spontaneous respiratory effect on admission was associated with normal survival. Pupils that remained dilated six hours after admission and fits continuing 24 hours after admission predicted a poor outcome. CONCLUSION--Children can survive normally after near drowning in the British Isles, particularly if they have been hypothermic. Resuscitation should not be abandoned in nearly drowned children until they have been rewarmed. LOE:5 Kyriacou, 1994 Kyriacou DN, Arcinue EL, Peek C, Kraus JF. Effect of immediate resuscitation on children with submersion injury. Pediatrics 1994;94(pt 1)(2):137-142. STUDY OBJECTIVE. To determine the effect of immediate resuscitative efforts on the neurological outcome of children with submersion injury. DESIGN. A case-control study was designed to determine if immediate resuscitation by rescuers or bystanders reduces the frequency of severe neurological damage or death in children with a documented submersion event. Logistic regression was used calculate an adjusted odds ratio. PARTICIPANTS. The study group consisted of 166 children, aged zero to 14 years, having a submersion event during May 1984 through August 1992, and admitted through various emergency departments to Huntington Memorial Hospital in Pasadena, California. MEASUREMENTS AND MAIN RESULTS. All study subjects had an observed and documented episode of apnea at the time of submersion. Outcomes were evaluated on the basis of neurological impairment or death. Exposure was verified from historical accounts of postsubmersion events provided by family, friends, and/or paramedical personnel. The study factors included age and gender, duration of submersion, hypothermia, presence of apnea, resuscitative efforts, and clinical outcome. Children with a good outcome were 4.75 (adjusted odds ratio (OR)) times more likely to have a history of immediate resuscitation than children with poor outcome (95% confidence interval: 3.44 < OR < 6.06, P = .0001). Various types of resuscitative efforts and potential confounding factors were also evaluated. CPR and mouth-to-mouth resuscitation were the most effective types for the prevention of death or severe anoxic encephalopathy. CONCLUSION. Immediate resuscitation before the arrival of paramedical personnel is associated with a significantly better neurological outcome in children with submersion injury. LOE:5 Schindler, 1996 Schindler MB, Bohn D, Cox PN, McCrindle BW, Jarvis A, Edmonds J, et al. Outcome of out-of- hospital cardiac or respiratory arrest in children. N Engl J Med 1996;335(20):1473-1479. BACKGROUND: Among adults who have a cardiac arrest outside the hospital, the survival rate is known to be poor. However, less information is available on out-of-hospital cardiac arrest among children. This study was performed to determine the survival rate among children after out- of-hospital cardiac arrest and to identify predictors of survival. METHODS: We reviewed the records of 101 children (median age, two years) with apnea or no palpable pulse (or both) who presented to the emergency department at the Hospital for Sick Children in Toronto. The characteristics of the patients and the outcomes of illness were analyzed. We assessed the functional outcome of the survivors using the Pediatric Cerebral and Overall Performance Category scores. RESULTS: Overall, there was a return of vital signs in 64 of the 101 patients; 15 survived to discharge from the hospital, and 13 were alive 12 months after discharge. Factors that predicted survival to hospital discharge included a short interval between the arrest and arrival at the hospital, a palpable pulse on presentation, a short duration of resuscitation in the emergency department, and the administration of fewer doses of epinephrine in the emergency department. No patients who required more than two doses of epinephrine or resuscitation for longer than 20 minutes in the emergency department survived to hospital discharge. The survivors who were neurologically normal after arrest had had a respiratory arrest only and were resuscitated within five minutes after 09a826193e718c0be8c6b2f6224b6745.doc Page 13 of 23
arrival in the emergency department. Of the 80 patients who had had a cardiac arrest, only 6 survived to hospital discharge, and all had neurologic sequelae. CONCLUSIONS: These results suggest that out-of-hospital cardiac arrest among children has a very poor prognosis, especially when efforts at resuscitation continue for longer than 20 minutes and require more than two doses of epinephrine. LOE:5 Kuisma, 1995 Kuisma M, Suominen P, Korpela R. Paediatric out-of-hospital cardiac arrests: epidemiology and outcome. Resuscitation 1995;30(2):141-150. OBJECTIVE: To determine the epidemiology and aetiology of out-of- hospital paediatric cardiac arrest and the outcome of resuscitation and to apply the Utstein template for the paediatric cardiac arrest population. DESIGN: Retrospective cohort study. SETTING: A middle-sized urban city (population 516,000) served by a single emergency medical services (EMS) system. PATIENTS: 79 consecutive paediatric (age under 16 years) prehospital cardiac arrest patients between January 1, 1985 and December 31, 1994. No patient was excluded. INTERVENTION: Advanced paediatric life support according to the recommendations of American Heart Association. MAIN OUTCOME MEASURES: Survival from cardiac arrest to discharge and factors associated with favourable outcome defined as alive 1 year after discharge with Bloom category I or II. RESULTS: 79 patients had cardiac arrest. The incidence of paediatric out-of- hospital cardiac arrest and sudden unexpected out-of-hospital death was 9.8 and 8.9/100,000/inhabitants aged under 16, respectively. The mean age was 2.9 years, 72.2% were under 18 months. SIDS was the leading cause of cardiac arrest followed by trauma, airway related cardiac arrest and (near)drowning. Fifty-two patients were considered for resuscitation in whom asystole was the most common initial rhythm (78.9%) followed by pulseless electrical activity (13.5%) and ventricular fibrillation (3.8%). Resuscitation was attempted in 34 patients. The overall survival rate was 9.6%, for attempted resuscitation 14.7%, for attempted resuscitation when cardiac arrest was witnessed 25.0% and for attempted resuscitation with witnessed arrest of cardiac origin 0%. Favourable outcome was registered in four of five survivors. Factors associated with favourable outcome were collapse in a public place, the near-drowning aetiology of arrest, bystander initiated CPR and short duration of resuscitation. Multivariate regression analysis showed no factor related to favourable outcome, but MICU time interval < 10 min was related with survival. Due to the retrospective nature of this study all core times could not be obtained. In spite of this, the Utstein template was applicable also in our paediatric cardiac arrest population. CONCLUSIONS: Survival from paediatric cardiac arrest has remained low. The overall survival rate was 9.6%, survival after attempted resuscitation 14.7% and 0% when resuscitation was attempted in witnessed arrest of cardiac origin. Asystole was the most common initial rhythm and the four leading causes for cardiac arrest were SIDS, trauma, airway related arrest and (near)drowning. The Utstein template adopted for adult out-of-hospital cardiac arrests was was found applicable also in paediatric cardiac arrests. LOE:5 Young, 1999 Young KD, Seidel JS. Pediatric cardiopulmonary resuscitation: a collective review. Ann Emerg Med 1999;33(2):195-205. Little information is available about the effects of CPR in children, although it is known that the outcomes are dismal. Examples of unanswered questions include which advanced life support (ALS) procedures should be performed out-of-hospital, whether high-dose epinephrine improves survival, and the true prevalence of ventricular fibrillation as a presenting rhythm. Children differ from adults as to the cause and pathophysiology of cardiopulmonary arrest, but prehospital EMS and hospital resuscitation teams were initially designed for the care of adults. Because pediatric cardiopulmonary arrest is rare, prospective data are difficult to gather, and there are few large published studies. The purpose of this collective review was to review the current body of knowledge regarding survival rates and outcomes in pediatric CPR and, based on this review, to outline a course for future research. LOE:5 Suominem, 2002 Suominen P, Baillie C, Korpela R, Rautanen S, Ranta S, Olkkola KT. Impact of age, submersion time and water temperature on outcome in near-drowning. Resuscitation 2002;52(3):247-54. BACKGROUND: Because children have less subcutaneous fat, and a higher surface area to 09a826193e718c0be8c6b2f6224b6745.doc Page 14 of 23
body weight ratio than adults, it has been suggested that children cool more rapidly during submersion, and therefore have a better outcome following near-drowning incidents. AIM OF THE STUDY: To study the impact of age, submersion time, water temperature and rectal temperature in the emergency room on outcome in near-drowning. MATERIAL AND METHODS: This retrospective study included all near-drowning victims admitted to the intensive care units of Helsinki University Central Hospital after successful cardiopulmonary resuscitation between 1985 and 1997. RESULTS: There were 61 near-drowning victims (age range: 0.5-60 years, median 29 years). Males were in the majority (40), and 26 were children (<16 years). The median water temperature was 17 degrees C (range: 0-33 degrees C). The median submersion time for the 43 survivors (70%) was 10 min (range: 1-38 min). Intact survivors and those with mild neurological disability (n=26, 43%) had a median submersion time of 5 min (range: 1-21 min). In non-survivors the median submersion time was 16 min (range: 2-75 min). Submersion time was the only independent predictor of survival in linear regression analysis (P<0.01). Patient age, water temperature and rectal temperature in the emergency room were not significant predictors of survival. CONCLUSIONS: Although submersion time is usually an estimate, it is the best prognostic factor after a near drowning incident. Children did not have a better outcome than adults. LOE:5 Li, 1999 Li G, Tang N, DiScala C, Meisel Z, Levick N, Kelen GD. Cardiopulmonary resuscitation in pediatric trauma patients: survival and functional outcome. J Trauma 1999;47(1):1-7. BACKGROUND: Although injury is the leading cause of cardiac arrests in children older than 1 year, few studies have examined the survival and functional outcome of cardiopulmonary resuscitation (CPR) in pediatric trauma patients. METHODS: A historical cohort of 957 trauma patients younger than 15 years who received CPR at the scene of injury or at the admitting hospital was constructed on the basis of the National Pediatric Trauma Registry. The rate of survival to discharge and factors related to survival were examined. Functional impairments were documented for surviving patients. RESULTS: The overall survival rate was 23.5%. With adjustment for the Injury Severity Score, the risk of fatality after CPR increased for children with systolic blood pressure below 60 mm Hg at admission (odds ratio [OR] 24.5, 95% confidence interval [CI] 8.6- 69.3), for those who were comatose at admission (OR, 4.7; 95% CI, 1.9-11.6), for those with penetrating injury (OR, 4.4; 95% CI, 1.5-13.3), and for those with CPR initiated at the hospital (OR, 2.4; 95% CI, 1.5-3.9). Surviving patients stayed in hospitals for an average of 24.3 days; at discharge, 64% had at least one impairment in the functional activities of daily living. CONCLUSIONS: Survival outcome of CPR in pediatric trauma patients appears to be comparable to that reported in adults of mixed arrest causes. Future research needs to identify factors underlying the excess mortality associated with penetrating trauma. LOE:5 Hallstrom, 2000 Hallstrom A, Cobb L, Johnson E, Copass M. Cardiopulmonary resuscitation by chest compression alone or with mouth-to-mouth ventilation. N Engl J Med 2000;342(21):1546-1553. BACKGROUND: Despite extensive training of citizens of Seattle in cardiopulmonary resuscitation (CPR), bystanders do not perform CPR in almost half of witnessed cardiac arrests. Instructions in chest compression plus mouth-to-mouth ventilation given by dispatchers over the telephone can require 2.4 minutes. In experimental studies, chest compression alone is associated with survival rates similar to those with chest compression plus mouth-to-mouth ventilation. We conducted a randomized study to compare CPR by chest compression alone with CPR by chest compression plus mouth-to-mouth ventilation. METHODS: The setting of the trial was an urban, fire-department-based, emergency-medical-care system with central dispatching. In a randomized manner, telephone dispatchers gave bystanders at the scene of apparent cardiac arrest instructions in either chest compression alone or chest compression plus mouth-to-mouth ventilation. The primary end point was survival to hospital discharge. RESULTS: Data were analyzed for 241 patients randomly assigned to receive chest compression alone and 279 assigned to chest compression plus mouth-to-mouth ventilation. Complete instructions were delivered in 62 percent of episodes for the group receiving chest compression plus mouth-to-mouth ventilation and 81 percent of episodes for the group receiving chest compression alone (P=0.005). Instructions for compression required 1.4 minutes less to complete than instructions for compression plus mouth-to- mouth ventilation. Survival to hospital discharge was better among patients assigned to chest compression alone than among those assigned to chest compression plus mouth-to-mouth 09a826193e718c0be8c6b2f6224b6745.doc Page 15 of 23
ventilation (14.6 percent vs. 10.4 percent), but the difference was not statistically significant (P=0.18). CONCLUSIONS: The outcome after CPR with chest compression alone is similar to that after chest compression with mouth-to-mouth ventilation, and chest compression alone may be the preferred approach for bystanders inexperienced in CPR. LOE:7 Bossaert, 1989 Bossaert L, Van Hoeyweghen R. Bystander cardiopulmonary resuscitation (CPR) in out-of-hospital cardiac arrest. The Cerebral Resuscitation Study Group. Resuscitation 1989;17(suppl):S55-S69. Prevalence of bystander CPR and effect on outcome has been evaluated on 3053 out-of- hospital cardiac arrest (CA) events. Bystander CPR was performed in 33% of recorded cases (n = 998) by lay people in 406 cases (family members 178, other lay people 228) and by bystanding health care workers in 592 cases (nurses 86, doctors 506). Family members and lay people mainly applied CPR in younger CA victims at public places, roadside or at the working place. Sudden infant death syndrome (SIDS) and drowning are highly represented. Health care workers performed CPR mainly in older patients, at public places or at the roadside and especially in case of cardiac or respiratory origin. CA caused by trauma/exsanguination and intoxication/metabolic origin received less bystander CPR (23% resp. 22%). Cardiac arrests receiving bystander CPR are more frequently witnessed and have a shorter access time to the emergency medical service (EMS) system and shorter response time of basic life support (BLS). Advanced life support (ALS) response time is significantly longer. In witnessed arrests of cardiac origin receiving bystander CPR a significantly better late survival was observed. In non- witnessed arrests of cardiac origin early and late survival are significantly higher in patients receiving bystander CPR. In CA events where response time of ALS exceeds 8 min, the beneficial effect of bystander CPR is most significant. Furthermore no deleterious effect of bad technique or inefficient bystander CPR can be demonstrated. LOE:7 van Hoeyweghen, 1993 Van Hoeyweghen RJ, Bossaert LL, Mullie A, Calle P, Martens P, Buylaert WA, et al. Quality and efficiency of bystander CPR. Belgian Cerebral Resuscitation Study Group. Resuscitation 1993;26(1):47-52. Incorrectly performed bystander CPR might compromise survival of the cardiac arrest patient. We therefore evaluated the outcome in 3306 out- of-hospital primary cardiac arrests of which 885 received bystander CPR. bystanders performed CPR correctly in 52%, incorrectly in 11%, 31% performed only external chest compressions (ECC) and 6% only mouth-to- mouth ventilation (MMV). The initial ECG in cases without bystander CPR was ventricular fibrillation in 28% (95% confidence interval: 27-30%); 45% (41-50%) and 39% (29-48%), respectively when bystander CPR was performed correctly or incorrectly; 43% (37-49%) when only ECC was applied and 22% (11-33%) when only MMV was practiced. Long term survival, defined as being awake 14 days after CPR, was 16% (13-19%) in patients with correct bystander CPR; 10% (7-14%) and 2% (0-9%), respectively when only ECC or only MMV was performed; 7% (6-8%) when no bystander was involved; 4% (0-8%) when bystander CPR was performed incorrectly. Bystander CPR might have a beneficial effect on survival by maintaining the heart in ventricular fibrillation by ECC. A negative effect of badly performed bystander CPR was not observed compared to cases which had not received bystander CPR. LOE:7 Homberg, 2001 Holmberg M, Holmberg S, Herlitz J. Factors modifying the effect of bystander cardiopulmonary resuscitation on survival in out-of-hospital cardiac arrest patients in Sweden. Eur Heart J 2001;22(6):511-519. AIM: To describe possible factors modifying the effect of bystander cardiopulmonary resuscitation on survival among patients suffering an out-of-hospital cardiac arrest. PATIENTS: A national survey in Sweden among patients suffering out-of-hospital cardiac arrest and in whom resuscitative efforts were attempted. Sixty per cent of ambulance organizations were included. DESIGN: Prospective evaluation. Survival was defined as survival 1 month after cardiac arrest. RESULTS: In all, 14065 reports were included in the evaluation. Of these, resuscitation efforts were attempted in 10966 cases, of which 1089 were witnessed by ambulance crews. The report deals with the remaining 9877 patients, of whom bystander cardiopulmonary resuscitation was attempted in 36%. Survival to 1 month was 8.2% among patients who received bystander cardiopulmonary resuscitation vs 2.5% among patients who did not receive it (odds ratio 3.5, 95% 09a826193e718c0be8c6b2f6224b6745.doc Page 16 of 23
confidence interval 2.9-4.3). The effect of bystander cardiopulmonary resuscitation on survival was related to: (1) the interval between collapse and the start of bystander cardiopulmonary resuscitation (effect more marked in patients who experienced a short delay); (2) the quality of bystander cardiopulmonary resuscitation (effect more marked if both chest compressions and ventilation were performed than if either of them was performed alone); (3) the category of bystander (effect more marked if bystander cardiopulmonary resuscitation was performed by a non- layperson); (4) interval between collapse and arrival of the ambulance (effect more marked if this interval was prolonged); (5) age (effect more marked in bystander cardiopulmonary resuscitation among the elderly); and (6) the location of the arrest (effect more marked if the arrest took place outside the home). CONCLUSION: The effect of bystander cardiopulmonary resuscitation on survival after an out-of-hospital cardiac arrest can be modified by various factors. Factors that were associated with the effect of bystander cardiopulmonary resuscitation were the interval between the collapse and the start of bystander cardiopulmonary resuscitation, the quality of bystander cardiopulmonary resuscitation, whether or not the bystander was a layperson, the interval between collapse and the arrival of the ambulance, age and the place of arrest. LOE:7 Waalewijn, 2001 Waalewijn RA, Tijssen JG, Koster RW. Bystander initiated actions in out-of-hospital cardiopulmonary resuscitation: results from the Amsterdam Resuscitation Study (ARRESUST). Resuscitation 2001;50(3):273-279. The objective of this study was to analyze the functioning of the first two links of the chain of survival: 'access' and 'basic cardiopulmonary resuscitation (CPR)'. In a prospective study, all bystander witnessed circulatory arrests resuscitated by emergency medical service (EMS) personnel, were recorded consecutively. Univariate differences in survival were calculated for various witnesses, the performance of basic CPR, the quality of CPR, the performers of CPR and the delays. A logistic regression model for survival was developed from all potential predictors of these first two links .From the 922 included patients, 93 survived to hospital discharge. In 21% of the cases, the witness did not immediately call 112, but first called others, resulting in a longer delay and a lower survival. Family members were frequent witnesses of the arrest (44%), but seldom started basic CPR (11%). Survival, when basic CPR performers were untrained and had no previous experience, was similar to that when no basic CPR was performed (6%). Not performing basic CPR, delay in basic CPR, the interval between basic CPR and EMS arrival, and being both untrained and inexperienced in basic CPR were independent predictors for survival. Basic CPR performed by persons trained a long time ago did not appear to have a negative influence on outcome, nor did basic CPR limited to chest compressions alone. The mere reporting that basic CPR has been performed does not describe adequately the actual value of basic CPR. The interval from collapse to initiation of basic CPR, and the training and experience of the performer must be taken into account. Policy makers for basic CPR training should focus on partners of the patients, who are most likely witness of an arrest. LOE:7 Cummins 1991 Cummins RO, Chamberlain DA, Abramson NS, Allen M, Baskett P, Becker L, et al. Recommended guidelines for uniform reporting of data from out-of-hospital cardiac arrest: the Utstein Style. Task Force of the American Heart Association, the European Resuscitation Council, the Heart and Stroke Foundation of Canada, and the Australian Resuscitation Council. Ann Emerg Med 1991;20(8):861-874. LOE:7 Wik, 1994 Wik L, Steen PA, Bircher NG. Quality of bystander cardiopulmonary resuscitation influences outcome after prehospital cardiac arrest. Resuscitation 1994;28(3):195-203. To evaluate the influence of quality of bystander cardiopulmonary resuscitation (CPR) on outcome in prehospital cardiac arrest we consecutively included patients with prehospital cardiac arrest treated by paramedics in a community run ambulance system in Oslo, Norway from 1985 to 1989. Good CPR was defined as palpable carotid or femoral pulse and intermittent chest expansion with inflation attempts. Outcome measure was hospital discharge rate. One hundred and forty-nine of 334 patients (45%) received bystander CPR. The discharge rate after good BCPR (23%) was higher than after no good BCPR (1%, P < 0.0005) or after no BCPR (6%, P < 0.0005). There was no difference between no good and no BCPR (P = 0.1114). There were no differences in paramedic response interval between the groups, but the mean interval from start of unconsciousness to 09a826193e718c0be8c6b2f6224b6745.doc Page 17 of 23
initiation of CPR (arrest-CPR interval) was significantly shorter in the group receiving good bystander CPR (2.5 min, 95% confidence interval (CI): 1.7-3.3 min) than no good CPR (6.6 min, CI: 5.2-8.0 min) or no bystander CPR (7.8 min, CI: 7.2-8.4 min). Bystanders started CPR more frequently in public than in the patient's home (58 vs. 34%, P < 0.0005). Good bystander CPR was associated with a shorter arrest-CPR interval and improved hospital discharge rate as compared to no good BCPR or no BCPR. LOE:7 Gallagher, 1995 Gallagher, E. J., G. Lombardi, et al. (1995). "Effectiveness of bystander cardiopulmonary resuscitation and survival following out-of-hospital cardiac arrest." Jama 274(24): 1922-5.
OBJECTIVE--To examine the independent relationship between effectiveness of bystander cardiopulmonary resuscitation (CPR) and survival following out-of- hospital cardiac arrest. DESIGN--Prospective observational cohort. SETTING-- New York City. PARTICIPANTS--A total of 2071 consecutive out-of-hospital cardiac arrests meeting Utstein criteria. INTERVENTION--Trained prehospital personnel assessed the quality of bystander CPR on arrival at the scene. Satisfactory execution of CPR required performance of both adequate compressions and ventilations in conformity with current American Heart Association guidelines. MAIN OUTCOME MEASURE--Adjusted association between CPR effectiveness and survival. Survival was defined as discharge from hospital to home. RESULTS--Outcome was determined on all members of the inception cohort--none were lost to follow-up. When the association between bystander CPR and survival was adjusted for effectiveness of CPR in the parent data set (N = 2071), only effective CPR was retained in the logistic model (adjusted odds ratio [OR] = 5.7; 95% confidence interval [CI], 2.7 to 12.2; P < . 001). Of the subset of 662 individuals (32%) who received bystander CPR, 305 (46%) had it performed effectively. Of these, 4.6% (14/305) survived vs 1.4% (5/357) of those with ineffective CPR (OR = 3.4; 95% CI, 1.1 to 12.1; P < .02). After adjustment for witness status, initial rhythm, interval from collapse to CPR, and interval from collapse to advanced life support, effective CPR remained independently associated with improved survival (adjusted OR = 3.9; 95% CI, 1.1 to 14.0; P < .04). CONCLUSION--The association between bystander CPR and survival in out-of-hospital cardiac arrest appears to be confounded by CPR quality. Effective CPR is independently associated with a quantitatively and statistically significant improvement in survival.
LOE:7 Shibata, 2000 Shibata K, Taniguchi T, Yoshida M, Yamamoto K. Obstacles to bystander cardiopulmonary resuscitation in Japan. Resuscitation 2000;44(3):187-193. OBJECTIVE: bystander cardiopulmonary resuscitation (CPR) is performed infrequently in Japan. We conducted this study to identify Japanese attitudes toward the performance of bystander CPR. METHODS: participants were asked about their willingness to perform CPR with varying scenarios and CPR techniques (mouth-to-mouth ventilation plus chest compression (MMV plus CC) versus chest compression alone (CC)). RESULTS: a total of 1302/1355 individuals completed the questionnaire, including high school students, teachers, emergency medical technicians, medical nurses, and medical students. About 2% of high school students, 3% of teachers, 26% of emergency medical technicians, 3% of medical nurses and 16% of medical students claimed they would 'definitely' perform MMV plus CC on a stranger. However, 21-72% claimed they would prefer the alternative of performing CC alone. Respondents claimed their unwillingness to perform MMV is not due to the fear of contracting a communicable disease, but the lack of confidence in their ability to perform CPR properly. CONCLUSION: in all categories of respondents, willingness to perform MMV plus CC for a stranger was disappointingly low. Better training in MMV together with teaching awareness that CC alone can be given should be instituted to maximize the number of potential providers of CPR in the community, even in communities where the incidence of HIV is very low. LOE:7 09a826193e718c0be8c6b2f6224b6745.doc Page 18 of 23
Berg, 1999 Berg RA, Hilwig RW, Kern KB, Babar I, Ewy GA. Simulated mouth-to-mouth ventilation and chest compressions (bystander cardiopulmonary resuscitation) improves outcome in a swine model of prehospital pediatric asphyxial cardiac arrest. Crit Care Med 1999;27(9):1893-1899. OBJECTIVE: To compare the efficacy of four methods of simulated single-rescuer bystander cardiopulmonary resuscitation (CPR) in a clinically relevant swine model of prehospital pediatric asphyxial cardiac arrest. DESIGN: Prospective, randomized study. SUBJECTS: Thirty-nine anesthetized domestic piglets. INTERVENTIONS: Asphyxial cardiac arrest was produced by clamping the endotracheal tubes of the piglets. For 8 mins of simulated bystander CPR, animals were randomly assigned to the following groups: group 1, chest compressions and simulated mouth-to-mouth ventilation (FI(O2) = 0.17, FI(CO2) = 0.04) (CC+V); group 2, chest compressions only (CC); group 3, simulated mouth-to-mouth ventilation only (V); and group 4, no CPR (control group). Standard advanced life support was then provided, simulating paramedic arrival. Animals that were successfully resuscitated received 1 hr of intensive care support and were observed for 24 hrs. MEASUREMENTS AND MAIN RESULTS: Electrocardiogram, aortic blood pressure, right atrial blood pressure, and end-tidal CO2 were monitored continuously until the intensive care period ended. Arterial and mixed venous blood gases were measured at baseline, 1 min after cardiac arrest, and 7 mins after cardiac arrest. Minute ventilation was determined during each minute of bystander CPR. Survival and neurologic outcome were determined. Twenty-four-hour survival was attained in eight of 10 group 1 (CC+V) piglets vs. three of 14 group 2 (CC) piglets (p < or = .01), one of seven group 3 (V) piglets (p < or = .05), and two of eight group 4 (control) piglets (p < or = .05). Twenty-four-hour neurologically normal survival occurred in seven of 10 group 1 (CC+V) piglets vs. one of 14 group 2 (CC) piglets (p < or = .01), one of seven group 3 (V) piglets (p < or = .05), and none of eight group 4 (control) piglets (p < or = .01). Arterial oxygenation and pH were markedly better during CPR in group 1 than in group 2. Within 5 mins of bystander CPR, six of 10 group 1 (CC+V) piglets attained sustained return of spontaneous circulation vs. only two of 14 group 2 (CC) piglets and none of the piglets in the other two groups (p < or = .05 for all groups). CONCLUSIONS: In this pediatric asphyxial model of prehospital single-rescuer bystander CPR, chest compressions plus simulated mouth-to-mouth ventilation improved systemic oxygenation, coronary perfusion pressures, early return of spontaneous circulation, and 24-hr survival compared with the other three approaches. LOE:6 Berg, 2000 Berg RA, Hilwig RW, Kern KB, Ewy GA. "Bystander" chest compressions and assisted ventilation independently improve outcome from piglet asphyxial pulseless "cardiac arrest". Circulation 2000;101(14):1743-1748. BACKGROUND: Bystander cardiopulmonary resuscitation (CPR) without assisted ventilation may be as effective as CPR with assisted ventilation for ventricular fibrillatory cardiac arrests. However, chest compressions alone or ventilation alone is not effective for complete asphyxial cardiac arrests (loss of aortic pulsations). The objective of this investigation was to determine whether these techniques can independently improve outcome at an earlier stage of the asphyxial process. METHODS AND RESULTS: After induction of anesthesia, 40 piglets (11.5+/- 0.3 kg) underwent endotracheal tube clamping (6.8+/-0.3 minutes) until simulated pulselessness, defined as aortic systolic pressure <50 mm Hg. For the 8-minute "bystander CPR" period, animals were randomly assigned to chest compressions and assisted ventilation (CC+V), chest compressions only (CC), assisted ventilation only (V), or no bystander CPR (control group). Return of spontaneous circulation occurred during the first 2 minutes of bystander CPR in 10 of 10 CC+V piglets, 6 of 10 V piglets, 4 of 10 CC piglets, and none of the controls (CC+V or V versus controls, P<0.01; CC+V versus CC and V combined, P=0.01). During the first minute of CPR, arterial and mixed venous blood gases were superior in the 3 experimental groups compared with the controls. Twenty-four-hour survival was similarly superior in the 3 experimental groups compared with the controls (8 of 10, 6 of 10, 5 of 10, and 0 of 10, P<0.05 each). CONCLUSIONS: Bystander CPR with CC+V improves outcome in the early stages of apparent pulseless asphyxial cardiac arrest. In addition, this study establishes that bystander CPR with CC or V can independently improve outcome. LOE:6 Berg, 1993 Berg RA, Kern KB, Sanders AB, Otto CW, Hilwig RW, Ewy GA. Bystander cardiopulmonary resuscitation. Is ventilation necessary? Circulation 1993;88(pt 1)(4):1907-1915. 09a826193e718c0be8c6b2f6224b6745.doc Page 19 of 23
BACKGROUND. Prompt initiation of bystander cardiopulmonary resuscitation (CPR) improves survival. Basic life support with mouth-to-mouth ventilation and chest compressions is intimidating, difficult to remember, and difficult to perform. Chest compressions alone can be easily taught, easily remembered, easily performed, adequately taught by dispatcher-delivered telephone instruction, and more readily accepted by the public. The principal objective of this study was to evaluate the need for ventilation during CPR in a clinically relevant swine model of prehospital witnessed cardiac arrest. METHODS AND RESULTS. Thirty seconds after ventricular fibrillation, swine were randomly assigned to 12 minutes of chest compressions plus mechanical ventilation (group A), chest compressions only (group B), or no CPR (group C). Standard advanced cardiac life support was then provided. Animals successfully resuscitated were supported for 2 hours in an intensive care setting, and then observed for 24 hours. All 16 swine in groups A and B were successfully resuscitated and neurologically normal at 24 hours, whereas only 2 of 8 group C animals survived for 24 hours (P < .001, Fisher's exact test). One of the 2 group C survivors was comatose and unresponsive. CONCLUSIONS. In this swine model of witnessed prehospital cardiac arrest, the survival and neurological outcome data establish that prompt initiation of chest compressions alone appears to be as effective as chest compressions plus ventilation and that both techniques of bystander CPR markedly improve outcome compared with no bystander CPR. LOE:6 Chandra, 1994 Chandra NC, Gruben KG, Tsitlik JE, Brower R, Guerci AD, Halperin HH, et al. Observations of ventilation during resuscitation in a canine model. Circulation 1994;90(6):3070-3075. BACKGROUND: Fear of infection limits the willingness of laymen to do cardiopulmonary resuscitation (CPR). This study assessed the time course of change in arterial blood gases during resuscitation with only chest compression (no ventilation) in an effort to identify the time for which ventilation could be deferred. METHODS AND RESULTS: Aortic pressures and arterial blood gases were monitored in seven 20- to 30-kg dogs in ventricular fibrillation (VF) at 2-minute intervals during chest compression alone (no ventilation) at 80 to 100 compressions per minute. Before the induction of ventricular fibrillation, all animals were intubated and ventilated with room air, 10 mL/kg. The endotracheal tube was removed when VF was induced. Pre-VF arterial pH, PCO2, and O2 saturation were (mean +/- SEM) 7.39 +/- 0.02, 27.0 +/- 1.5 mm Hg, and 97.5 +/- 0.5%, respectively, with aortic pressures being 143.2 +/- 5.7/116.2 +/- 4.6 mm Hg. At 4 minutes of chest compression alone, the corresponding values were 7.39 +/- 0.03, 24.3 +/- 3.1 mm Hg, and 93.9 +/- 3.0%, with an arterial pressure of 48.1 +/- 7.7/22.6 +/- 3.9 mm Hg. Mean minute ventilation during the fourth minute of CPR, measured with a face mask-pneumotachometer, was 5.2 +/- 1.1 L/min. CONCLUSIONS: These data suggest that in the dog model of witnessed arrest, chest compression alone during CPR can maintain adequate gas exchange to sustain O2 saturation > 90% for > 4 minutes. The need for immediate ventilation during witnessed arrest should be reexamined. LOE:6 Idris, 1995 Idris A, Wenzel V, Banner MJ, Melker RJ. Smaller tidal volumes minimize gastric inflation during CPR with an unprotected airway [abstract]. Circulation 1995;92(suppl):I-759. No abstract LOE:6 Idris, 1995 Idris AH, Wenzel V, Becker LB, Banner MJ, Orban DJ. Does hypoxia or hypercarbia independently affect resuscitation from cardiac arrest? Chest. 1995;108(2):522-8. STUDY OBJECTIVE: In a previous cardiopulmonary resuscitation (CPR) study in swine, ventilation was associated with improved rate of return of spontaneous circulation (ROSC) compared with nonventilated animals, which had greater hypoxia and hypercarbic acidosis. We used the same model to determine the independent effect of hypoxia and hypercarbic acidosis on ROSC after cardiac arrest. DESIGN: Laboratory model of cardiac arrest. SETTING: University teaching hospital laboratory. PARTICIPANTS: Domestic swine (23 to 61 kg). INTERVENTIONS: Twenty-four swine were randomly assigned to three groups receiving ventilation during CPR with 85% O2/15% N2 (control), 95% O2/5% CO2 (hypercarbia), or 10% O2/90% N2 (hypoxia). All animals had ventricular fibrillation for 6 min without CPR, then CPR with one of the ventilation gases for 10 min, then defibrillation. Animals without ROSC received epinephrine, 85% O2, CPR for another 3 min, and defibrillation. MEASUREMENTS AND RESULTS: During the tenth 09a826193e718c0be8c6b2f6224b6745.doc Page 20 of 23
minute of CPR, the hypercarbic group had more mean (SD) arterial hypercarbia than the control group (PCO2, 47 +/- 6, compared with 34 +/- 6; p < 0.01), and greater mixed venous hypercarbia (PCO2, 72 +/- 14, compared with 59 +/- 8; p < 0.05), while mean arterial and mixed venous PO2 was not significantly different. The hypoxic group had significantly less mean arterial (43 +/- 9 compared with 228 +/- 103 mm Hg) and mixed venous (22 +/- 5 compared with 35 +/- 7 mm Hg) PO2 when compared with the control group (p < 0.01), while mean arterial and mixed venous PCO2 were not significantly different. Thus, the model succeeded in producing isolated hypercarbia without hypoxia in the hypercarbic group and isolated hypoxia without hypercarbia in the hypoxic group. The rate of ROSC was 6/8 (75%) for the control group, 1/8 (13%) for the hypercarbic group, and 1/8 (13%) for the hypoxic group (p < 0.02). CONCLUSIONS: Both hypoxia and hypercarbia independently had an adverse effect on resuscitation from cardiac arrest. In this model with a prolonged interval of untreated cardiac arrest, adequate ventilation was important for resuscitation. LOE:6 Berg, 1995 Berg RA, Wilcoxson D, Hilwig RW, Kern KB, Sanders AB, Otto CW, et al. The need for ventilatory support during bystander CPR. Ann Emerg Med 1995;26(3):342-350. STUDY OBJECTIVE: To compare CPR with chest compressions plus ventilatory support (CC+V) and chest compressions alone (CC). DESIGN: Prospective, randomized study. SETTING: Research laboratory. INTERVENTIONS: After 2 minutes of ventricular fibrillation, 18 domestic swine (20 to 35 kg) were treated first with CC or CC+V for 10 minutes, then with standard advanced cardiac life support. RESULTS: Hemodynamics, survival, and neurologic outcome were determined. All 8 swine subjected to CC+V and all 10 subjected to CC showed return of spontaneous circulation. One animal in each group died within 1 hour. Seven of 8 animals in the CC+V group survived for 24 and 48 hours, compared with 9 of 10 CC animals at 24 hours and 8 of 10 at 48 hours. All 48-hour survivors were neurologically normal. CONCLUSION: In this experimental model of bystander CPR, we could not detect a difference in hemodynamics, 48-hour survival, or neurologic outcome when CPR was applied with and without ventilatory support. LOE:6 Noc, 1995 Noc M, Weil MH, Tang W, Turner T, Fukui M. Mechanical ventilation may not be essential for initial cardiopulmonary resuscitation. Chest 1995;108(3):821-827. BACKGROUND: In a rodent model of cardiac arrest and resuscitation in which the inspired gas mixture was enriched with oxygen, resuscitability and survival were unaffected by positive pressure ventilation. In the present study, in a larger animal model, tidal volumes generated during precordial compression and with spontaneous gasping were quantitated. METHODS: Domestic pigs with an average weight of 34 kg were anesthetized with pentobarbital. Ventricular fibrillation (VF) was induced electrically. Precordial compression was begun after 4 min of untreated VF. Each of 22 animals received one of two interventions in conjunction with precordial compression: positive pressure ventilation with oxygen or oxygen supplied at the port of a tracheal tube at ambient pressure. After 8 min of precordial compression, defibrillation was attempted. RESULTS: Only very moderate increases in arterial PCO2 were documented during cardiopulmonary resuscitation in the absence of mechanical ventilation but arterial oxygen tension was consistently in excess of 100 mm Hg. Cardiac resuscitability and 48-h survival were approximately the same in animals maintained on inspired oxygen whether or not they were mechanically ventilated (7/11 or 8/11). In the absence of mechanical ventilation, precordial compression and spontaneous gasping yielded minute volumes that exceeded 5 L. CONCLUSION: Positive pressure mechanical ventilation did not improve resuscitability or postresuscitation outcome in this porcine model of cardiac arrest. LOE:6 Engoren, 1997 Engoren M, Plewa MC, Buderer NF, Hymel G, Brookfield L. Effects of simulated mouth-to-mouth ventilation during external cardiac compression or active compression-decompression in a swine model of witnessed cardiac arrest. Ann Emerg Med 1997;29(5):607-615. LOE:6 Berg, 1997 Berg RA, Kern KB, Hilwig RW, Berg MD, Sanders AB, Otto CW, et al. Assisted ventilation does not improve outcome in a porcine model of single-rescuer bystander cardiopulmonary resuscitation. 09a826193e718c0be8c6b2f6224b6745.doc Page 21 of 23
Circulation 1997;95(6):1635-1641. BACKGROUND: Mouth-to-mouth rescue breathing is a barrier to the performance of bystander cardiopulmonary resuscitation (CPR). We evaluated the need for assisted ventilation during simulated single-rescuer bystander CPR in a swine model of prehospital cardiac arrest. METHODS AND RESULTS: Five minutes after ventricular fibrillation, swine were randomly assigned to 8 minutes of hand-bag-valve ventilation with 17% oxygen and 4% carbon dioxide plus chest compressions (CC + V), chest compressions only (CC), or no CPR (control group). Standard advanced life support was then provided. Animals successfully resuscitated received 1 hour of intensive care support and were observed for 24 hours. All 10 CC animals, 9 of the 10 CC + V animals, and 4 of the 6 control animals attained return of spontaneous circulation. Five of the 10 CC animals, 6 of the 10 CC + V animals, and none of the 6 control animals survived for 24 hours (CC versus controls, P = .058; CC + V versus controls, P < .03). All 24-hour survivors were normal or nearly normal neurologically. CONCLUSIONS: In this model of prehospital single- rescuer bystander CPR, successful initial resuscitation, 24-hour survival, and neurological outcome were similar after chest compressions only or chest compressions plus assisted ventilation. Both techniques tended to improve outcome compared with no bystander CPR. LOE:6 Berg, 1997 Berg RA, Kern KB, Hilwig RW, Ewy GA. Assisted ventilation during 'bystander' CPR in a swine acute myocardial infarction model does not improve outcome. Circulation 1997;96(12):4364-4371. BACKGROUND: Mouth-to-mouth rescue breathing is a barrier to the performance of bystander cardiopulmonary resuscitation (CPR). We evaluated the need for assisted ventilation during simulated single-rescuer bystander CPR in a swine myocardial infarction model of prehospital cardiac arrest. METHODS AND RESULTS: Steel cylinders were placed in the mid left anterior descending coronary arteries of 43 swine. Two minutes after ventricular fibrillation, animals were randomly assigned to 10 minutes of hand-bag-valve ventilation with 17% oxygen and 4% carbon dioxide plus chest compressions (CC+V), chest compressions only (CC), or no CPR (control group). Standard advanced life support was then provided. Animals successfully resuscitated received 1 hour of intensive care support and were observed for 24 hours. Five of 14 CC animals, 3 of 15 CC+V animals, and 1 of 14 controls survived for 24 hours (CC versus controls, P=.07). Myocardial oxygen delivery and consumption were greater among surviving animals than nonsurvivors but did not differ between CC and CC+V animals. CONCLUSIONS: In this acute myocardial infarction model of prehospital single-rescuer bystander CPR, assisted ventilation did not improve outcome. LOE:6 Kern, 1998 Kern KB, Hilwig RW, Berg RA, Ewy GA. Efficacy of chest compression-only BLS CPR in the presence of an occluded airway. Resuscitation 1998;39(3):179-188. Reluctance of the lay public to perform bystander CPR is becoming an increasingly worrisome problem in the USA. Most bystanders who admit such reluctance concede that fear of contagious disease from mouth-to-mouth contact is what keeps them from performing basic life support. Animal models of prehospital cardiac arrest indicates that 24-h survival is essentially as good with chest compression-only CPR as with chest compressions and assisted ventilation. This simpler technique is an attractive alternative strategy for encouraging more bystander participation. Such experimental studies have been criticized as irrelevant however secondary to differences between human and porcine airway mechanics. This study examined the effect of chest compression-only CPR under the worst possible circumstances where the airway was totally occluded. After 6 min of either standard CPR including ventilation with a patent airway or chest compressions-only with a totally occluded airway, no difference in 24 h survival was found (10/10 vs. 9/10). As anticipated arterial blood gases were not as good, but hemodynamics produced were better with chest compression-only CPR (P < 0.05). Chest compression-only CPR, even with a totally occluded airway, is as good as standard CPR for successful outcome following 6.5 min of cardiac arrest. Such a strategy for the first minutes of cardiac arrest, particularly before professional help arrives, has several advantages including increased acceptability to the lay public. LOE:6 Berg, 2001 Berg RA, Sanders AB, Kern KB, Hilwig RW, Heidenreich JW, Porter ME, et al. Adverse hemodynamic effects of interrupting chest compressions for rescue breathing during 09a826193e718c0be8c6b2f6224b6745.doc Page 22 of 23
cardiopulmonary resuscitation for ventricular fibrillation cardiac arrest. Circulation 2001;104(20):2465-2470. BACKGROUND: Despite improving arterial oxygen saturation and pH, bystander cardiopulmonary resuscitation (CPR) with chest compressions plus rescue breathing (CC+RB) has not improved survival from ventricular fibrillation (VF) compared with chest compressions alone (CC) in numerous animal models and 2 clinical investigations. METHODS AND RESULTS: After 3 minutes of untreated VF, 14 swine (32+/-1 kg) were randomly assigned to receive CC+RB or CC for 12 minutes, followed by advanced cardiac life support. All 14 animals survived 24 hours, 13 with good neurological outcome. For the CC+RB group, the aortic relaxation pressures routinely decreased during the 2 rescue breaths. Therefore, the mean coronary perfusion pressure of the first 2 compressions in each compression cycle was lower than those of the final 2 compressions (14+/-1 versus 21+/-2 mm Hg, P<0.001). During each minute of CPR, the number of chest compressions was also lower in the CC+RB group (62+/-1 versus 92+/-1 compressions, P<0.001). Consequently, the integrated coronary perfusion pressure was lower with CC+RB during each minute of CPR (P<0.05 for the first 8 minutes). Moreover, at 2 to 5 minutes of CPR, the median left ventricular blood flow by fluorescent microsphere technique was 60 mL. 100 g(-1). min(-1) with CC+RB versus 96 mL. 100 g(-1). min(-1) with CC, P<0.05. Because the arterial oxygen saturation was higher with CC+RB, the left ventricular myocardial oxygen delivery did not differ. CONCLUSIONS: Interrupting chest compressions for rescue breathing can adversely affect hemodynamics during CPR for VF. LOE:6 Kern, 2002 Kern KB, Hilwig RW, Berg RA, Sanders AB, Ewy GA. Importance of continuous chest compressions during cardiopulmonary resuscitation: improved outcome during a simulated single lay-rescuer scenario. Circulation 2002;105(5):645-9. BACKGROUND: Interruptions to chest compression-generated blood flow during cardiopulmonary resuscitation (CPR) are detrimental. Data show that such interruptions for mouth- to-mouth ventilation require a period of "rebuilding" of coronary perfusion pressure to obtain the level achieved before the interruption. Whether such hemodynamic compromise from pausing to ventilate is enough to affect outcome is unknown. METHODS AND RESULTS: Thirty swine (weight 35 +/- 2 kg) underwent 3 minutes of untreated ventricular fibrillation before 12 minutes of basic life support CPR. Animals were randomized to receive either standard airway (A), breathing (B), and compression (C) CPR with expired-gas ventilation in a 15:2 compression-to-ventilation ratio or continuous chest compression CPR. Those randomized to the standard 15:2 group had no chest compressions for a period of 16 seconds each time the 2 ventilations were delivered. Defibrillation was attempted at 15 minutes of cardiac arrest. All resuscitated animals were supported in an intensive care environment for 1 hour, then in a maintenance facility for 24 hours. The primary end point of neurologically normal 24-hour survival was significantly better in the experimental group receiving continuous chest compression CPR (12 of 15 versus 2 of 15; P<0.0001). CONCLUSIONS: Mouth-to-mouth ventilation performed by single layperson rescuers produces substantial interruptions in chest compression-supported circulation. Continuous chest compression CPR produces greater neurologically normal 24-hour survival than standard ABC CPR when performed in a clinically realistic fashion. Any technique that minimizes lengthy interruptions of chest compressions during the first 10 to 15 minutes of basic life support should be given serious consideration in future efforts to improve outcome results from cardiac arrest. LOE:6 Sanders, 2002 Sanders AB, Kern KB, Berg RA, Hilwig RW, Heidenrich J, Ewy GA. Survival and neurologic outcome after cardiopulmonary resuscitation with four different chest compression-ventilation ratios. Ann Emerg Med 2002;40(6):553-62. STUDY OBJECTIVE: The optimal ratio of chest compressions to ventilations during cardiopulmonary resuscitation (CPR) is unknown. We determine 24-hour survival and neurologic outcome, comparing 4 different chest compression-ventilation CPR ratios in a porcine model of prolonged cardiac arrest and bystander CPR. METHODS: Forty swine were instrumented and subjected to 3 minutes of ventricular fibrillation followed by 12 minutes of CPR by using 1 of 4 models of chest compression-ventilation ratios as follows: (1) standard CPR with a ratio of 15:2; (2) CC-CPR, chest compressions only with no ventilations for 12 minutes; (3) 50:5-CPR, CPR with a ratio of 50:5 compressions to ventilations, as advocated by authorities in Great Britain; and (4) 09a826193e718c0be8c6b2f6224b6745.doc Page 23 of 23
100:2-CPR, 4 minutes of chest compressions only followed by CPR with a ratio of 100:2 compressions to ventilations. CPR was followed by standard advanced cardiac life support, 1 hour of critical care, and 24 hours of observation, followed by a neurologic evaluation. RESULTS: There were no statistically significant differences in 24-hour survival among the 4 groups (standard CPR, 7/10; CC-CPR, 7/10; 50:5-CPR, 8/10; 100:2-CPR, 9/10). There were significant differences in 24-hour neurologic function, as evaluated by using the swine cerebral performance category scale. The animals receiving 100:2-CPR had significantly better neurologic function at 24 hours than the standard CPR group with a 15:2 ratio (1.5 versus 2.5; P =.007). The 100:2-CPR group also had better neurologic function than the CC-CPR group, which received chest compressions with no ventilations (1.5 versus 2.3; P =.027). Coronary perfusion pressures, aortic pressures, and myocardial and kidney blood flows were not significantly different among the groups. Coronary perfusion pressure as an integrated area under the curve was significantly better in the CC-CPR group than in the standard CPR group (P =.04). Minute ventilation and PaO (2) were significantly lower in the CC-CPR group. CONCLUSION: In this experimental model of bystander CPR, the group receiving compressions only for 4 minutes followed by a compression-ventilation ratio of 100:2 achieved better neurologic outcome than the group receiving standard CPR and CC-CPR. Consideration of alternative chest compression-ventilation ratios might be appropriate. LOE:6