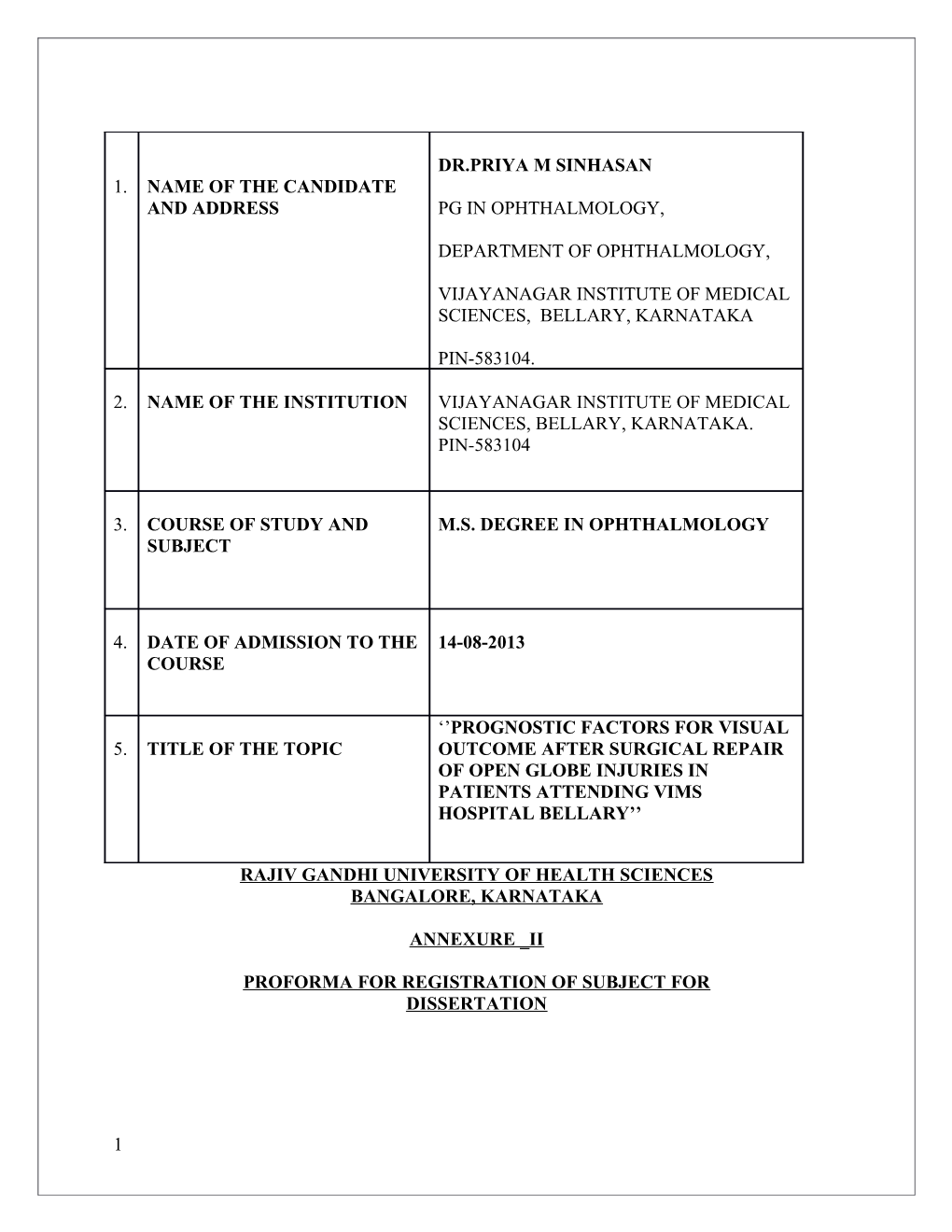
DR.PRIYA M SINHASAN 1. NAME OF THE CANDIDATE AND ADDRESS PG IN OPHTHALMOLOGY,
DEPARTMENT OF OPHTHALMOLOGY,
VIJAYANAGAR INSTITUTE OF MEDICAL SCIENCES, BELLARY, KARNATAKA
PIN-583104.
2. NAME OF THE INSTITUTION VIJAYANAGAR INSTITUTE OF MEDICAL SCIENCES, BELLARY, KARNATAKA. PIN-583104
3. COURSE OF STUDY AND M.S. DEGREE IN OPHTHALMOLOGY SUBJECT
4. DATE OF ADMISSION TO THE 14-08-2013 COURSE
‘’PROGNOSTIC FACTORS FOR VISUAL 5. TITLE OF THE TOPIC OUTCOME AFTER SURGICAL REPAIR OF OPEN GLOBE INJURIES IN PATIENTS ATTENDING VIMS HOSPITAL BELLARY’’
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES BANGALORE, KARNATAKA
ANNEXURE _II
PROFORMA FOR REGISTRATION OF SUBJECT FOR DISSERTATION
1 6. BRIEF RESUME OF INTENDED WORK
6.1.NEED FOR THE STUDY:
Ocular trauma is one of the leading causes of ocular morbidity in all the age groups especially children and young adults. Successful surgical repair of open globe injury and subsequent visual rehabilitation is a topic of great significance and challenge to the practicing ophthalmologists. Even though, with the advent of new modalities and improved technology, the management of penetrating ocular injuries has changed, we need to prognosticate any patient with ocular trauma before and after the repair of open globe injuries. Monocular blindness accounts for more than 40% due to ocular injuries2, 3, 4.
Surgical repair and subsequent visual rehabilitation have its own significance in the outcome of varieties of ocular trauma5.Management of open globe injuries poses great dilemma in children as the surgical repair in a Childs eye is much more difficult and challenging than the management of an adult trauma. Over and above repeated examinations under general anesthesia prolonged periods of visual deprivations which can be amblyogenic and visual rehabilitations are some of the many factors making a child hood open globe injury a difficult entity to deal with. International classification of ocular trauma is based on some of the variables affecting the final visual outcome. The factors governing the prognosis of visual outcome plays a major role in Open Globe Injuries are;
Age Sex Preoperative visual acuity Mode of injury Type of injury Time lag between injury and surgery Location and extent of wound
2 Visual axis involvement Relative afferent pupillary defect Lens status Involvement of ocular structures causing hyphema,uveal or retinal tissue prolapse, vitreous loss, vitreous hemorrhage, retinal detachment Presence and type of foreign body
So an attempt is intended to study the prognostic factors for visual outcome in open globe injuries after surgical repairs.
6.2. REVIEW OF LITERATURE: Due to the rapid growth in all the sectors in the world, the incidence of ocular injuries has been consistently on higher side. Major causes being the profession or work related, assault, sports and road traffic accidents7, 8,9,10.
Though, the open globe injuries are less common compared to blunt/ closed globe injuries, it significantly cripples the life of subject by causing visual impairment11.
An open globe injury by definition is a full thickness wound of corneoscleral envelope.
Classification of Open Globe Injuries has been made depending on the type, visual acuity; zones affected and defect in pupillary response12.
Types: 1. Rupture. (Blunt trauma) 2. Penetrating. 3. Intraocular foreign body. 4. Perforating. 5. Mixed. Grade (visual acuity) > 20/40 20/50 to 20/100 19/100 to 5/200 4/200 to light perception
3 No light perception Pupil Positive RAPD in injured eye Negative RAPD in injured eye Zone I. cornea and limbus
II. limbus to5mm posterior into sclera
III. posterior to 5mm from limbus
KhodamRostomian et al studied 50 children with open globe injuries and found a male preponderance (71%). The average age of patients in their study was 5 yrs. Sharp objects caused majority of injuries (92%).The cornea was involved in 92 % of cases and 32 eyes required only primary repair. 5 eyes were enucleated. Visual acuity of 20/40 or better was obtained in 45% of cases. The factors related to unfavourable visual outcome were retinal detachment, RAPD, vitreous hemorrhage and hyphema. Endophthalmitis following penetrating eye injuries has a relatively poor prognosis due to the underlying eye trauma and the frequency of more virulent organisms such as Bacillus species. Risk factors for infection include 1) retained intraocular foreign body, 2) a rural injury setting, 3) delay in primary wound closure, and 4) disruption of the crystalline lens.15
Kyle J alliman et al studied Ocular trauma and visual outcome secondary to paintball projectiles and they found that 86% were males and most common ocular finding was hyphema. 81 % eyes needed surgical intervention and 22% needed enucleation. They found that 97 % were not wearing eye protection at the time of trauma13.
4 In a study done at EyeResearch Center, Farabi Eye Hospital, Tehran University of Medical
Sciences (TUMS), Tehran, Iran, showed tat of the 98 patients included in the study, men exhibited a greater vulnerability and they were mostly aged around 29 years old. In terms of the place of trauma, 40 (43.5%) cases occurred in the street, 27 cases (29.3%) occurred at home, and
17 cases (18.5%) occurred at the workplace, while 4 cases (4.3%) happened in entertaining environments like parks. For 3 patients (3.3%), the incident took place at a public pathway, and in 1 patient (1.1%), the case occurred at school. As the most common cause of trauma, 41 patients (42.3%) had an object hit their eyes. In addition, assaults were a major cause of injury.
The right eye and the upper lid were also the most common sites of injuries. Although no blindness occurred due to trauma causing eyelid laceration, the visual outcomes were correlated with severity of the incident defined based on the presence of open globe injuries.
In a study done at L V Prasad Eye Institute, Hyderabad involving 325 patients of ocular trauma, anterior segment was involved in 51.1 %, posterior segment in 8.9% and both in 31.4% of the patients. The factors associated with visual impairment (VA < 6/18) were poor initial visual acuity, full chamber hyphaema, Retinal detachment and Vitreous hemorrhage14.
R V Azad et al did a study to know the profile of ocular trauma at tertiary eye centre. Out of total
523 eyes registered large proportion was <25years of age (67%), males(88%) and literate (77%).
Forty-four percent belonged to rural area and 38% were students. Most of the open globe injuries were Zone 1(50.8%). 75% presented >1 week after injury. The incidence of intraocular foreign body and retinal detachment was 17.4, and 11.3% respectively. Diagnosis of post traumatic endophthalmitis was made in 20.5% of open globe injuries. Development of
5 endophthalmitis correlated with younger age, rural setting, illiteracy, presence of foreign body and lens disruption.9
A two year prospective study done at Wilmer Ophthalmological institute found that domestic accidents and assault each accounted for approximately one third of the injuries in their study.10
According to “The Aravind Comprehensive Eye Survey” on “Ocular trauma in a rural South
Indian Population”, prevelance of blindness in any eye caused by trauma was 0.8%, Odds ratio for trauma was higher for males and labourers and lower literates. In this study, it was concluded that ocular trauma is to be considered as a priority in South Indian population, because lifetime prevalence of ocular trauma is higher than that reported for glaucoma, age related macular degeneration or ]diabetic retinopathy for this population. Simple measures such as education regarding the use of protective eye wear could possibly significantly decrease this preventable cause of visual disability.15
In a study done by Imtiaz A, Choudhry et al, who studied visual outcome of endophthalmitis associated with IOFB, it was found that delayed removal of IOFB following trauma significantly increased the chances of endophthalmitis.17
Reynolds DS et al did a study on post traumatic endophthalmitis and found that endophthalmitis following penetrating eye injuries has a relatively poor prognosis due to the underlying eye trauma and the frequency of more virulent organisms such as Bacillus species.
Risk factors for infection include 1) retained intraocular foreign body, 2) a rural injury setting, 3) delay in primary wound closure, and 4) disruption of the crystalline lens.18
6 It was found that the risk of developing glaucoma following penetrating ocular trauma was
2.67%, in a cohort study done by Cristopher AGirkin et al, wherein 3,627 patients who met with penetrating ocular injury were studied.18
Sharma T, Agarwal P, Gopal L, Badrinath S S, MurugesanR at Vision Research Foundation,
Madras, studied 100 children with penetrating injury with broomstick bows and arrows. They found that successful reconstruction of the globe with attached retina was attained in 85% of the eyes. Improvement in visual acuity of two Snellen lines in eyes with measurable pre operative acuity or improvement to at least 2 / 60 with pre operative acuity of PL or HM, was attained in
62% of the eyes; acuity of 6/9 or better was achieved in 28%. Predictors of poor anatomical success were injuries involving both anterior and posterior segment, endophthalmitis and presence of retinal detachment.21
A study was done by Lamkin JC et al to know the outcomes of simultaneous corneal laceration repair, cataract removal and PCIOL implantation found that corneal lacerations with traumatic cataract without any other associated complications like vitreous loss are amenable to cataract extraction and lens implantation at the time of primary repair. They found that this approach obviated the need for additional operative procedure and anesthetic risks while affording more timely visual rehabilitation. 23
Steqmann R and Miller D did a study on use of sodium hyaluronate in penetrating injuries and the study describes the surgical treatment and eventual outcome of 15 cases of anterior-segment penetrating ocular trauma that would be classically considered as having a poor prognosis. Signs of poor prognosis included: corneal lacerations, complicated by signs of infection ranging from infiltration to necrotic digestion; large scleral lacerations, with ciliary body or choroidalprolapse;
7 and an exaggerated inflammatory response to the trauma. Treatment included careful microsurgical techniques, vitrectomy (when necessary), use of antibiotics and anti-inflammatory agents, and the liberal use of sodium hyaluronate to break fibrin adhesions and maintain the chamber at the close of surgery. Such treatment resulted in no enucleations, an average best corrected visual acuity of 20/80, an average normal angle of 314 degrees, and 13 cases of normal intraocular pressure without medication.24
A study done by David Leonardo Cruvinel Isaac et al analysed the prognostic factors in open globe injuries and showed that length of laceration, elapsed time between trauma and surgery, presence or absence of vitreous loss, cataract, hyphema and retinal detachment were important factors related to poor post operative visual acuity.27
Visual outcome of pars planavitrectomy with intraocular foreign body removal through sclerocorneal tunnel and sulcus-fixated intraocular lens implantation as a single procedure, in cases of metallic intraocular foreign body with traumatic cataract was studied be
SanthoshMahapatra et al. All the 18 patients were young males, with an average follow-up period of 12 months. In 12 cases the foreign body was intravitreal and in six cases it was intraretinal but extramacular. Thirteen cases had a best corrected visual acuity ranging from
20/20 to 20/60 at their last follow-up. Five cases developed retinal detachment due to proliferative vitreoretinopathy (PVR) changes postoperatively and were subsequently managed by surgery.28
6.3.OBJECTIVE OF STUDY
8 To know the prognostic factors for visual outcome in open globe injuries following surgical repair.
7.MATERIALS AND METHODS
7.1.SOURCES OF DATA: The study will be conducted prospectively in patients, attending
VIMS Hospital Bellary. The study will be conducted in the Department of Ophthalmology at
VIMS Bellary
7.2.METHODS OF COLLECTION OF DATA
A) STUDY DESIGN: Prospective study
B) STUDY PERIOD: Nov 2013 to Jun 2015.
C) PLACE OF STUDY: Department of Ophthalmology, VIMS, Bellary.
D) SAMPLE SIZE: cases of open globe injuries with surgical repair.
E) INCLUSION CRITERIA:
All patients with open globe injuries attending VIMS HOSPITAL BELLARY.
F) EXCLUSION CRITERIA
9 1. Chemical ocular injuries.
2. Systemically unstable patients.
3. Previous ocular morbidity
4. Associated head injury which affects visual acuity
5. Who underwent previous ocular surgeries
STUDY METHODOLOGY : During the above said period patients satisfying the inclusion criteria are selected · The patients presenting with open globe injuries at VIMS, Bellary
Assessment consists of: · Determining the modes and types of injury
· Ocular tissues involved
· Visual acuity testing
· Slit lamp examination
· Direct and indirect Ophthalmoscopy
· Gonioscopy and B-scan in relevant cases
· Radiograph of orbit in relevant cases
· CT scan of orbit in relevant cases
· MRI in relevant cases
STATISTICAL ANALYSIS
10 Descriptive statistics will be done for all data. Based on normality, parametric and non- parametric tests will be done and will be declared statistically significant for p-value <0.05.
7.4. HAS ETHICAL CLEARANCE BEEN OBTAINED FROM YOUR INSTITUTION IN CASE OF 7.3.
YES, Ethical clearance has been obtained from the Institutional Ethics Committee, Vijayanagar Institute of Medical Sciences.
8. LIST OF REFERENCES:
1. Rao LG, and Ninan A, Rao KA. Descriptive study on ocular survival, visual outcome prognostic factors in open globe injuries. Indian J Ophthalmol. 2010;58:321–3.
2. Gupta A, Srinivasan R, Babu KR, Setia S. Comparison of the clinical presentation and visual outcome in open globe injuries in adults and children over 30 months. Eur J Ophthalmol. 2010;20:590–5.
3. Biju John MS, FRCS. ChithraRaghavan DNB ; Open Globe Injuries-Primary Repair of Corneoscleral Injuries; ksojournal; Vol. XXII, No.3, Sept. 2010 (225-234
4. Kyle J Alliman, William E Smiddy, James Banta: Ocular trauma and visual outcome secondary to paintball projectiles: Am J of Oph: Vol 147, Issue @, Feb 2009,239-242.e1
5. Charles C Wykoff, Harry W Flynn Jr, Darlene Miller, Ingrid U Scott, Eduardo C Alfonso: “Exogenous Fungal Endophthalmitis: Microbiology and clinical outcome” Ophthalmology vol 115, no 9, Sept 2008
6. Imtiaz A. Choudhry; Farrukh A Shamsi; Abdulwahab Al-Theeb; Incidence and Visual outcome of Endophthalmitis Associated with intraocular foreign bodies; Graefe’s Arch for Clinical and Exp Ophthalmology; Vol 246, No 2, Feb 2008
7. Kuhn F, Morris R, Witherspoon CD, Mann L: Epidemiology of blinding trauma in the United States Eye Injury Registry. Ophthalmic Epidemiol 13: 209-16, 2006
8. Kampougeris G, Antoniadou A, Kavouklis E, et al: Penetration of moxifloxacin into the human aqueous humour after oral administration. Br J Ophthalmol 89: 628- 31, 2005
11 9. Cristopher A Girkin, Gerald McGwinJr, Robert Morris, Ferenc Kuhn “Glaucoma following penetrating ocular trauma: A cohort study of the United States Eye Injury Registry” American Journal of Ophthalmology, 23 Aug 2004.
10. Pieramici, Dante J. The prognostic significance of a system for classifying Mechanical injuries of the eye in Open globe injuries; Journal of trauma: Injury, Infection and Critical care. April 2003;54 (4);750-4. 11. Boscia F, La Tegola MG, Columbo G, et al: Combined topical anesthesia and sedation for open-globe injuries in selected patients. Ophthalmology 110: 1555-9, 2003
12. Scott IU, Mccabe CM, Flynn HW, injuries. Am J Ophthalmol 134: 707-11, 2002et al: Local anesthesia with intravenous sedation for surgical repair of selected open globe.
13. Thylefors B: Epidemiologic patterns of ocular trauma. Aust N Z J Ophthalmol 20:95,1992.
14. Negrel AD, Massembo-Yako B, Botaka E et al: Prevalence et causes de la ceciteouCongo. Bull WHO 68:237, 1990
15. Dana MR, Tielsch JM, Enger C et al: Visual impairment in a rural Appalachian community. JAMA 264:2400, 1990.
16. Sterberg P., Jr . Prognosis and outcomes for penetrating ocular trauma. In: Shingleton BJ, Hersh PS, Kenyon KR, editors. Eye trauma. Louis: Mosby Year Book; 1991. pp. 238–41.
17. Kuhn F, Morris R, Witherspoon CD, Heimann K, Jeffers JB, Treister G. A standardized classification of ocular trauma. Ophthalmology. 1996;103:240–3.
18. Liggett PE, Pince KJ, Barlow W et al: Ocular trauma in an urban population. Ophthalmology 97:581, 1990
19. Schein OD, Hibberd PL, Shingleton BJ et al: The spectrum and burden of ocular injury. Ophthalmology 95:300, 1988
20. MacEwen CJ: Eye injuries: A prospective survey of 5671 cases. Br J Ophthalmol 73:888, 1989.
21. Dannenberg AL, Parver LM, Brechner RJ et al: Penetrating eye injuries in the workplace. Arch Ophthalmol 110:843, 1992
22. V K GothwalBopt, S Adolph Dopt, S JalaliMs& TJ NaduvilathMsc, L V Prasad Eye Institute, Hyderabad: “Demography and prognostic factors of ocular injuries in
12 South India”; Australian and New Zealand Journal of Ophthalmology, Vol 27 Issue 5, Pages 318-325.
23. Ocular trauma in a rural South Indian Population- The Aravind Comprehensive Eye Survey: Ophthalmology Vol 111, issue 9, pages 1778-1781
13 9. SIGNATURE OF THE CANDIDATE
10. REMARKS OF THE GUIDE
11. NAME & DESIGNATION (IN BLOCK LETTERS)
11.1 GUIDE DR. PAVAN G PROF AND HOD DEPT OF OPHTHALMOLOGY VIMS ,BELLARY 11.2 SIGNATURE
11.3 CO-GUIDE (IF ANY) DR.VIJAY N ASSOCIATE PROFESSOR DEPT OF OPHTHALMOLOGY VIMS ,BELLARY 11.4 SIGNATURE
11.5 HEAD OF THE DR.PAVAN G DEPARTMENT PROF AND HOD DEPARTMENT OF OPHTHALMOLOGY VIJAYANAGAR INSTITUTE OF MEDICAL SCIENCES, BELLARY, KARNATAKA
11.6 SIGNATURE
12. 12.1 REMARKS OF THE CHAIRMAN & PRINCIPAL
12.2 SIGNATURE
28-10-2013 Bellary
14