Document Title and Code: Pain Management Policy / NMA-PM. Version: 3 Author: Prepared by Nursing Matters and Associates. Adapted for Local use by: Issue Date: March 2016 Review date: March 2019 Authorised by:
1.0 Policy Statement: Management of pain is an important element of promoting both the dignity and quality of life of residents. It is therefore the policy of the Centre that residents with pain will have a person centred assessment and care plan to meet their needs for pain management. Pain management will be evidence based and aimed at either alleviating the pain or where this is not possible, reducing it to a level acceptable to the individual resident. Approaches to pain management will be aimed at minimising the effect of pain on functional ability and quality of life.
2.0 Purpose: The purpose of this policy is to ensure that every resident presenting with pain will have an assessment and care plan individual to his/her needs, preferences and wishes.
3.0 Objectives:
1.1 To ensure that approaches to pain management are aimed at the resident being either pain free or having their pain controlled to a level that is acceptable to them.
1.2 To ensure that residents with pain will be enabled to maintain the highest level of functioning possible to them.
1.3 To minimise the impact of pain on the resident’s well being and quality of life.
4.0 Scope: This policy applies to all nursing staff, healthcare assistants and other health care professionals involved in management of pain for individual residents.
5.0 Definitions: This policy adopts the combination of the following definition of pain:
“ An unpleasant sensory and emotional experience associated with actual or potential tissue damage, or described in terms of such damage” (International Association for the Study of Pain, 1986) While also acknowledging that pain is: “Whatever the experiencing person says it is, existing whenever he says it does” (McCaffery and Pasero 1999).
1 | P a g e M a n a g e m e n t o f P a i n P o l i c y 0 7 0 3 2 0 1 6 Pain is classified according to: A. Duration, that is acute pain usually resulting from injury, surgery or tissue damage; and persistent pain referring to pain that extends beyond the normal duration of tissue damage (3-6 months). B. Pathophysiology or cause. ◙ Nociceptive pain is due to stimulation of peripheral or visceral pain receptors resulting from disease processes such as osteoarthritis; soft tissue injuries such as falls or medical procedures. It is usually localised and responds well to treatment. ◙ Neuropathic pain results from damage to the peripheral and / or central nervous system. It is often described in terms such as burning, itching, tingling, electric or shooting. It is usually more diffuse and less responsive to conventional analgesics. ◙ Pain due to psychological / psychiatric factors said to be present when psychological / psychiatric factors are judged to play a major role in the onset, severity and maintenance of the pain. However, medical conditions may also be present and contribute to the presentation, particularly in older people. ◙ Pain related to mixed or unknown mechanisms. Management may require trials of different and / or combination of approaches. (Australian Pain Society, 2005; Hartford Institute of Geriatric Nursing, 2013).
Key Messages: Pain and Older People. Pain is commonly experienced by many older adults. It is estimated that approximately 85% of nursing home residents experience persistent pain. Pain is a subjective experience that is influenced by cognitive, emotional, medical and cultural factors. Failure to identify pain often stems from residents’ cognitive and communication impairments; attitudes; inadequate staff awareness and high workloads. The possibility of the onset of pain should be considered if there is a significant change in a resident’s condition and routinely every three months. Evidence suggests that pain for residents in residential care is poorly identified, assessed and management.
2 | P a g e M a n a g e m e n t o f P a i n P o l i c y 0 7 0 3 2 0 1 6 6.0 Responsibilities. Actions Responsible Person. This policy will be disseminated to and read by all nursing Person in Charge/Director personnel involved in assessment and care planning for residents. of Nursing. A record will be kept of all those who have signed the policy Person in Charge/Director acknowledgement forms. of Nursing. Where a new version of this policy is produced, the previous Person in Charge/Director version will be removed and filed away. of Nursing. An explanation of this policy will be given to all new nursing staff, Person in Charge/Director care assistants and other healthcare professionals involved in the of Nursing or delegated to management of pain for individual residents. another named nurse. Nurses will be provided with the opportunity to attend training Person in Charge/Director /updates on pain management every two years or where there is a of Nursing. significant change to practice in this area. The designated nurse for each resident will ensure that residents Admitting and/or are screened for the presence of pain on admission; where there designated nurse. is a significant change in the resident’s condition; following any injury or painful procedure and routinely every three months. Where any resident has pain, an assessment of their pain will be All registered nurses. carried out by using the appropriate pain assessment tool and a plan of care developed in consultation with the resident and /or representative and other healthcare staff involved in the resident’s care. Nurses will maintain their competence in the management of pain All registered nurses. for residents and communicate any competency / knowledge deficits to their line manager/Person in Charge. Care given to residents will be in accordance with the plan of care All healthcare staff developed and agreed by the resident and / or representative and providing care to other healthcare professionals involved in the resident’s care. residents. Changes in a resident’s condition will be reported to the senior All nurses, care assistants nurse in charge and changes to care will be communicated to all and other healthcare relevant healthcare professionals. professionals involved in the resident’s care. Care plans to address pain will include interventions to review pain All registered nurses. and the effectiveness of any treatment/intervention using the appropriate pain scale as per this policy.
3 | P a g e M a n a g e m e n t o f P a i n P o l i c y 0 7 0 3 2 0 1 6 7.0 Quick Reference Guide –Pain Management.
Screening for Presence of Pain. Routinely ask resident about the presence of any aching, soreness and / or discomfort: ◙ On admission as part of admission assessment. ◙ Every four months on reassessment ◙ When there is a significant change to care/condition. ◙ Before, during and after any painful diagnostic or therapeutic treatments ◙ Following any injury. ◙ If you feel a resident is unable to understand or convey adequate response either involve resident’s family/carer/representative or observe for behavioural cues that might indicate presence of pain such as facial expressions, verbalisations, body movements, changes in activity patterns, changes in interactions, mental status changes. ◙ If pain detected, go to the next step.
Pain Assessment. 1. Carry out comprehensive pain assessment: ◙ Use Brief Pain Inventory (BPI) short form for residents who can communicate. ◙ Use Abbey Pain Scale Assessment Tool for residents who cannot communicate. ◙ Liaise with residents’ GP to ensure a complete pain assessment includes: Resident or family / representative as appropriate Pain History General medical history. Physical Examination. Physical impact of pain. Psychosocial impact of pain Social impact of pain Medication and treatment review. 2 .Identify the intensity of the pain using pain scale for residents who can communicate, in order to determine current level of pain and to evaluate interventions.
Care Planning for Pain. Initiate Plan of Care to include: ◙ Resident and / or family/carer as appropriate. ◙ Collaboration with other nurses and healthcare professionals involved in the resident’s care. ◙ Referral to other disciplines / agencies as appropriate. ◙ Consider non-pharmacological treatments that may be effective and acceptable to the resident. ◙ Include interventions to prevent deterioration in functional ability. ◙ Include methods to monitor and evaluate effectiveness of care. ◙ Include use of a pain scale to monitor pain intensity and effectiveness of interventions/treatment. Document care plan. Communicate care plan to other healthcare team members involved in the residents care
Monitoring. ◙ Use pain scale to monitor pain intensity and effects of treatment ◙ Use verbal descriptor scale for residents who can communicate. ◙ Use Abbey pain scale for residents who cannot communicate. ◙ Administer pain medications as prescribed and use pain scale to monitor effectiveness of same. ◙ Monitor for common side effects of medications used. ◙ Liaise with resident’s GP. and other healthcare professionals involved in the resident’s care regarding effectiveness or otherwise of treatment. ◙ Amend/ update care plan in accordance with changing needs.
4 | P a g e M a n a g e m e n t o f P a i n P o l i c y 0 7 0 3 2 0 1 6 8.0 Pain Assessment and Care Planning Protocol.
1.4 Screening for and Identification of the Presence of Pain.
1.4.1 All residents should be routinely screened for the presence of pain: 9.0 On admission. 10.0 Where there is a significant change in the resident’s condition. 11.0 Before, during and after any painful diagnostic procedures or therapeutic treatments. 12.0 Following injury.
5 | P a g e M a n a g e m e n t o f P a i n P o l i c y 0 7 0 3 2 0 1 6 1.4.2 Screening for the presence of pain on admission should include asking the resident about the presence of any aching, soreness and / or discomfort.
1.4.3 Identifying any diseases or conditions the resident has, which could be causing pain, such as osteoarthritis.
1.4.4 Where the resident either complains of pain or there is reason to believe from other information/indicators that the resident has pain a comprehensive pain assessment should be completed.
1.4.5 Residents with advanced dementia who are unable to communicate or show signs of pain either verbally or non-verbally should be assessed for the presence of pain using the Abbey Pain Scale.
1.5 Hierarchical Approach to pain Assessment in Non-Verbal Residents.
The Hierarchical approach to pain assessment (The American Society for Pain Management Nursing’s Task Force on Pain Assessment in the Nonverbal Patient, 2011) recommends a comprehensive assessment and incorporates the following steps:
1. Ask older adults with dementia about their pain. Even older adults with mild to moderate dementia can respond to simple questions about their pain.
2. Use a standardized tool to assess pain intensity, such as the numerical rating scale (NRS) (0-10) or a verbal descriptor scale (VDS) (Specify which pain rating scale used in the Centre).
3. Use an observational tool to measure the presence of pain in older adults with dementia. The Centre uses the Abbey Pain Scale.
4. Ask family or usual caregivers as to whether the patient’s current behavior (e.g., crying out, restlessness) is different from their customary behavior. This change in behavior may signal pain.
5. If pain is suspected, consider a time-limited trial of an appropriate type and dose of an analgesic agent. In the Centre, the nurse must liaise with the resident’s medical practitioner if pain is suspected to discuss the need for a time limited trial of analgesia for the resident.
6. Thoroughly investigate behavior changes to rule out other causes. Use self-report and observational pain measures to evaluate the pain before and after administering the analgesic (as outlined in section 10.2).
6 | P a g e M a n a g e m e n t o f P a i n P o l i c y 0 7 0 3 2 0 1 6 1.5.1 The following should trigger assessment / re assessment of pain: ■ Any change in condition. ■ Diagnosis of a chronic, painful disease. ■ History of chronic, unexpressed pain. ■ Taking pain medication for > 72 hours. ■ Unexplained behavior changes, distress related behaviours or facial grimaces. ■ Family/others indicate pain is present.
1.5.2 Non-specific signs and symptoms that may indicate pain in people with dementia include: ■ Change in gait. ■ Loss of function. ■ Decreased activity levels. ■ Resisting certain movements during care. ■ Bracing, guarding, rubbing. ■ Fidgeting, increasing or recurring restlessness. ■ Frowning, grimacing, fearful facial expressions, grinding of teeth. ■ Change in behaviour. ■ Striking out, increasing or recurring agitation. ■ Eating or sleeping poorly. ■ Sighing, groaning, crying, breathing heavily. (American Medical Directors Association, 2012)
1.6 Comprehensive Pain Assessment.
1.6.1 Where there is information or indicators that suggest that a resident has pain, a comprehensive assessment of the cause and effects of the pain will be completed.
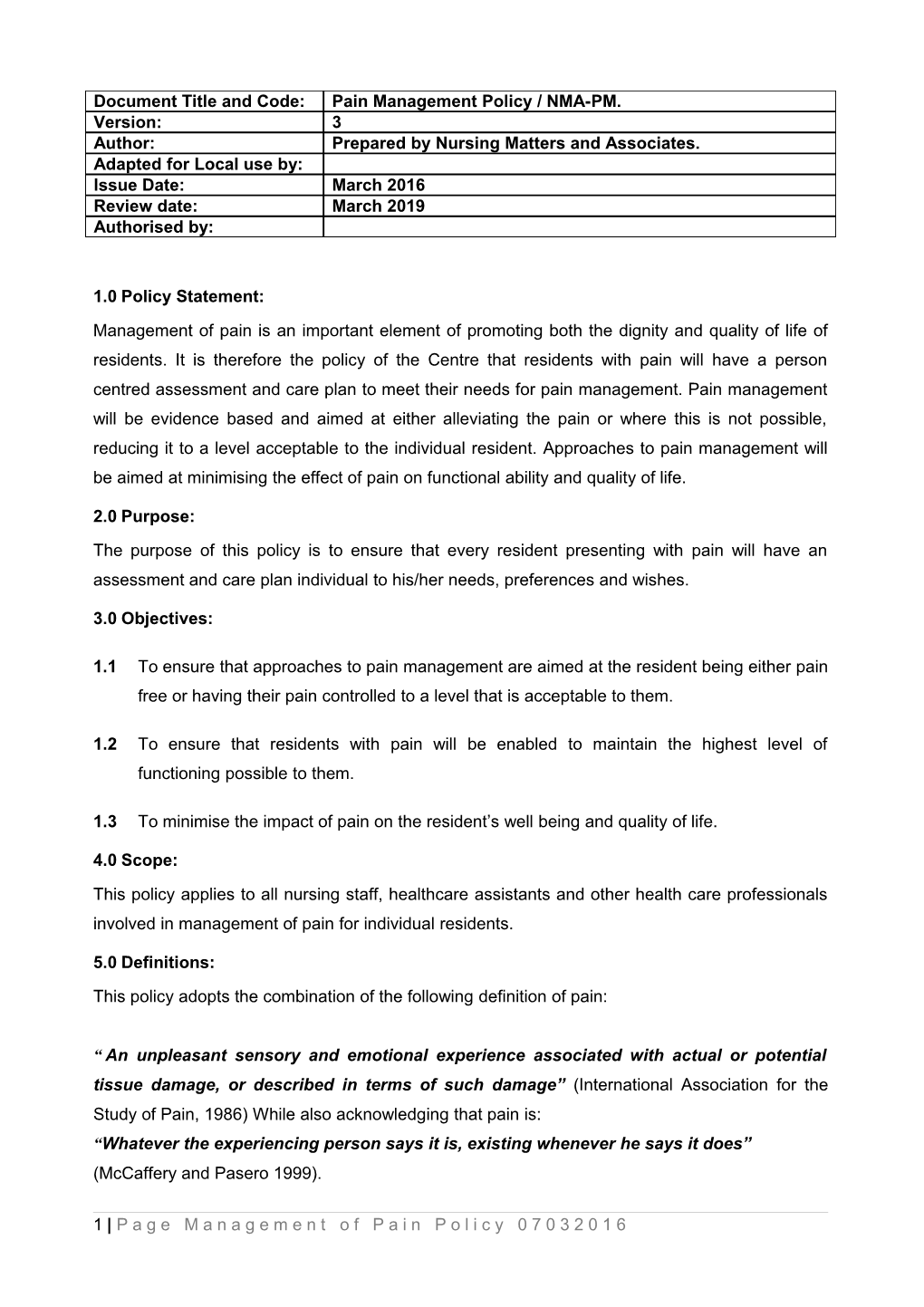
1.6.2 Fig 1 includes sample Mnemonics that can be used to assist the nurse in structuring a baseline assessment of pain. Fig 1: Mnemonics for Pain Assessment.
PQRST PAINED OLD CART P – Provoking or precipitating P – Place / location(s) of the O – Onset / when did the pain factors pain start? Q – Quality of pain (resident’s A – Amount refers to pain L – Location / where is your description e.g. sharp, intensity pain? achy etc.) R – Radiation of pain (does I – Intensifiers / what makes D – Duration – persistent/ the pain extend from the the pain worse periodic? site?)
7 | P a g e M a n a g e m e n t o f P a i n P o l i c y 0 7 0 3 2 0 1 6 S – Severity of the pain N – Nullifiers / what makes the C – Characteristics / what does it (intensity 1-10) pain better feel like? T – Timing (occasional v’s. E – Effects of pain on quality A – Aggravating factors / what constant) of life makes the pain worse?
D – Descriptors of the quality R – Relieving factors / what of pain (aching, burning, makes the pain better? throbbing etc.)
T – Treatment / what medications work for you? Do you have adverse effects from your medications?
1.6.3 The Brief Pain Inventory Assessment Form should be used for residents who can communicate or the Abbey Pain Scale for residents who are unable to communicate and/or have cognitive impairment.
1.6.4 The Abbey Pain Scale should be completed immediately following the delivery of personal care involving movement of the resident.
1.6.5 The nurse should also gather information regarding the following: ■ Any recent injuries or general / specific illnesses relevant to the pain. ■ Onset / duration of pain ■ Any recent injury or general illnesses that might be associated with the pain. ■ Location of pain ■ Frequency of pain ■ Level of pain ■ Relieving factors ■ Associated symptoms (e.g. nausea). ■ Impact of pain on activities of daily living, including sleep and mood. ■ Aggravating factors. ■ Coping strategies ■ Medications. ■ Treatments including medications that have been tried and their effectiveness or otherwise. ■ Known behavioural cues that may indicate the resident’s expression of pain. These may be known by the resident’s representative or other carer’s.
8 | P a g e M a n a g e m e n t o f P a i n P o l i c y 0 7 0 3 2 0 1 6 1.6.6 The resident’s vital signs should be recorded.
1.6.7 The assessing nurse should observe for any physical or behavioural symptoms related to pain e.g. sweating, pallor, sores, agitation, restlessness and so on.
1.6.8 The assessing nurse should document the assessment and observations on the relevant assessment form and place it in the resident’s care plan.
1.6.9 The assessing nurse should liaise with resident’s general practitioner / referring doctor and any other healthcare professional involved in the resident’s care to identify any other assessments that may be required and to develop a management plan.
1.6.10 Pain assessment, goals and care plan should be discussed with the resident and / or representative as appropriate.
1.6.11 A care plan to address the resident’s pain should be developed and documented.
13.0 Care Planning.
1.7 The assessing nurse should initiate a plan of care with the resident and / or the resident’s representative as appropriate and include the following activities:
1.7.1 The care plan should be based on the need to either eliminate the resident’s pain or to bring the pain to a level acceptable to the resident as well as minimising the impact of the pain on the resident’s functioning and quality of life. In order to direct interventions to meet these goals, the resident must be involved in both assessment and care planning.
1.7.2 As with all care planning the nurse must promote the resident’s autonomy and provide support to the resident with decision-making. This may necessitate the need to explore alternative communication methods where the resident has difficulty understanding information or making their wishes known (see the Centre’s Consent and Advocacy Policy for more information).
1.7.3 The nurse must liaise with the resident’s GP, where the resident has any new pain or where existing pain management interventions are not effective.
1.7.4 The nurse should also liaise with other healthcare professionals involved in the resident’s care.
1.7.5 The nurse should identify the need for specialist input and liaise with the resident, the resident’s representative as appropriate and the resident’s GP as required to arrange same. Specialist referral may include, for example, tissue viability expertise if pain is related to a wound, rheumatology services if the pain is related to arthritis and palliative care specialists for residents experiencing pain at the advanced stages of a life limiting illness.
9 | P a g e M a n a g e m e n t o f P a i n P o l i c y 0 7 0 3 2 0 1 6 1.7.6 The care plan should include the following information at a minimum: ■ The resident’s abilities with reference to pain management, for example, ability to communicate pain and the method of communication the resident uses to alert staff to the presence of pain e.g. can the resident verbally tell staff or point to the area of pain or does the resident display non-specific signs and symptoms such as moaning, groaning, restlessness, agitation etc. This might also include ability to respond to verbal pain scales; ability for self-care interventions that may be planned for pain prevention and / or management. ■ The resident’s wishes and preferences regarding the management of pain. ■ The problem statements – such as the type, cause and location of the pain. The care plan should provide information about the characteristics of the pain, using the resident’s own words where possible e.g. aching, hurting ■ Any other problems /needs related to the pain and how these will be addressed – if these are already outlined in another care plan, the nurse should refer to the other care plans, eg. Mobility. Where the pain is triggered or exacerbated by a particular activity such providing personal care or wound care, the care plan should address how the pain will be managed before, during and after the intervention/procedure e.g. administer analgesia 30 minutes prior to the procedure. ■ Interventions agreed to address the problems and needs identified. ■ Any risks related to either the pain itself or interventions agreed to manage the resident’s pain and how these will be addressed. This for example might include loss of functional ability or risks related to medication. Where these are addressed in other care plans, the care plan for pain should refer to those care plans. ■ Any aids or equipment that might be in use to manage the pain, eg. TENs. ■ Other professionals involved in managing the resident’s pain and instructions from these professionals that must be carried out, such as the use of massage. ■ Any monitoring required in relation to monitoring the resident. These include methods that will be employed to monitor the resident’s pain and evaluate effectiveness of care; use of a pain scale; observation of the resident for non-verbal cues and so on.
10 | P a g e M a n a g e m e n t o f P a i n P o l i c y 0 7 0 3 2 0 1 6 1.7.7 The care plan should include factors affecting the resident’s experience of pain e.g. anxiety, the need to have a person present to provide psychological support, depression, fatigue.
1.7.8 The care plan should identify any non-pharmacological treatments that have been agreed to manage the pain e.g. heat/cold therapy, massage, positioning, distraction, relaxation.
1.7.9 The care plan should also include general comfort measures identified to help the resident cope with pain.
1.7.10 The care plan must be communicated to all other nursing and care staff who are involved in the resident’s care.
1.8 Continuous Assessment / Monitoring of Unresolved Pain.
1.8.1 Nursing staff should continue to monitor the resident’s pain as outlined in the care plan until pain is either resolved or reduced to a level acceptable to them.
1.8.2 The resident’s pain should be formally re-assessed: At each new report of pain. After starting the treatment plan. If pain is suddenly not relieved by previously effective strategies. If there is unexpected, intense pain associated with altered vital signs; hypotension, tachycardia, or fever. Four monthly. Where a resident’s pain is new or is not yet effectively managed, at pre-determined intervals or before and after each pharmacological and non-pharmacological intervention, the Verbal Descriptor Scale should be used for residents who can communicate pain and the Abbey Pain Scale for residents who are unable to communicate pain and the nurse assessing the residents pain should document the pain intensity in the resident’s daily progress/narrative notes. All nurses should communicate to other members of the care team the need to report to the nurse on duty if a resident complains or shows indicators of pain The frequency of monitoring should be decided by the nurse preparing the care plan in collaboration with the resident, the resident’s medical practitioner and the care team, but where a resident continues to have pain, it should take place at least four hourly and allow for evaluation of specific pain management interventions such as pain medications. (eg. before and after). It is recommended that pain intensity should be assessed after the intervention has reached peak effect (15-30 minutes after parenteral drug therapy, 1 hour after immediate release
11 | P a g e M a n a g e m e n t o f P a i n P o l i c y 0 7 0 3 2 0 1 6 analgesic, 4 hours after sustained release analgesic or transdermal patch, 30 minutes after non-pharmacological intervention (Australian Pain Society, 2005). The resident’s designated nurse should ensure liaison with the resident’s doctor and other members of the healthcare team is carried out regarding the effectiveness or otherwise of treatments. Nurses should amend and update the care plan to reflect any changes to the residents care or condition.
Key Messages: Barriers that interfere with assessment and treatment in Older People.
The elderly often under report pain because it is often considered a normal part of aging The elderly sometimes choose to suffer in silence. This may be a culturally orientated response to pain or may be related to the high cost of medications and/or inability to access medical care. Caregivers’ and other’s misconceptions of the pain experience can influence the elderly person’s pain. Elderly persons with cognitive impairments or communication challenges may not be able to make their pain needs heard. Nurses must be observant of subtle clues such as guarding, wincing, moaning etc. The ability of elderly persons to swallow pills easily may be impaired due to dry mouth, swallowing difficulties or ill-fitting dentures. Fear of losing self-control Fear of addiction (Registered Nurses Association of Ontario, 2007)
12 | P a g e M a n a g e m e n t o f P a i n P o l i c y 0 7 0 3 2 0 1 6 14.0 Pain Intervention Guide.
Treatment Nursing Considerations
Pharmacological Treatments Paracetemol. ◙ Used as first line treatment for musculoskeletal pain and mild forms of neuropathic pain; infrequent or incident pain; breakthrough pain where controlled release analgesics do not control pain adequately. ◙ Should not exceed recommended dose of 4000mgs in a 24 hr. period. ◙ Risk of hepatotoxicity with fasting; dehydration; poor nutrition; large alcohol intake and underlying liver dysfunction.
Non-Steroidal Anti- ◙ Used with caution in the elderly. inflammatory Drugs ◙ Should be used in the lowest effective dose for the shortest duration (NSAIDS). possible. ◙ Side effects include peptic ulceration and haemorrhage; sodium and water retention; increased blood pressure; peripheral oedema. ◙ Special precaution required when using in residents with hypertension, cardiac failure or renal failure. ◙ Caution required when combined with ACE inhibitors. ◙ Care plans should include measures to monitor for and address side effects of NSAIDS. Opioids ◙ Controlled release opioids in low doses can provide effective relief for persistent pain where NSAIDS have proved inadequate. ◙ Codeine most widely used opioid therapy and can be recommended for incident, predictable, short lasting and infrequent pain. ◙ Controlled release opioids in relatively low doses can provide effective pain relief for persistent pain in older people when non-opioid treatments have proved inadequate. ◙ Older people are more sensitive to the actions of opioids meaning better pain relief but also more side effects. ◙ Education regarding side effects and their management should be provided to residents and / or relatives as appropriate. ◙ Side effects include constipation, nausea, and confusion. ◙ Constipation should be anticipated and care plans should include measures to prevent / manage constipation in residents on opioid therapy. ◙ Analgesic effects may be inhibited by many SSRIs and amitriptyline. ◙ Strong opioids such as morphine and oxycodone used for treatment of cancer pain and severe non-cancer pain ◙ Care plans should include measures to monitor for and address side effects of opioid therapy.
Adjuvant Analgesics. ◙ Antidepressants and antiepileptic agents can be useful for pain of neuropathic origin. ◙ Side effects include sedation, dizziness, and ataxia, which can predispose the resident to falls. Care plans should include measures to monitor for and address potential side effects for this group of drugs.
13 | P a g e M a n a g e m e n t o f P a i n P o l i c y 0 7 0 3 2 0 1 6 Treatment.Source: Australian PainNursing Society Considerations. (2005) Pain in Residential Aged Care Facilities.
Non- Pharmacological Treatments Superficial Heat. ◙ Indicated only for the management of acute pain 48hrs after onset. ◙ Should only be used in residents who have thermal sensation and adequate communication and cognitive abilities. ◙ Risk for superficial burns.
Superficial cold ◙ Not recommended as a pain relief strategy in older people. ◙ Prolonged cooling of the skin has the potential for tissue damage. ◙ Not well tolerated.
TENS ◙ Can relieve pain for more than 30 mins when used intermittently and may be applied for many hours for persistent pain. ◙ Those who cannot report on sensations are not suitable for TENS. ◙ Excessive levels of use can cause discomfort and may be painful. ◙ Recommended only for residents who have persistent pain and who can provide accurate feedback on the sensations evoked by the stimulator. ◙ Should only be used by a practitioner trained to use it. ◙ Procedures for informed consent should be adhered to when using pain management strategies. ◙ Liaison with referring doctor and other relevant healthcare personnel should inform treatment options. Exercise ◙ Active resident participation essential Strengthening. ◙ Should be selected according to resident’s cognitive, communicative Stretching and physical abilities. Aerobic ◙ Residents may be apprehensive about aggravating pain. ◙ Should only be used under direction of a physiotherapist and referring doctor.
Psycho-educational ◙ Supported by strong evidence for the management of persistent pain in strategies. the elderly. Cognitive-behavioural ◙ Should only be administered by a trained therapist. therapy – focus on ◙ Requires cognitive capacity and participation of the resident. changing the ◙ Liaise with resident’s GP/referring doctor re specialist referral for resident’s perception persistent pain that appears to be of a psychological nature. of the pain.
Complementary ◙ Often used for relief of pain and anxiety. Therapies. ◙ Clear approval and consent from the resident required. ◙ The facility must be informed before any form of complementary therapy is undertaken by a resident. ◙ Practitioners should be properly qualified to undertake delivery of the specific therapy.
Other adjunct ◙ Should be tailored to the needs of the resident. interventions. ◙ Evaluation of different approaches should be carried out. Relaxation. Diversion Music
14 | P a g e M a n a g e m e n t o f P a i n P o l i c y 0 7 0 3 2 0 1 6 15.0 References. 1. Health Information and Quality Standards (2009); National Quality Standards for Residential Settings for Older People. 2. Health Act, 2007 (Care and welfare for older people in designated centres) regulations (2013) 3. Herr K, Bjoro K, Steffensmeier J, Rakel B. Acute pain management in older adults. Iowa City (IA): University of Iowa Gerontological Nursing Interventions Research Center, Research Translation and Dissemination Core; 2006 Jul. accessed at http://www.nursing.uiowa.edu/consumers_patients/evidence_based.htm 4. Irish Hospice Foundation (2015) Pain Assessment and Management. Draft for Consultation accessed at IHF.ie 5. John A. Hartford Center of Geriatric Nursing Excellence (2011) Pain Assessment in the Patient Unable to Self-Report: Position Statement with Clinical Practice Recommendations. 6. Registered Nurses Association of Ontario (2013) Clinical Practice Guidelines: Assessment and Management of Pain. 7. Horgas, Ann L ; McLennon, Susan M.; Floetke, Amanda L. Pain Management in Persons With Dementia Alzheimers Care Quarterly Volume 4(4), October/November/December 2003, p 297–311. 8. McLennon SM. Persistent pain management. Iowa City (IA): University of Iowa Gerontological Nursing Interventions Research Center, Research Translation and Dissemination Core; 2005 Aug. accessed at: http://www.nursing.uiowa.edu/consumers_patients/evidence_based.htm 9. Australian Pain Society (2005) Pain in Residential Aged Care Facilities. Management Strategies. Australian Pain Society. Sydney. 10. NHS Quality Improvement Scotland. (2006) Best Practice Statement: Management of Chronic Pain in Adults. Accessed at www.nhsquality.org 11. Schofield P.A., Reid D. (2006) The Assessment and Management of Pain in Older Adults: A Systematic Review of the Literature. Burdett Trust for Nursing. Unpublished Report. 12. Moloney, S. L.; Kobayashi, M,; Holleran, E. A.; Mezey, M., Assessing Pain as a FIFTH VITAL SIGN IN LONG-TERM CARE FACILITIES: Recommendations from the Field. Journal of Gerontological Nursing. Volume 31(3), March 2005, p 16–24
15 | P a g e M a n a g e m e n t o f P a i n P o l i c y 0 7 0 3 2 0 1 6