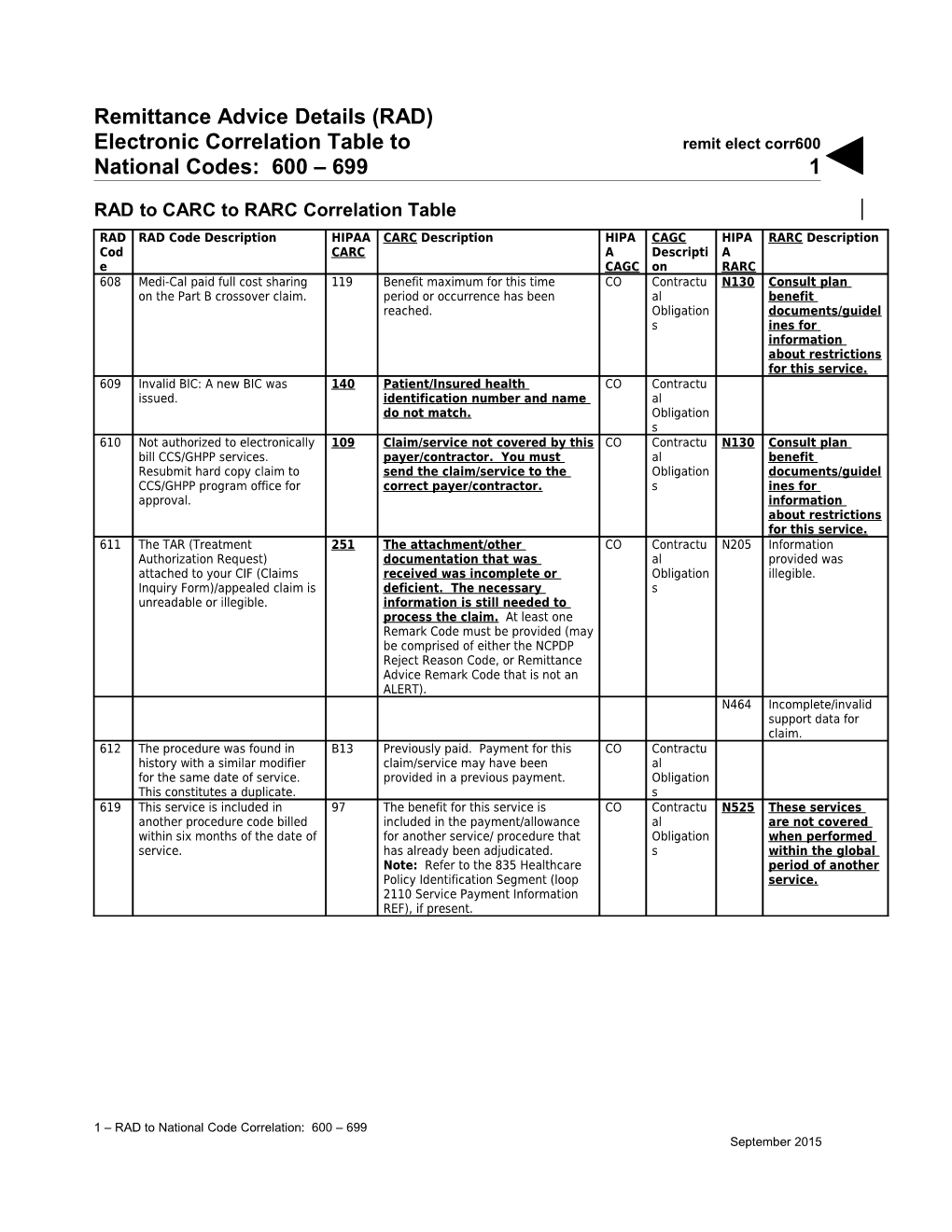
Remittance Advice Details (RAD) Electronic Correlation Table to remit elect corr600 National Codes: 600 – 699 1
RAD to CARC to RARC Correlation Table RAD RAD Code Description HIPAA CARC Description HIPA CAGC HIPA RARC Description Cod CARC A Descripti A e CAGC on RARC 608 Medi-Cal paid full cost sharing 119 Benefit maximum for this time CO Contractu N130 Consult plan on the Part B crossover claim. period or occurrence has been al benefit reached. Obligation documents/guidel s ines for information about restrictions for this service. 609 Invalid BIC: A new BIC was 140 Patient/Insured health CO Contractu issued. identification number and name al do not match. Obligation s 610 Not authorized to electronically 109 Claim/service not covered by this CO Contractu N130 Consult plan bill CCS/GHPP services. payer/contractor. You must al benefit Resubmit hard copy claim to send the claim/service to the Obligation documents/guidel CCS/GHPP program office for correct payer/contractor. s ines for approval. information about restrictions for this service. 611 The TAR (Treatment 251 The attachment/other CO Contractu N205 Information Authorization Request) documentation that was al provided was attached to your CIF (Claims received was incomplete or Obligation illegible. Inquiry Form)/appealed claim is deficient. The necessary s unreadable or illegible. information is still needed to process the claim. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT). N464 Incomplete/invalid support data for claim. 612 The procedure was found in B13 Previously paid. Payment for this CO Contractu history with a similar modifier claim/service may have been al for the same date of service. provided in a previous payment. Obligation This constitutes a duplicate. s 619 This service is included in 97 The benefit for this service is CO Contractu N525 These services another procedure code billed included in the payment/allowance al are not covered within six months of the date of for another service/ procedure that Obligation when performed service. has already been adjudicated. s within the global Note: Refer to the 835 Healthcare period of another Policy Identification Segment (loop service. 2110 Service Payment Information REF), if present.
1 – RAD to National Code Correlation: 600 – 699 September 2015 remit elect corr600 2
620 Claims were recycled the 16 Claim/service lacks information or CO Contractu N54 Claim information is maximum number of times. has submission/billing error(s) al inconsistent with Information requested from which is needed for adjudication. Do Obligation pre- provider on deferred TAR not use this code for claims s certified/authorized (Treatment Authorization attachment(s)/other services. Request) has not been documentation. At least one received. Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT). Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. N29 Missing documentation/orde rs/ notes/summary/rep ort/ chart. N225 Incomplete/invalid documentation/ orders/notes/ summary/report/ch art.
1 – RAD to National Code Correlation: 600 – 699 __2006 Remittance Advice Details (RAD) Electronic Correlation Table to remit elect corr600 National Codes: 600 – 699 3
RAD RAD Code Description HIPAA CARC Description HIPA CAGC HIPA RARC Description Cod CARC A Descripti A e CAGC on RARC 621 The monthly/yearly limit for this 119 Benefit maximum for this time CO Contractu N362 The number of days procedure has been exceeded. period or occurrence has been al or units of service The claim is denied. reached. Obligation exceeds the s acceptable maximum. N435 Exceeds number/ frequency approved/ allowed within time period without support documentation. 622 Coinsurance and deductible are 97 The benefit for this service is CO Contractu N130 Consult plan not separately payable on included in the al benefit inpatient stay of Medicare Part payment/allowance for another Obligation documents/guidel B-only covered recipient. service/procedure that has s ines for already been adjudicated. Note: information Refer to the 835 Healthcare about restrictions Policy Identification Segment for this service. (loop 2110 Service Payment Information REF), if present. 623 The claim has been denied due B20 Procedure/service was partially CO Contractu to OHC (Other Health Coverage) or fully furnished by another al having paid in full or OHC provider. Obligation payment exceeding s Medi-Cal allowed amount. 624 Non-emergency services are 40 Charges do not meet qualifications CO Contractu not payable for limited scope for emergent/urgent care. Note: al 100 percent recipients. Refer to the 835 Healthcare Policy Obligation Identification Segment (loop 2110 s Service Payment Information REF), if present. 625 A CIF (Claims Inquiry Form) 251 The attachment/other CO Contractu N225 Incomplete/invalid cannot be used to request documentation that was al documentation/ resubmission of a denied claim received was incomplete or Obligation orders/notes/ if the inpatient provider also deficient. The necessary s summary/report/ch wants to add or delete claim information is still needed to art. lines. process the claim. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT). 626 Non-emergency related 40 Charges do not meet qualifications CO Contractu services are not payable for aid for emergency/urgent care. Note: al code 55 recipients. Refer to the 835 Healthcare Policy Obligation Identification Segment (loop 2110 s Service Payment Information REF), if present. 627 The inpatient days or date of 15 The authorization number is missing, CO Contractu N54 Claim information is service billed on the claim does invalid, or does not apply to the al inconsistent with not match the CCS (California billed services or provider. Obligation pre- Children’s Services) s certified/authorized Authorization Form. services.
1 – RAD to National Code Correlation: 600 – 699 September 2015 remit elect corr600 2
628 The Medi-Cal provider/recipient 16 Claim/service lacks information CO Contractu N54 Claim information is IDs or the service billed is not or has submission/billing error(s) al inconsistent with consistent with the CCS which is needed for adjudication. Obligation pre- (California Children’s Services) Do not use this code for claims s certified/authorized Authorization Form. attachment(s)/other services. documentation. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT). Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. N433 Resubmit this claim using only your National Provider Identifier (NPI).
1 – RAD to National Code Correlation: 600 – 699 September 2015 remit elect corr600 3
RAD RAD Code Description HIPAA CARC Description HIPA CAGC HIPA RARC Description Cod CARC A Descripti A e CAGC on RARC 629 Surgery other than a common 97 The benefit for this service is CO Contractu N130 Consult plan office procedure was not billed included in the al benefit for this patient on the same payment/allowance for another Obligation documents/guidel date of service. Operating service/procedure that has s ines for room payable at treatment already been adjudicated. Note: information room level, or at zero. Refer to the 835 Healthcare about restrictions Recovery room payable at zero. Policy Identification Segment for this service. (loop 2110 Service Payment Information REF), if present. 630 The submitted documentation 251 The attachment/other CO Contractu N225 Incomplete/invalid was not adjudicated. The documentation that was al documentation/orde length of time actually spent received was incomplete or Obligation rs/ monitoring the service must be deficient. The necessary s notes/summary/rep indicated. information is still needed to ort/ process the claim. At least one chart. Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT). N464 Incomplete/invalid support data for claim. 631 TAR (Treatment Authorization B13 Previously paid. Payment for CO Contractu Request) authorized outpatient this claim/service may have been al psychiatry services have been provided in a previous payment. Obligation previously reimbursed. These s non-TAR services are not payable for the same period of time as TAR-authorized psychiatric services. 632 Invalid disproportionate share 96 Non-covered charge(s). At least CO Contractu N130 Consult plan code for dates of service on or one Remark Code must be al benefit after July 1, 1992. (Chapter 279, provided (may be comprised of Obligation documents/guidel Senate Bill 855. Chapter 1046, either the NCPDP Reject Reason s ines for Senate Bill 146.) [sic] Code, or Remittance Advice information Remark Code that is not an about restrictions ALERT). Note: Refer to the 835 for this service. Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. 633 TPN (Total Parenteral Nutrition)/ 16 Claim/service lacks information or CO Contractu N225 Incomplete/invalid Compound prescription has submission/billing error(s) al documentation/orde documentation is incomplete or which is needed for adjudication. Do Obligation rs/ incorrect. A letter has been not use this code for claims s notes/summary/rep sent to the address on the attachment(s)/other ort/ claim indicating the needed documentation. At least one chart. correction. Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT). Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. N388 Missing/incomplete/ invalid prescription number.
1 – RAD to National Code Correlation: 600 – 699 September 2015 remit elect corr600 6
N464 Incomplete/invalid support data for claim.
1 – RAD to National Code Correlation: 600 – 699 September 2015 remit elect corr600 3
RAD RAD Code Description HIPAA CARC Description HIPA CAGC HIPA RARC Description Cod CARC A Descripti A e CAGC on RARC 634 CLIA (Clinical Laboratory 16 Claim/service lacks information CO Contractu MA12 Missing/incomplete/ Improvement Amendment) or has submission/billing error(s) al 0 invalid CLIA laboratory number is not on file which is needed for adjudication. Obligation certification on date of service. Do not use this code for claims s number. attachment(s)/other documentation. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT). Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. N570 Missing/incomple te/ invalid credentialing data N463 Missing support data for claim. 635 The statement of medical 16 Claim/service lacks information or CO Contractu MA70 Missing/incomplete/ necessity requires a physician’s has submission/billing error(s) al invalid provider signature. which is needed for adjudication. Do Obligation representative not use this code for claims s signature. attachment(s)/other documentation. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT). Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. N463 Missing support data for claim. 636 Medi/Medi-Charpentier claim 16 Claim/service lacks information or CO Contractu N4 Missing/incomplete/ does not meet submission has submission/billing error(s) al invalid prior requirements. Verify that the which is needed for adjudication. Do Obligation insurance carrier correct codes were used; dates not use this code for claims s EOB. of service match (Explanation attachment(s)/other of Medicare Benefits documentation. At least one (EOMB)/Medicare Remittance Remark Code must be provided (may Notice (MRN); EOMB/MRN and be comprised of either the NCPDP Medi-Cal RADs are attached. Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT). Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. N29 Missing documentation/ orders/notes/summ ary/ report/chart. N463 Missing support data for claim.
1 – RAD to National Code Correlation: 600 – 699 September 2015 remit elect corr600 4
637 Maximum allowed per month 119 Benefit maximum for this time CO Contractu N435 Exceeds has been paid. Medical period or occurrence has been al number/frequenc justification is required for reached. Obligation y approved additional dialysis visits. s /allowed within time period without support documentation.
1 – RAD to National Code Correlation: 600 – 699 September 2015 remit elect corr600 9
RAD RAD Code Description HIPAA CARC Description HIPA CAGC HIPA RARC Description Cod CARC A Descripti A e CAGC on RARC 638 The rendering provider number 16 Claim/service lacks information CO Contractu N290 Missing/incomplete/ is missing or invalid. or has submission/billing error(s) al invalid rendering which is needed for adjudication. Obligation provider primary Do not use this code for claims s identifier. attachment(s)/other documentation. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT). Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. N433 Resubmit this claim using only your National Provider Identifier (NPI). 639 Recipient is not eligible for 252 An attachment/other CO Contractu MA04 Secondary payment Medi-Cal benefits without documentation is required to al cannot be complete denial coverage from adjudicate this claim/service. At Obligation considered without Prudential. (16, 109) least one Remark Code must be s the identity of or provided (may be comprised of payment either the NCPDP Reject Reason information from Code, or Remittance Advice the primary payer. Remark Code that is not an The information ALERT). was either not reported or was illegible. N406 This service is only covered when the recipient’s insurer(s) do not provide coverage for the service. 640 Recipient is not eligible for 252 An attachment/other CO Contractu MA04 Secondary payment Medi-Cal benefits without documentation is required to al cannot be complete denial of coverage adjudicate this claim/service. At Obligation considered without from the Medicare Health least one Remark Code must be s the identity of or Maintenance Organization provided (may be comprised of payment (HMO), Competitive Medical either the NCPDP Reject Reason information from Plan (CMP) or Health Care Code, or Remittance Advice the primary payer. Prepayment Plan (HCPP). Medi- Remark Code that is not an The information Cal is not obligated for plan ALERT). was either not services when the recipient reported or was chooses not to go to a plan illegible. provider. N406 This service is only covered when the recipient’s insurer(s) do not provide coverage for the service.
1 – RAD to National Code Correlation: 600 – 699 September 2015 remit elect corr600 10
641 Recipient is not eligible for 16 Claim/service lacks information or CO Contractu MA04 Secondary payment Medi-Cal benefits without has submission/billing error(s) al cannot be complete denial of coverage which is needed for adjudication. Do Obligation considered without from Mutual of Omaha. not use this code for claims s the identity of or attachment(s)/other payment documentation. At least one information from Remark Code must be provided (may the primary payer. be comprised of either the NCPDP The information Reject Reason Code, or Remittance was either not Advice Remark Code that is not an reported or was ALERT). Note: Refer to the 835 illegible. Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. N406 This service is only covered when the recipient’s insurer(s) do not provide coverage for the service. N463 Missing support data for claim.
1 – RAD to National Code Correlation: 600 – 699 November 2007 remit elect corr600 11
RAD RAD Code Description HIPAA CARC Description HIPA CAGC HIPA RARC Description Cod CARC A Descripti A e CAGC on RARC 642 Recipient is not eligible for 16 Claim/service lacks information or CO Contractu MA04 Secondary payment Medi-Cal benefits without has submission/billing error(s) al cannot be complete denial of coverage which is needed for adjudication. Do Obligation considered without from Metropolitan Life. not use this code for claims s the identity of or attachment(s)/other payment documentation. At least one information from Remark Code must be provided (may the primary payer. be comprised of either the NCPDP The information Reject Reason Code, or Remittance was either not Advice Remark Code that is not an reported or was ALERT). Note: Refer to the 835 illegible. Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. N406 This service is only covered when the recipient’s insurer(s) do not provide coverage for the service. N463 Missing support data for claim. 643 Recipient not eligible for Medi- 16 Claim/service lacks information or CO Contractu MA04 Secondary payment Cal benefits without complete has submission/billing error(s) al cannot be denial of coverage from John which is needed for adjudication. Do Obligation considered without Hancock Mutual Life. not use this code for claims s the identity of or attachment(s)/other payment documentation. At least one information from Remark Code must be provided (may the primary payer. be comprised of either the NCPDP The information Reject Reason Code, or Remittance was either not Advice Remark Code that is not an reported or was ALERT). Note: Refer to the 835 illegible. Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. N406 This service is only covered when the recipient’s insurer(s) do not provide coverage for the service. N463 Missing support data for claim. 644 Recipient not eligible for Medi- 16 Claim/service lacks information or CO Contractu MA04 Secondary payment Cal benefits without complete has submission/billing error(s) al cannot be denial of coverage from which is needed for adjudication. Do Obligation considered without Equicor/Equitable. not use this code for claims s the identity of or attachment(s)/other payment documentation. At least one information from Remark Code must be provided (may the primary payer. be comprised of either the NCPDP The information Reject Reason Code, or Remittance was either not Advice Remark Code that is not an reported or was ALERT). Note: Refer to the 835 illegible. Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present.
1 – RAD to National Code Correlation: 600 – 699 September 2015 remit elect corr600 12
N406 This service is only covered when the recipient’s insurer(s) do not provide coverage for the service. N463 Missing support data for claim.
1 – RAD to National Code Correlation: 600 – 699 September 2015 remit elect corr600 13
RAD RAD Code Description HIPAA CARC Description HIPA CAGC HIPA RARC Description Cod CARC A Descripti A e CAGC on RARC 645 Recipient not eligible for Medi- 16 Claim/service lacks information or CO Contractu MA04 Secondary payment Cal benefits without complete has submission/billing error(s) al cannot be denial of coverage from which is needed for adjudication. Do Obligation considered without Travelers. not use this code for claims s the identity of or attachment(s)/other payment documentation. At least one information from Remark Code must be provided (may the primary payer. be comprised of either the NCPDP The information Reject Reason Code, or Remittance was either not Advice Remark Code that is not an reported or was ALERT). Note: Refer to the 835 illegible. Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. N406 This service is only covered when the recipient’s insurer(s) do not provide coverage for the service. N463 Missing support data for claim. 646 Recipient not eligible for Medi- 16 Claim/service lacks information or CO Contractu MA04 Secondary payment Cal benefits without complete has submission/billing error(s) al cannot be denial of coverage from which is needed for adjudication. Do Obligation considered without Connecticut General CIGNA. not use this code for claims s the identity of or attachment(s)/other payment documentation. At least one information from Remark Code must be provided (may the primary payer. be comprised of either the NCPDP The information Reject Reason Code, or Remittance was either not Advice Remark Code that is not an reported or was ALERT). Note: Refer to the 835 illegible. Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. N406 This service is only covered when the recipient’s insurer(s) do not provide coverage for the service. N463 Missing support data for claim. 647 Recipient not eligible for Medi- 16 Claim/service lacks information or CO Contractu MA04 Secondary payment Cal benefits without complete has submission/billing error(s) al cannot be denial of coverage from private which is needed for adjudication. Do Obligation considered without insurance carrier. not use this code for claims s the identity of or attachment(s)/other payment documentation. At least one information from Remark Code must be provided (may the primary payer. be comprised of either the NCPDP The information Reject Reason Code, or Remittance was either not Advice Remark Code that is not an reported or was ALERT). Note: Refer to the 835 illegible. Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present.
1 – RAD to National Code Correlation: 600 – 699 September 2015 remit elect corr600 6
N406 This service is only covered when the recipient’s insurer(s) do not provide coverage for the service. N463 Missing support data for claim.
1 – RAD to National Code Correlation: 600 – 699 March 2007 remit elect corr600 7
RAD RAD Code Description HIPAA CARC Description HIPA CAGC HIPA RARC Description Cod CARC A Descripti A e CAGC on RARC 648 Recipient not eligible for Medi- 16 Claim/service lacks information or CO Contractu MA04 Secondary payment Cal benefits without complete has submission/billing error(s) al cannot be denial of coverage from Great which is needed for adjudication. Do Obligation considered without West Life Assurance. not use this code for claims s the identity of or attachment(s)/other payment documentation. At least one information from Remark Code must be provided (may the primary payer. be comprised of either the NCPDP The information Reject Reason Code, or Remittance was either not Advice Remark Code that is not an reported or was ALERT). Note: Refer to the 835 illegible. Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. N406 This service is only covered when the recipient’s insurer(s) do not provide coverage for the service. N463 Missing support data for claim. 649 Recipient not eligible for Medi- 16 Claim/service lacks information or CO Contractu MA04 Secondary payment Cal benefits without complete has submission/billing error(s) al cannot be denial of coverage from which is needed for adjudication. Do Obligation considered without Provident Life and Accident. not use this code for claims s the identity of or attachment(s)/other payment documentation. At least one information from Remark Code must be provided (may the primary payer. be comprised of either the NCPDP The information Reject Reason Code, or Remittance was either not Advice Remark Code that is not an reported or was ALERT). Note: Refer to the 835 illegible. Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. N406 This service is only covered when the recipient’s insurer(s) do not provide coverage for the service. N463 Missing support data for claim. 650 Recipient not eligible for Medi- 16 Claim/service lacks information or CO Contractu MA04 Secondary payment Cal benefits without complete has submission/billing error(s) al cannot be denial of coverage from which is needed for adjudication. Do Obligation considered without Principal Financial Group. not use this code for claims s the identity of or attachment(s)/other payment documentation. At least one information from Remark Code must be provided (may the primary payer. be comprised of either the NCPDP The information Reject Reason Code, or Remittance was either not Advice Remark Code that is not an reported or was ALERT). Note: Refer to the 835 illegible. Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present.
1 – RAD to National Code Correlation: 600 – 699 April 2008 remit elect corr600 16
N406 This service is only covered when the recipient’s insurer(s) do not provide coverage for the service. N463 Missing support data for claim.
1 – RAD to National Code Correlation: 600 – 699 September 2015 remit elect corr600 17
RAD RAD Code Description HIPAA CARC Description HIPA CAGC HIPA RARC Description Cod CARC A Descripti A e CAGC on RARC 651 Recipient not eligible for Medi- 16 Claim/service lacks information or CO Contractu MA04 Secondary payment Cal benefits without complete has submission/billing error(s) al cannot be denial of coverage from Pacific which is needed for adjudication. Do Obligation considered without Mutual Life Insurance. not use this code for claims s the identity of or attachment(s)/other payment documentation. At least one information from Remark Code must be provided (may the primary payer. be comprised of either the NCPDP The information Reject Reason Code, or Remittance was either not Advice Remark Code that is not an reported or was ALERT). Note: Refer to the 835 illegible. Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. N406 This service is only covered when the recipient’s insurer(s) do not provide coverage for the service. N463 Missing support data for claim. 652 Recipient not eligible for Medi- 16 Claim/service lacks information or CO Contractu MA04 Secondary payment Cal benefits without complete has submission/billing error(s) al cannot be denial of coverage from Alta which is needed for adjudication. Do Obligation considered without Health Strategies. not use this code for claims s the identity of or attachment(s)/other payment documentation. At least one information from Remark Code must be provided (may the primary payer. be comprised of either the NCPDP The information Reject Reason Code, or Remittance was either not Advice Remark Code that is not an reported or was ALERT). Note: Refer to the 835 illegible. Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. N406 This service is only covered when the recipient’s insurer(s) do not provide coverage for the service. N463 Missing support data for claim. 653 Recipient not eligible for Medi- 16 Claim/service lacks information or CO Contractu MA04 Secondary payment Cal benefits without complete has submission/billing error(s) al cannot be denial of coverage from AARP. which is needed for adjudication. Do Obligation considered without not use this code for claims s the identity of or attachment(s)/other payment documentation. At least one information from Remark Code must be provided (may the primary payer. be comprised of either the NCPDP The information Reject Reason Code, or Remittance was either not Advice Remark Code that is not an reported or was ALERT). Note: Refer to the 835 illegible. Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present.
1 – RAD to National Code Correlation: 600 – 699 September 2015 remit elect corr600 18
N406 This service is only covered when the recipient’s insurer(s) do not provide coverage for the service. N463 Missing support data for claim.
1 – RAD to National Code Correlation: 600 – 699 September 2015 remit elect corr600 19
RAD RAD Code Description HIPAA CARC Description HIPA CAGC HIPA RARC Description Cod CARC A Descripti A e CAGC on RARC 654 Recipient not eligible for Medi- 16 Claim/service lacks information or CO Contractu MA04 Secondary payment Cal benefits without complete has submission/billing error(s) al cannot be denial of coverage from Allstate which is needed for adjudication. Do Obligation considered without Life Insurance. not use this code for claims s the identity of or attachment(s)/other payment documentation. At least one information from Remark Code must be provided (may the primary payer. be comprised of either the NCPDP The information Reject Reason Code, or Remittance was either not Advice Remark Code that is not an reported or was ALERT). Note: Refer to the 835 illegible. Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. N406 This service is only covered when the recipient’s insurer(s) do not provide coverage for the service. N463 Missing support data for claim. 655 Recipient not eligible for Medi- 16 Claim/service lacks information or CO Contractu MA04 Secondary payment Cal benefits without complete has submission/billing error(s) al cannot be denial of coverage from New which is needed for adjudication. Do Obligation considered without York Life Insurance. not use this code for claims s the identity of or attachment(s)/other payment documentation. At least one information from Remark Code must be provided (may the primary payer. be comprised of either the NCPDP The information Reject Reason Code, or Remittance was either not Advice Remark Code that is not an reported or was ALERT). Note: Refer to the 835 illegible. Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. N406 This service is only covered when the recipient’s insurer(s) do not provide coverage for the service. N463 Missing support data for claim. 656 Recipient not eligible for Medi- 252 An attachment/other CO Contractu MA04 Secondary payment Cal benefits without proof of documentation is required to al cannot be denial of coverage from the adjudicate this claim/service. At Obligation considered without Healthy Families (HF) Program. least one Remark Code must be s the identity of or Call 1-800-880-5305 for more provided (may be comprised of payment information. either the NCPDP Reject Reason information from Code, or Remittance Advice the primary payer. Remark Code that is not an The information ALERT). was either not reported or was illegible.
1 – RAD to National Code Correlation: 600 – 699 June 2010 remit elect corr600 20
N406 This service is only covered when the recipient’s insurer(s) do not provide coverage for the service. 657 Recipient not eligible for Medi- 252 An attachment/other CO Contractu MA04 Secondary payment Cal benefits until documentation is required to al cannot be payment/denial information is adjudicate this claim/service. At Obligation considered without given from other insurance least one Remark Code must be s the identity of or carrier. provided (may be comprised of payment either the NCPDP Reject Reason information from Code, or Remittance Advice the primary payer. Remark Code that is not an The information ALERT). was either not reported or was illegible. N406 This service is only covered when the recipient’s insurer(s) do not provide coverage for the service.
1 – RAD to National Code Correlation: 600 – 699 September 2015 remit elect corr600 21
RAD RAD Code Description HIPAA CARC Description HIPA CAGC HIPA RARC Description Cod CARC A Descripti A e CAGC on RARC 658 This claim has been denied 96 Non-covered charge(s). At least CO Contractu N10 Payment based based on additional review by one Remark Code must be provided al on the findings of Audits and Investigations. (may be comprised of either the Obligation a review NCPDP Reject Reason [sic] Code, or s organization/ Remittance Advice Remark Code professional that is not an ALERT). Note: Refer consult/manual to the 835 Healthcare Policy adjudication/medi Identification Segment (loop cal advisor/dental 2110 Service Payment advisor/peer Information REF), if present. review. 663 Attachments/comments are 252 An attachment/other CO Contractu N225 Incomplete/invali required. Please resubmit documentation is required to al d claim. adjudicate this claim/service. At Obligation documentation/or least one Remark Code must be s ders/notes/summ provided (may be comprised of ary/report/chart. either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT). N463 Missing support data for claim. N517 Resubmit a new claim with the requested information. 664 No match found to the 251 The attachment/other CO Contract N206 The supporting Attachment Control Number documentation that was ual documentation (ACN) indicated on received was incomplete or Obligatio does not match electronic claim. deficient. The necessary ns the claim. information is still needed to process the claim. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT). 665 The days supply billed exceeds 154 Payer deems the information CO Contractu the days supply limit. submitted does not support this days al supply. Obligation s 666 This claim exceeds $599.00 per 96 Non-covered charge(s). At least CO Contractu N61 Rebill services on calendar year or 10 claim lines one Remark Code must be provided al separate claims. per calendar year. (may be comprised of either the Obligation NCPDP Reject Reason [sic] Code, or s Remittance Advice Remark Code that is not an ALERT). Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. 667 The date of issue entered does 251 The attachment/other CO Contractu N225 Incomplete/invalid not match. documentation that was al documentation/ received was incomplete or Obligation orders/notes/ deficient. The necessary s summary/report/ch information is still needed to art. process the claim. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT).
1 – RAD to National Code Correlation: 600 – 699 September 2015 remit elect corr600 22
668 The prescription number is a B13 Previously paid. Payment for this CO Contractu duplicate of a previously paid claim/service may have been al claim. provided in a previous payment. Obligation s 669 Fee for Service/Managed Care 16 Claim/service lacks information CO Contractu M62 Missing/incomplete/ Network (FFS/MCN) Referral or has submission/billing error(s) al invalid treatment Authorization Form (RAF) has which is needed for adjudication. Obligation authorization code. expired. Contact FFS/MCN plan. Do not use this code for claims s attachment(s)/other documentation. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT). Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present.
1 – RAD to National Code Correlation: 600 – 699 September 2015 remit elect corr600 23
RAD RAD Code Description HIPAA CARC Description HIPA CAGC HIPA RARC Description Cod CARC A Descripti A e CAGC on RARC 670 Fee for Service/Managed Care 15 The authorization number is missing, CO Contractu N517 Resubmit a new Network (FFS/MCN) Referral invalid, or does not apply to the al claim with the Authorization Form (RAF) billed services or provider. Obligation requested required for FFS/MCN plan s information. service rendered by a non- FFS/MCN provider. Contact FFS/MCN plan. 671 State initiated reprocessing of 96 Non-covered charge(s). At least CO Contractu MA67 Correction to a prior claim. This claim has been one Remark Code must be provided al claim. assigned a new CCN (Claim (may be comprised of either the Obligation Control Number). NCPDP Reject Reason [sic] Code, or s Remittance Advice Remark Code that is not an ALERT). Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. N377 Payment based on a processed replacement claim. 672 The claim exceeds the monthly 119 Benefit maximum for this time CO Contractu N362 The number of days reimbursement limit for period or occurrence has been al or units of service incontinence supplies. reached. Obligation exceeds the s acceptable maximum. 673 The claim exceeds the monthly 197 Precertification/authorization/no CO Contractu N435 Exceeds number/ prescription limit. The claim tification absent. al frequency requires an approved TAR Obligation approved/ (Treatment Authorization s allowed within time Request). period without support documentation. 674 Discharge rate not payable if 97 The benefit for this service is CO Contractu N130 Consult plan readmitted within 24 hours for included in the al benefit the same or related condition. payment/allowance for another Obligation documents/guidel service/procedure that has s ines for already been adjudicated. Note: information Refer to the 835 Healthcare about restrictions Policy Identification Segment for this service. (loop 2110 Service Payment Information REF), if present. 675 Fee for Service/Managed Care 16 Claim/service lacks information CO Contractu N54 Claim information Network (FFS/MCN) Referral or has submission/billing error(s) al is inconsistent Authorization Form (RAF) which is needed for adjudication. Obligation with pre- number does not match claim. Do not use this code for claims s certified/authoriz Verify RAF number on claim and attachment(s)/other ed services. contact the FFS/MCN plan if documentation. At least one necessary. Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT). Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. N206 The supporting documentation does not match the claim.
1 – RAD to National Code Correlation: 600 – 699 August 2012 remit elect corr600 24
RAD RAD Code Description HIPAA CARC Description HIPA CAGC HIPA RARC Description Cod CARC A Descripti A e CAGC on RARC 676 Outcome data for CDP: EWC 252 An attachment/other CO Contractu N29 Missing (Cancer Detection Program: documentation is required to al documentation/orde Every Woman Counts) claims adjudicate this claim/service. At Obligation rs/ (aid code 9A) must be listed for least one Remark Code must be s notes/summary/rep each procedure code. provided (may be comprised of ort/ chart. either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT). N463 Missing support data for claim. 677 Denied by SCR (Special Claims P14 The Benefit for this Service is CO Contractu M86 Service denied Review) – this service is included in the al because payment reimbursed under another payment/allowance for another Obligation already made for procedure. service/procedure that has been s same/similar performed on the same day. procedure within Note: Refer to the 835 set time frame. Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. To be used for Property and Casualty only. 678 Denied by SCR (Special Claims 251 The attachment/other CO Contractu N29 Missing Review) – electronic billing is documentation that was al documentation/ not appropriate for services received was incomplete or Obligation orders/notes/summ that require supporting deficient. The necessary s ary/ documentation. information is still needed to report/chart. process the claim. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT). N225 Incomplete/invalid documentation/orde rs/ notes/summary/rep ort/ chart. 680 EAPC (Expanded Access to 31 Patient cannot be identified as our CO Contractu Primary Care) claims for CHDP insured. al (Child Health and Disability Obligation Prevention) health assessment s are not reimbursable when a patient has paid a Share of Cost. 681 EAPC (Expanded Access to 109 Claim not covered by this CO Contractu N130 Consult plan Primary Care) claims are not payer/contractor. You must send the al benefit reimbursable when a patient claim to the correct Obligation documents/guidel has Other Health Coverage or is payer/contractor. s ines for Medi-Cal eligible. information about restrictions for this service. N23 Patient liability may be affected due to coordination of benefits with other Carriers and/or maximum benefit provisions.
1 – RAD to National Code Correlation: 600 – 699 June 2010 remit elect corr600 25
682 The provider is not on 96 Non-covered charge(s). At least CO Contractu N130 Consult plan EAPC/MSSP file, or grant one Remark Code must be al benefit amount for fiscal year provided (may be comprised of Obligation documents/guidel exceeded. either the NCPDP Reject Reason s ines for [sic] Code, or Remittance Advice information Remark Code that is not an about restrictions ALERT). Note: Refer to the 835 for this service. Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. 683 The CPSP (Comprehensive 49 This is a non-covered service CO Contractu M86 Service denied Perinatal Services Program) because it is a al because payment initial comprehensive code routine/preventive exam or a Obligation already made for (Z6500) and any initial diagnostic/screening procedure s same/similar individual assessment code done in conjunction with a procedure within (Z6200, Z6300, Z6402) are not routine/preventive exam. Note: set time frame. reimbursed in conjunction with Refer to the 835 Healthcare each other. Policy Identification Segment (loop 2110 Service Payment Information REF), if present.
1 – RAD to National Code Correlation: 600 – 699 September 2015 remit elect corr600 26
RAD RAD Code Description HIPAA CARC Description HIPA CAGC HIPA RARC Description Cod CARC A Descripti A e CAGC on RARC 684 Non-capitated inpatient 197 Precertification/authorization/notifica CO Contractu psychiatric mental health tion absent. al services for a PCCM (Primary Obligation Care Case Management) s recipient requires an approved TAR Form 18-3 (Treatment Authorization Form, Request for Mental Health Stay in Hospital), from the County Mental Health Plan. 685 Ancillary charges are required 97 The benefit for this service is CO Contractu N19* Procedure code for billing but are not separately included in the al incidental to reimbursable. Use other non- payment/allowance for another Obligation primary contract, non-HSM provider service/procedure that has s procedure. number to bill take-home drugs already been adjudicated. Note: with Medicare deductibles Refer to the 835 Healthcare and/or coinsurance. Policy Identification Segment (loop 2110 Service Payment Information REF), if present. 686 Resubmit with an attached 251 The attachment/other CO Contractu N439 Missing anesthesia report documentation that was al anesthesia indicating/certifying the actual received was incomplete or Obligation physical status time spent with the patient. deficient. The necessary s report/indicators. information is still needed to process the claim. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT). N203 Missing/incomplete/ invalid anesthesia time/units. N463 Missing support data for claim. 687 “By Report” custom-made 252 An attachment/other CO Contractu N26 Missing itemized orthotic and prosthetic documentation is required to al bill/statement. appliances require a copy of the adjudicate this claim/service. At Obligation original invoice for the least one Remark Code must be s materials/parts used in provided (may be comprised of preparing the device, or the either the NCPDP Reject Reason manufacturer’s catalog page Code, or Remittance Advice Remark showing the suggested retail Code that is not an ALERT). price of the materials. M23 Missing invoice. N232 Incomplete/invalid itemized bill/statement. 688 Daily and monthly services are 97 The benefit for this service is CO Contractu M86 Service denied not separately reimbursed for included in the al because payment the same recipient and the payment/allowance for another Obligation already made for same calendar month. service/procedure that has s same/similar already been adjudicated. Note: procedure within Refer to the 835 Healthcare set time frame. Policy Identification Segment (loop 2110 Service Payment Information REF), if present.
1 – RAD to National Code Correlation: 600 – 699 September 2015 remit elect corr600 27
689 Check the CDP: EWC 251 The attachment/other N29 Missing Application for missing data documentation that was documentation/ (such as breast symptoms, received was incomplete or orders/notes/summ provider number, recipient deficient. The necessary ary/ name, recipient ID number). information is still needed to report/ chart. Check each claim line for an process the claim. At least one outcome code. Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT). N463 Missing support data for claim. 690 CCS Authorization invalid. 197 Precertification/authorization/notifica CO Contractu tion absent. al Obligation s
1 – RAD to National Code Correlation: 600 – 699 June 2010 remit elect corr600 28
RAD RAD Code Description HIPAA CARC Description HIPA CAGC HIPA RARC Description Cod CARC A Descripti A e CAGC on RARC 691 The diagnosis code is invalid for 16 Claim/service lacks information CO Contractu M76 Missing/incomplete/ the date of service. or has submission/billing error(s) al invalid diagnosis or which is needed for adjudication. Obligation condition. Do not use this code for claims s attachment(s)/other documentation. At least one Remark Code must be provided (may be comprised of either the NCPDP Reject Reason Code, or Remittance Advice Remark Code that is not an ALERT). Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. 692 Outpatient and emergency 96 Non-covered charge(s). At least CO Contractu M80 Not covered services during an inpatient one Remark Code must be al when performed stay are not separately provided (may be comprised of Obligation during the same reimbursable per facility either the NCPDP Reject Reason s session/date as a contract. [sic] Code, or Remittance Advice previously Remark Code that is not an processed service ALERT). Note: Refer to the 835 for the patient. Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. 693 Other coverage code is missing 16 Claim/service lacks information or CO Contractu MA04 Secondary payment or invalid. has submission/billing error(s) al cannot be which is needed for adjudication. Do Obligation considered without not use this code for claims s the identity of or attachment(s)/other payment documentation. At least one information from Remark Code must be provided (may the primary payer. be comprised of either the NCPDP The information Reject Reason Code, or Remittance was either not Advice Remark Code that is not an reported or was ALERT). Note: Refer to the 835 illegible. Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. N463 Missing support data for claim. N464 Incomplete/invalid support data for claim. 694 Only one Cancer Detection 119 Benefit maximum for this time CO Contractu M80 Not covered when Programs: Every Woman Counts period or occurrence has been al performed during case management code is reached. Obligation the same reimbursable per recipient, per s session/date as a recipient certification/ previously recertification period (one processed service year). for the patient. M86 Service denied because payment already made for same/similar procedure within set time frame.
1 – RAD to National Code Correlation: 600 – 699 ___ 2015 remit elect corr600 29
695 Ancillary charges are 97 The benefit for this service is CO Contract N19* Procedure code required for billing, but not included in the ual incidental to separately payable for payment/allowance for another Obligatio primary transitional care providers. service/procedure that has ns procedure. already been adjudicated. Note: Refer to the 835 Healthcare Policy Identification Segment (loop 2110 Service Payment Information REF), if present. 696 The Code I duration of B5 Coverage/program guidelines were CO Contractu N130 Consult plan drug/medical supply therapy not met or were exceeded. al benefit limitation has been exceeded. Obligation documents/guidel s ines for information about restrictions for this service.
1 – RAD to National Code Correlation: 600 – 699 September 2015 remit elect corr600 30
RAD RAD Code Description HIPAA CARC Description HIPA CAGC HIPA RARC Description Cod CARC A Descripti A e CAGC on RARC 697 The drug/medical supply 119 Benefit maximum for this time CO Contractu N362 The number of days dispensed has exceeded the period or occurrence has been al or units of service dispensing frequency limitation. reached. Obligation exceeds the s acceptable maximum. N435 Exceeds number/ frequency approved/ allowed within time period without support documentation. 698 The claim was sent to Fiscal 109 Claim not covered by this CO Contractu N193 Specific Intermediary in error. Submit payer/contractor. You must send the al Federal/state/loc the claim to the CCS (California claim to the correct Obligation al program may Children’s Services) office in the payer/contractor. s cover this service county where the recipient through another resides. payer. 699 This procedure is payable only 197 Precertification/authorization/notifica CO Contractu once in 140 days, and certain tion absent. al codes require a TAR if Obligation S3626/Z2503 has been paid in s 84 days.
1 – RAD to National Code Correlation: 600 – 699 September 2015