May 2015 Sm Animal Benchmark – Perioperative CC Case 1
A 5-year-old FS Staffordshire Terrier (35 kg) presents to the ER with acute tetraplegia, intact deep pain sensation and normal spinal reflexes. The dog is extremely tense on cervical palpation, but pain cannot be elicited. Mentation and cranial nerve exam are normal. The owners do not speak English and you are awaiting an interpreter to obtain a history.
Provide your neuroanatomical diagnosis.
List your top 3 differentials for this dog’s presenting neurologic signs.
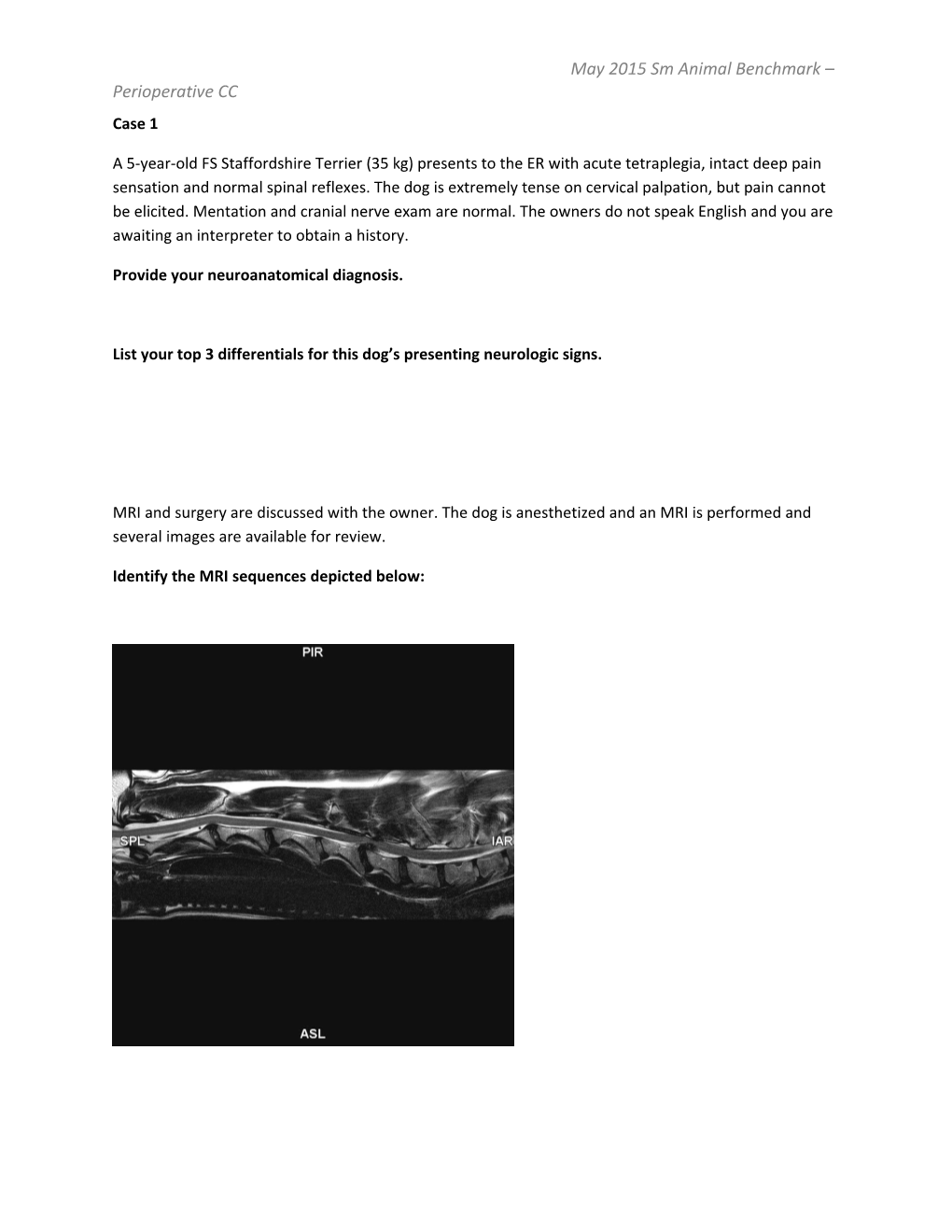
MRI and surgery are discussed with the owner. The dog is anesthetized and an MRI is performed and several images are available for review.
Identify the MRI sequences depicted below: May 2015 Sm Animal Benchmark – Perioperative CC
Please identify the following structures on the T2-weighted axial MRI image of the cervical spine depicted below:
Articular facet
Annulus fibrosis
Nucleus pulposus
Spinous process
Spinal cord
Subarachnoid space
Interarcuate ligament
Vertebral artery May 2015 Sm Animal Benchmark – Perioperative CC
What is your imaging diagnosis?
The dog is taken to surgery for a ventral slot decompression. The neurosurgeon reported excessive intraoperative hemorrhage and says that despite significant decompression, the cord could not be visualized (indicating the possibility of residual disc material.)
According to a recent review article of ventral slot decompression in a large cohort of dogs with cervical intervertebral disc disease, what is the approximate occurrence rate of perioperative adverse events (AE)? May 2015 Sm Animal Benchmark – Perioperative CC For the same group of dogs mentioned above, list 3 major AE and 5 risk factors associated with their occurrence.
One hour postoperatively, the dog remains intubated. You assess the patient as euhydrated and well- perfused, with a systolic BP of 140 mm Hg and a rectal temperature of 99F. PCV and total solids are 36% and 4.6 g/dL. Venous electrolytes are within normal limits.
The dog’s end tidal and arterial CO2 are 48 mm Hg and 55 mm Hg, respectively. Following drug reversal and patient repositioning, ventilatory drive appears adequate. The dog is extubated for several minutes, and then reintubated due to ineffectual chest excursions.
Arterial blood gas re-evaluation (the patient remains intubated and is spontaneously breathing with flow by oxygen) reveals the following:
pH: 7.11
PaO2: 95 mmHg
PaCO2: 80.0 mmHg - HCO3 : 23.5 mmHg BE: -2.4 mmol/L
What is the most likely cause of the severe and progressive respiratory acidosis in this dog? May 2015 Sm Animal Benchmark – Perioperative CC Due to the progressive respiratory acidosis, perceived poor thoracic wall excursions, and concern for impending ventilatory failure, the decision is made to place the dog on the mechanical ventilator.
You choose the mode of ventilation depicted below for this patient. Identify and characterize this mode of ventilation.
Provide 2 GENERAL advantages and 2 disadvantages associated with its selection of the mode of ventilation. May 2015 Sm Animal Benchmark – Perioperative CC You anticipate that long-term ventilator committee might be indicated for this dog.
List and briefly discuss 5 potential complications associated with prolonged anesthesia and immobility in human and/or veterinary patients and your interventions to minimize the occurrence of each.
Despite close proximity to the caudal cervical ventral slot surgical site, the decision is made on Day 2 of hospitalization to perform a temporary tracheostomy in this patient. This intervention is undertaken to facilitate patient wakefulness and interpretation of daily spontaneous breathing trials (SBT).
Describe this surgical procedure in detail. May 2015 Sm Animal Benchmark – Perioperative CC
List and provide evidence in the literature for one potential advantage associated with the use of the tracheostomy tube drawn above versus the “standard” tube type (standard depicted for comparison). May 2015 Sm Animal Benchmark – Perioperative CC
Outline your complete plan for maintenance of the tracheostomy tube.
On day 3, SBT reveals improved respiratory muscle strength. Mechanical ventilation is re- implemented with the incorporation of pressure support (PS). Describe this mode of ventilation in terms of trigger, limit and cycle. May 2015 Sm Animal Benchmark – Perioperative CC
List one advantage and one disadvantage associated with PS ventilation. May 2015 Sm Animal Benchmark – Perioperative CC
Case 2
A 7yr FN Doberman pinscher, weighing 40kg, presents with a 12 hour history of progressive abdominal distention and unproductive retching. Your physical exam findings include a heart rate (HR) of 160 beats per minutes, reduced pulse quality with an occasional irregularly irregular rhythm, and pale pink mucus membranes. Respiratory and neurological systems are normal; the dog does indeed have a distended and tense abdomen.
You suspect the dog has a gastric dilatation-volvulus (GDV). A peripheral IV catheter is placed and 20ml/kg of Plasma-lyte is administered, during which time a lateral abdominal radiograph confirms your diagnosis. The findings are discussed with the owner who agrees to surgery. The owner informs you the dog has been diagnosed with mild dilated cardiomyopathy (DCM) and is being treated with pimobendan and an angiotensin-converting enzyme inhibitor (ACEi).
Additional routine diagnostics included measurement of arterial blood pressure (BP) (100mmHg systolic) and venous blood lactate (9.3mmol/l), and obtainment of an ECG that shows a sinus tachycardia with occasional unifocal VPCs. Gastric decompression is performed by needle trocharization without incident. After a second 20 ml/kg bolus of isotonic crystalloids, the patient’s BP is 140 mm Hg and HR has decreased to 120 bpm.
Is this dog’s initial plasma lactate concentration of clinical significance? Defend your answer.
The criticalist working as your mentor is upset that therapy with lidocaine was not implemented prior to gastric needle decompression.
Justify or refute your mentor’s concerns based on recent veterinary literature. May 2015 Sm Animal Benchmark – Perioperative CC By what general mechanism/s is/are lidocaine postulated to have beneficial effects when administered early to dogs with GDV?
Complete the following table relating to the American Society of Anesthesiologists classification of physical status.
Category Physical Status Example of Category I
II
III
IV
V
What ASA category is this patient? May 2015 Sm Animal Benchmark – Perioperative CC
Following adequate resuscitation you elect to anesthetize the patient, starting first with administration of a premedication.
List the benefits of premedication in relation to anesthesia. What drug/drugs would you use in this patient for premedication, including dose? Justify your answer.
The patient has been on long term ACEi therapy. What effect may this therapy have on this dog’s ability to maintain GFR should she become hypotensive during the peri-operative period? Describe the mechanism.
Describe 2 methods of pre-oxygenating the patient, the benefits of pre-oxygenation and how long a patient should be pre-oxygenated.
For each of the following agents that can be used as part of an induction protocol, describe their mechanism of action, dose and effects of the cardiovascular system.
Propofol May 2015 Sm Animal Benchmark – Perioperative CC
Alphaxalone
Etomidate
Ketamine
Fentanyl
Midazolam May 2015 Sm Animal Benchmark – Perioperative CC
Describe what drug or drug combination you would use to induce this patient to minimize cardiovascular dysfunction associated with many anesthetic agents.
Define Total Intravenous Anesthesia (TIVA) and in basic terms describe the principle/s upon which this practice is based.
List 5 drugs that are recommended for use in TIVA (include in your response both initial IV loading dose and CRI dose).
Name three indications for the preferential use of TIVA over inhalant anesthesia. May 2015 Sm Animal Benchmark – Perioperative CC
There are many properties of inhalant anesthetics to consider in a critical patient. Define partition coefficient (PC) with regards to inhalant anesthetics.
Would you like a low or high blood:gas PC in this patient and explain why?
Given your response above, which inhalant anesthetic agent available in North America is most appropriate in this case?
The oil:gas PC is another important factor when choosing an agent for a particular patient.
List two patient populations for which particular consideration should be given to the different oil:gas PCs of various inhalant anesthetics and explain why this is.
Define MAC (minimum alveolar concentration). May 2015 Sm Animal Benchmark – Perioperative CC
Match the MAC % with the appropriate agent for dogs. Included are nitrous oxide, isoflurane, desflurane, methoxyflurane, halothane and sevoflurane. Which agent is most potent?
Agent MAC % 0.23 0.87 1.3 2.3 7.2 188
After surgery, the surgeon informs you that the dog required a splenectomy and partial gastrectomy, and was hypotensive several times while in the operating room.
The dog’s abdominal exploratory was otherwise unremarkable, and she is recovering well in the ICU. Plasma lactate is 1.8 mmol/L and venous blood gas and electrolytes are normal. Her heart rate is 120 bpm (normal sinus rhythm with occasional VPCS) and her systolic BP is 140 mm Hg.
Exclusive of plasma lactate, list 3 negative prognostic factors evident in this patient.
Case 3
Maddie, a 12 year old FS terrier mix, presents to your hospital for anxiety and trembling, and 24 hours of inappetance. On initial physical examination (PE) she is BAR and euhydrated, with moderate dental May 2015 Sm Animal Benchmark – Perioperative CC disease and a tense abdomen on palpation. Fundic examination is normal OU and there are no other significant abnormalities on PE.
Initial diagnostics include a CBC and biochemistry panel, which are within normal limits. A urinalysis reveals 2+ proteinuria with a USG of 1.036. Systolic blood pressure (BP) is 230 mmHg systolic with the patient in lateral recumbency and quiet (concurrent heart rate is 130 bpm).
You perform a FAST abdominal scan in the emergency room and think you see an abdominal mass. A CT scan with contrast of the chest and abdomen is performed to obtain more information about the tumor you visualized and acquire a more sensitive screen of the thoracic cavity for evidence of metastatic disease.
Interpret the abdominal CT images provided below: May 2015 Sm Animal Benchmark – Perioperative CC May 2015 Sm Animal Benchmark – Perioperative CC Pheochromocytoma (pheo) is at the top of your differential list. From what cell type does a pheo originate and what substance/s does this tumor secrete?
Implementation of what specific medication preoperatively may improve surgical outcome for this dog? Provide an evidence-based justification for your response (include drug mechanism of action, dose and regimen, and effect on mortality between treated and untreated dogs).
What are the postulated mechanisms via which the drug listed above reduces perioperative complications and mortality in both humans and dogs with pheochromocytomas?
In addition to preoperative administration of the drug discussed above, list 2 perioperative factors associated with improved 10-day survival in dogs with pheochromocytoma treated with surgery. May 2015 Sm Animal Benchmark – Perioperative CC Your supervising criticalist wishes to use prazocin in this dog perioperatively. What theoretical advantage/s might this drug have over the drug discussed above?
This dog is going to require a nephrectomy in addition to an adrenalectomy. Is this additional surgical procedure of any prognostic significance? Provide an evidence-based response.
List 5 negative pre- and/or intraoperative prognostic factors for dogs undergoing adrenalectomy for adrenal gland tumors that have been reported in the veterinary literature. May 2015 Sm Animal Benchmark – Perioperative CC Describe in general terms your anesthetic protocol for this dog. Include in your response any drugs that should be avoided in this case scenario.
After induction, you place an arterial catheter in the left dorsal pedal artery and recheck a blood pressure which is now 150 mmHg systolic, with a MAP of 100 mmHg. The HR is 300 bpm and the ECG (25 mm/s) shows this:
What is your diagnosis and recommended treatment (include drug dosages in your answer)? May 2015 Sm Animal Benchmark – Perioperative CC Your resident mate stops you before you administer a bolus of esmolol to this patient. He is concerned about administering a β blocker to a patient with a pheo who has not been treated first with an α- adrenergic receptor antagonist.
Justify the concern of your colleague.
What is your target blood pressure during anesthesia?
Your anesthetist informs you that the dog’s arterial blood pressure is 230 mmHg approximately 30 minutes into the surgery.
At what time in the perioperative period would you expect to deal with this complication and what is the likely mechanism causing hypertension in your patient?
How can you pharmacologically address this complication intraoperatively? List 3 appropriate agents (include drug mechanisms of action and doses in your answer)? May 2015 Sm Animal Benchmark – Perioperative CC
During surgical manipulation and removal of the tumor, the heart rate is now 190 bpm and the ECG shows this:
What is your diagnosis and how will you treat? Include drug class and dose in your answer. May 2015 Sm Animal Benchmark – Perioperative CC
During attempted excision of the tumor, hemorrhage from the vena cava occurs and the MAP drops to 40 mmHg. The dog’s PCV/TS drop from 48%/7.9 to 24%/4.0. The surgeon is currently achieving hemostasis.
How would you resuscitate this patient?
Post-operatively, hypotension recurs and persists despite volume-loading and treatment with exogenous catecholamines.
What is/are the most likely cause/s of this phenomenon and what treatment may be tried?
List 3 non-hemodynamic, postoperative complications in veterinary and/or human patients with pheochromocytoma. May 2015 Sm Animal Benchmark – Perioperative CC
Discuss hypocortisolism in patients with adrenal tumors of uncertain histologic type.
What is the prognosis after adrenalectomy in terms of short-term and long-term survival?
May 2015 Sm Animal Benchmark – Perioperative CC
Case 4
An 8-year old MC DSH presents to his primary veterinarian for a 36-hour history of anorexia and lethargy.
Two years prior to presentation, the cat had an acute episode of vomiting and was found to have hydronephrosis of the right kidney with normal complete blood count, serum chemistry, and urine specific gravity. Urine culture at that time was negative. No additional diagnostics or treatments were pursued for the hydronephrosis. Since that time, serial bloodwork was monitored, with the most recent being 2 months prior to presentation. His weight and body condition score were stable during this two year time period. His serum chemistry, complete blood count, and T4 at that time were within normal limits.
On examination, the cat is slightly quiet, well-perfused (Doppler systolic blood pressure is 140 mm Hg) and estimated as slightly dehydrated (5%). Temperature, heart rate, and respiratory rate are within normal limits, and heart and lung auscultation is normal. The cat is slightly uncomfortable on abdominal palpation; a 5 cm bladder is palpable.
Complete blood count, serum chemistry, venous blood gas, and urinalysis via cystocentesis are below. Aerobic urine culture is pending.
Total protein = 8.2 g/dL (5.2-8.8)
Albumin = 3.7 g/dL (2.5-3.9)
Globulin = 4.5 g/dL (2.3-5.3)
ALT = 102 U/L (10-100)
ALKP = 35 U/L (6-102)
BUN = 216 mg/dL (14-36)
Creatinine = 19.4 mg/dL (0.6-2.4)
Glucose = 86 mg/dL (64-170)
TCO2 = 14 mmol/L (16-25)
Na = 156 mmol/L (147-162)
K = 5.38 mmol/L (2.9-4.2)
Cl- = 120 mmol/L (112-129) iCa = 1.33 mmol/L (1.20-1.32) May 2015 Sm Animal Benchmark – Perioperative CC
pH = 7.206 (7.30-7.400)
PvCO2 = 26.2 mmHg (28.0-34.0)
HCO3- = 10.5 mmol/L (18-20)
BE = -15.3 mmol/L (-5 – 4)
WBC = 8.3 x103/L (3.5-16.0)
Neutrophils = 5727/L (2500-8500) (69%)
Bands = 0/L (0-150) (0%)
Lymphocytes = 1743L (1200-8000) (21%)
Monocytes = 83/L (0-600) (1%)
Eosinophils = 747/L (0-1000) (9%)
Basophils = 0/L (0-150) (0%)
RBC = 8.3 x106/L (5.92-9.93)
Hemoglobin = 13.5g/dL (9.3-15.9)
Hematocrit = 37 % (29-48)
MCV = 45 fL (37-61)
MCH = 16.3 pg (11-21)
MCHC = 36.5 g/dL (30-38)
Platelet count = 311 x103/L (200-500)
T4 = 1.6 ug/dL (0.8-4.0)
Urine appearance = cloudy (clear)
USG = 1.016 (1.015-1.060) pH = 6.0 (5.5 – 7.0) May 2015 Sm Animal Benchmark – Perioperative CC Protein = negative (negative)
Glucose = negative (negative)
Ketone = negative (negative)
Bilirubin = negative (negative)
Blood = 3+ (negative)
WBC = 0-1/HPF (0-3)
RBC = 11-20/HPF (0-3)
Casts = none seen
Crystals = none seen
Bacteria = none seen
Aerobic urine culture: pending
Abdominal ultrasound images and report are below: May 2015 Sm Animal Benchmark – Perioperative CC
Right kidney:
5.2cm long and distended with echogenic material. No normal parenchyma seen. The ureter is moderately distended (5mm) up to a 5.7mm shadowing structure in the mid portion of the ureter.
Left Kidney:
5.8cm long with diffusely mildly hyperechoic granular cortex and medulla, poor CM definition and a small cortical cyst. There is perirenal inflammation and small amount of effusion. The renal pelvis is 4.1mm dilated and the proximal ureter is 4.1mm dilated up to a narrowed area located approximately 3cm caudal to the kidney. The narrowed ureter has circumferential thickened wall and is approximately 1cm long. At the distal aspect of the abnormal narrowed ureter a faint curvilinear non-shadowing structure is present, presumably within the ureter. The ureter could not be followed distal to this area.
Urinary bladder:
Urinary bladder wall is normal. There is a small amount of sediment at the dependent portion
Conclusions:
- Right kidney- Severe echogenic hydronephrosis and proximal hydroureter likely secondary to the ureteric stone. The increased echogenicity of the right renal fluid can be due to pyonephrosis vs highly cellular fluid May 2015 Sm Animal Benchmark – Perioperative CC - Left renomegaly, pyelectasia, proximal ureteric dilation and thickened mid ureter causing luminal narrowing. Suspect the changes in the mid ureter are secondary to chronic ureteritis (infectious, inflammatory) with secondary stricture formation. The small hyperechoic structure caudal to the narrowed area can represent some sediment or a very small stone. The perirenal changes can be secondary to the chronic inflammation +/- acute nephritis/pyelonephritis. • Abdominal radiographs are obtained and reveal no presence of ureteral calculi not visualized via ultrasound.
What is your assessment of this cat’s history and the cause of azotemia?
Does this cat need hemodialysis? Justify your argument for or against hemodialysis at this time. May 2015 Sm Animal Benchmark – Perioperative CC Should antibiotic therapy be instituted pending the results of the urine culture? Justify your answer for or against antibiotics at this time.
In general terms, describe the management options for feline ureteral obstructions, including 2 pros and 2 cons for each option (not necessarily specific for this case). May 2015 Sm Animal Benchmark – Perioperative CC Should the ultrasound results have supported a concurrent diagnosis of a circumcaval ureter in this cat, would his expected outcome after management of his ureteral obstruction change?
Urine culture is negative for aerobic growth after 48 hours. Since the cat’s azotemia is persistent despite fluid therapy, the decision is made to pursue intervention to relieve the ureteral obstruction. A subcutaneous ureteral bypass (SUB) is placed in the left kidney due concerns for ureteral stricture as the source of the ureteral obstruction. The decision is also made to perform ureteronephrectomy on the right kidney due to concerns for it being a source of infection and having no viable parenchyma after being obstructed for at least 2 years. Histopathology of the right kidney shows marked dilation of the renal pelvis which is lined by hyperplastic transitional epithelium. No renal parenchyma remains and there is no evidence of neoplasia.
An E-tube and triple lumen jugular catheter are placed at the completion of surgery. Fluoroscopic images of the pyelogram consistent with ureteral stricture and implant upon surgical completion are below: May 2015 Sm Animal Benchmark – Perioperative CC
Label the parts of the SUB device in both images depicted below. May 2015 Sm Animal Benchmark – Perioperative CC May 2015 Sm Animal Benchmark – Perioperative CC
Post-operatively, the cat is managed on a fentanyl CRI (3-5 g/kg/hr) and crystalloids to match his urine production, which is on average, 8-10 ml/kg/hr. His creatinine decreases from 24.5 mg/dL pre-operatively to 3.4 mg/dL less than 24 hours after SUB placement. Water and food (1/3 RER) are introduced via the E-tube within 24 hours of surgery.
Forty-eight (48) hours post-operatively, the cat becomes acutely anuric. Despite treatment with furosemide and a fluid bolus, the cat remains anuric for 6 hours. Recheck creatinine increases to 6.8 mg/dL. Recheck fluoroscopy of the SUB using a diluted iodinated contrast agent (50:50 contrast:saline dilution) injected into the SUB port after aseptic preparation of the skin results in the following image: May 2015 Sm Animal Benchmark – Perioperative CC
What is the cause of the cat’s anuria and how must it be addressed?
What are long-term considerations for patients with SUB devices? May 2015 Sm Animal Benchmark – Perioperative CC List 3 reported predictors of decreased overall survival for cats following placement of ureteral stent or subcutaneous ureteral bypass device. May 2015 Sm Animal Benchmark – Perioperative CC Case 5
Dudley is a 12 year old, male/castrated Labrador Retriever who presented for polyuria and polydipsia (PU/PD) and weight loss. The owners report that his activity level may also be slightly decreased. Dudley has no prior medical or surgical history. He is current on vaccinations and not on any medications aside from monthly heartworm and flea prevention.
List 6 causes of PU/PD in small animal patients.
You elect to start the diagnostic work up with a CBC, Serum Biochemistry, and urinalysis. The results are reported below:
CBC
Variable Result Reference Range RBC 6.3 4.8 – 9.3 x 106/uL Hemoglobin 14.9 12.1 – 20.3 g/dl Hematocrit 43 36 – 60 % MCV 68 58 – 79 fl MCH 23.7 19 – 29 pg MCHC 34.7 30 – 38 g/dl Platelet Count 347 170 – 400 103/uL WBC 14.5 4.0 – 15.5 x 103/uL Differential Absolute Percentage Neutrophils 10,295 71 2,060 – 10,600/uL Bands 0 0 0 – 300/uL Lymphocytes 2030 14 690 – 4,500/uL Monocytes 870 6 0 – 840/uL Eosinophils 1305 9 0 – 1200/uL Basophils 0 0 0 – 150/uL
Serum Biochemistry May 2015 Sm Animal Benchmark – Perioperative CC Variable Result Reference Range ALT 322 12 – 118 U/L ALP 302 5 – 131 U/L T. Bili 0.2 0.1 – 0.3 mg/dL Total Protein 7.1 5.0 – 7.4 g/dL Albumin 3.6 2.7 – 4.4 g/dL Globulin 3.5 1.6 – 3.6 g/dL Glucose 85 70 – 138 mg/dL Calcium (total) 15.2 8.9 – 11.4 mg/dL Urea Nitrogen 13 6 – 31 mg/dL Creatinine 1.2 0.5 – 1.6 mg/dL Phosphorus 2.5 2.5 – 6.0 mg/dL Sodium 145 139 – 154 mEq/L Potassium 4.8 3.6 – 5.5 mEq/L Chloride 108 102 – 120 mEq/L Cholesterol 232 92 – 324 mg/dL Amylase 991 290 – 1,125 U/L
Urinalysis – Collected via cystocentesis
Variable Result Reference Range Color Yellow Appearance Cloudy Specific Gravity 1.012 1.015 – 1.015 pH 6.0 5.5 – 7.0 Protein 2+ Negative Glucose Negative Negative Ketone Negative Negative Bilirubin Negative Negative Blood 2+ Negative – 1+ WBC > 50 0 – 3/hpf RBC 4 – 10 0 – 3/hpf Casts None Crystals None Bacteria Cocci and Rods >100 None/hpf Transitional Epithelial Cells 0 – 1 0 – 1/hpf
Provide 10 differentials for hypercalcemia. Indicate which is the most common cause in dogs. May 2015 Sm Animal Benchmark – Perioperative CC
Based on the clinical presentation and laboratory results, you suspect primary hyperparathyroidism (PHPT) in this dog. What are the classic biochemical abnormalities for PHPT?
Provide a brief review of the roles of each of the following in calcium homeostasis.
Parathyroid Hormone:
Vitamin D Metabolites: May 2015 Sm Animal Benchmark – Perioperative CC
Calcitonin:
The most common clinical signs of PHPT-induced hypercalcemia involve which 3 organ systems? For each listed, provide a brief explanation for the signs observed.
List 6 treatment options available for acute medical management of hypercalcemia? Describe the mechanism/s by which these therapies reduce calcium concentrations. May 2015 Sm Animal Benchmark – Perioperative CC
What influence does the underlying cause have on your decision to treat acutely treat this patient’s hypercalcemia?
Based upon the results of the total calcium you elect to send off a parathyroid panel:
Variable Result Reference Range May 2015 Sm Animal Benchmark – Perioperative CC Parathyroid Hormone 17.50 0.5 – 5.80 pmol/L Ionized Calcium 2.07 1.25 – 1.45 mmol/L Parathormone Related Protein 0.0 0.0 – 1.0 pmol/L
Interpret the results of this panel.
True or false: In a patient with hypercalcemia, a serum PTH value which falls within the reported reference range makes a diagnosis of PHPT unlikely. Justify your response.
An ultrasound is done of the parathyroid glands. The radiologist finds a 1.9 cm x 0.99 cm nodule with a 1.4 cm x 0.5 cm cavitary central area in the region of the right caudal parathyroid gland – presumed to be cavitary neoplasia such as adenoma or adenocarcinoma, with parathyroid hyperplasia less likely. There is a 0.8 cm x 0.4 cm hypoechoic nodule in the region of the left caudal parathyroid gland – presumed parathyroid adenoma, with hyperplasia less likely. The right cranial parathyroid gland measures 0.27 cm x 0.16 cm and the left cranial parathyroid gland measures 0.16 cm x 0.13 cm.
In a veterinary study published within the last 3 years, what was the agreement between ultrasound and surgical findings regarding the laterality of parathyroid gland lesions in dogs with PHPT?
a. 100% b. 75% c. 50% d. 25%
What treatment options are available to treat canine PHPT? May 2015 Sm Animal Benchmark – Perioperative CC
List 2 complications associated with one or more of the treatment options listed above.
The owners elect to take Dudley to surgery. Preoperatively his total calcium concentration is 15.5 mg/dl.
Should medical therapy with vitamin D be provided to Dudley prior to surgery to reduce the risk of post-surgical hypocalcemia? Justify your answer based on available literature.
A chemiluminescent (CLA) PTH assay has been evaluated in PHPT dogs peri-operatively for rapid assessment (<20 minutes) of PTH concentrations.
What is the theorectical clinical utility of this test? May 2015 Sm Animal Benchmark – Perioperative CC
What are the reported incidences of hypocalcemia and clinical hypocalcemia, respectively, in dogs with PHPT postoperatively?
List 3 preoperative variables associated with low postoperative serum calcium nadir concentrations.
Dudley recovers from general anesthesia without complication.
What are your recommendations for post-operative care and monitoring?
Four days following surgery Dudley does not want to eat. He begins pawing at his face and has a slight increased effort to his breathing. You measure an ionized calcium and it is 0.97 mmol/L (Reference Range: 1.25 – 1.50 mmol/L).
How do you treat acute signs of tetany related to hypocalcemia? May 2015 Sm Animal Benchmark – Perioperative CC
Outline your long-term management strategy. Give doses where appropriate.