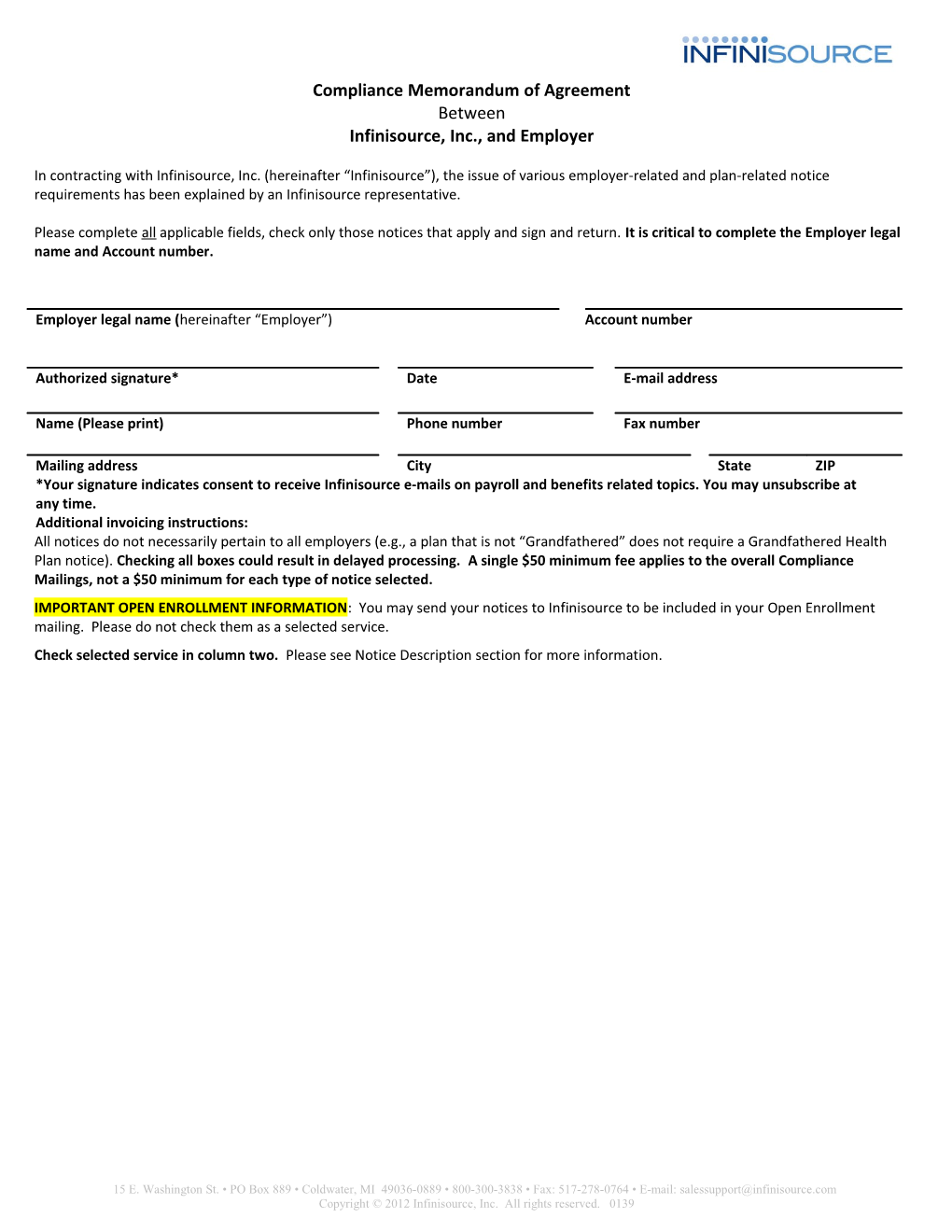
Compliance Memorandum of Agreement Between Infinisource, Inc., and Employer
In contracting with Infinisource, Inc. (hereinafter “Infinisource”), the issue of various employer-related and plan-related notice requirements has been explained by an Infinisource representative.
Please complete all applicable fields, check only those notices that apply and sign and return. It is critical to complete the Employer legal name and Account number.
Employer legal name (hereinafter “Employer”) Account number
Authorized signature* Date E-mail address
Name (Please print) Phone number Fax number
Mailing address City State ZIP *Your signature indicates consent to receive Infinisource e-mails on payroll and benefits related topics. You may unsubscribe at any time. Additional invoicing instructions: All notices do not necessarily pertain to all employers (e.g., a plan that is not “Grandfathered” does not require a Grandfathered Health Plan notice). Checking all boxes could result in delayed processing. A single $50 minimum fee applies to the overall Compliance Mailings, not a $50 minimum for each type of notice selected. IMPORTANT OPEN ENROLLMENT INFORMATION: You may send your notices to Infinisource to be included in your Open Enrollment mailing. Please do not check them as a selected service. Check selected service in column two. Please see Notice Description section for more information.
15 E. Washington St. • PO Box 889 • Coldwater, MI 49036-0889 • 800-300-3838 • Fax: 517-278-0764 • E-mail: [email protected] Copyright © 2012 Infinisource, Inc. All rights reserved. 0139 Administrative Service Law Required Recipients Timing Compliance Notices Fees, per notice type: 1 - $3.00; 2 - $3.75; 3 - $4.50; 4 or more - $5.25 (unless otherwise indicated) Affordable Care Act Notices Affordable Care Act 1. All participants and 1. Annually, with 1. Grandfathered Health Plan Notice (If (Public Laws 111-148 beneficiaries any plan selected, the Patient Protection Notice is & 111-152) 2. All participants materials not needed) 3. All individuals who 2. Whenever an SPD 2. Patient Protection Notice are eligible to be or similar benefits 3. Summary of Benefits & Coverage (mailing participants or description is only; client) beneficiaries provided 3. Annually at open enrollment and when SBC changes CHIP Notice (Children’s Health Insurance CHIPRA §311 All employees Annually before plan Program) year
COBRA General Notice 29 CFR §2590.606-1 All covered individuals Upon enrolling in Are you certified for Trade Adjustment plan and periodically Assistance by the Department of Labor? Yes No Do you offer an HMO plan? Yes No Do you have subaccounts with Infinisource? Yes No
FMLA General Notice 29 CFR §825.300(a) All employees On-site, in handbook or via other distribution HIPAA Special Enrollment Notice 26 USC §9801; 26 All eligible employees At enrollment CFR §54.9801-6(d) HIPAA Notice of Privacy Practices (NPP) 45 CFR §164.520 All covered Individuals Upon enrolling and upon request, material revision of notice HIPAA Notice of Availability of Notice of Privacy 45 CFR §164.520 All covered Individuals Every three years Practices Medicare Part D Notice of Creditable or 42 USC §1395w- All Medicare enrolled Annually by October Noncreditable Coverage 113(b)(6)(B) individuals with 15 Creditable Noncreditable Both prescription coverage (all covered employees Notice language English Combined highly recommended English/Spanish (If not indicated, notice will be because of unknown English) status of spouse/dependents) Summary Annual Report (SAR) 29 CFR §2520.104b- Within nine months Additional financial information from the 10 of the end of plan Employer’s completed Form 5500 will be needed year or two months to complete the SAR. after any extension period for filing the Form 5500 Women’s Health and Cancer Rights (WHCRA) All participants and Upon enrolling and 29 USC §1185b beneficiaries annually Please check here to indicate that you want Infinisource to complete the Data Sheet described in Section 1 based on information you provide. An additional fee of $1.50 per recipient is charged if Infinisource creates the Data Sheet. Notice of new COBRA administrator, $1.50 per letter, $25 minimum Possible Electee Letter, $1.50 per letter , $25 minimum Notice Inserts Upon request Additional information exceeding one (1) page, in one or more benefit related notice(s). $300 fee 15 E. Washington St. • PO Box 889 • Coldwater, MI 49036-0889 • 800-300-3838 • Fax: 517-278-0764 • E-mail: [email protected] Flexible Benefits Copyright © 2012 Infinisource, Inc. All rights reserved. 0139 Nondiscrimination Testing Internal Revenue Recommended twice Plan Documents and Summary Plan Annually Descriptions (SPDs) 1. IRC §105 & ERISA 1. Health Reimbursement Arrangements1 §104 2. Health Flexible Spending Accounts (FSAs) 1 2. IRC §105, 125, 129 & ERISA §104 3. Cafeteria Plans, Dependent Care FSAs1 3. IRC §132 4. 1 Qualified Transportation 4. 29 USC §§1022 & 5. 1102 ERISA Wrap Plan Document & SPD 1Plan design worksheet needed. $300-$1,000 fee based on customization Summary of Benefits & Coverage for HRAs Affordable Care Act All individuals who are Annually at open (creation & mailing, non-client) (Public Laws 111-148 eligible to be enrollment and $395 fee plus $3.00 per notice, $50 minimum & 111-152) participants or when SBC changes beneficiaries Open Enrollment (OE) $10 per packet or a $50 minimum. You may Treas. Reg. Annually send your notices to Infinisource to be included §54.4980B-5, Q/A- in your Open Enrollment mailing. Please do not 4(c) check them as a selected service. COBRA individuals: If you have sub-accounts with Infinisource you would like us to process OE for, please indicate those account numbers Annually here: Prop. Cafeteria Plan Reg. §1.125-2
Flexible Benefit participants: If you have sub- accounts with Infinisource you would like us to process OE for, please indicate those account numbers here:
*Cafeteria plan testing does not include the eligibility test or the contributions and benefits test **Dependent Care FSA testing does not include the eligibility test or the contributions and benefits test
Complete all information, save the document, print a copy and sign in the “Authorized Signature” area. Please fax this completed Memorandum of Agreement and all required documents to 517-278-0764, ATTN: Sales Support.
Please contact Infinisource at 800-300-3838 if you have questions.
Infinisource use only MOA valid for 30 days from Internal agent # Account # Service effective date
15 E. Washington St. • PO Box 889 • Coldwater, MI 49036-0889 • 800-300-3838 • Fax: 517-278-0764 • E-mail: [email protected] Copyright © 2012 Infinisource, Inc. All rights reserved. 0139 Employer agrees to the following:
1. Data To the extent necessary, Infinisource will provide Employer with a form (hereinafter “Data Sheet”) requesting data necessary to complete each administrative service. Infinisource is not required to provide administrative services if the data submitted is incomplete, inaccurate or untimely and is not liable for any adverse action based on tests conducted with incomplete, inaccurate or untimely data. Such data shall include but not be limited to: Legal name of group health plan (if uncertain, simply identify it as “Group Health Plan of [Employer Name]”) Contact information for the group health plan(s) (if uncertain, Infinisource will use any current information in our system) 2. Payment Infinisource will charge Employer, and Employer agrees to pay Infinisource, the fees for the services that are checked. Please note that special pricing may or may not apply to the mailing of the Summary of Benefits & Coverage, depending on the volume of the compliance mailing. Infinisource will notify Employer of the applicable pricing in advance if special pricing applies. Infinisource will charge Employer based on the number of individuals reported on the Data Sheet, including notices returned as undeliverable. Payment is due on receipt of the MOA, unless otherwise specified. All fees are nonrefundable once administrative services have been provided. 3. Notice Delivery Infinisource will send the notices via first class mail. Undelivered notices will be returned to Employer to be re-sent at its discretion with instructions on how to complete correctly. All documentation regarding the mailing will be returned to Employer for its records. 4. Possible Electee letter Infinisource can provide a letter to all COBRA individuals currently within their election periods and those that have recently elected. This letter alerts them to the change in administrators, and provides them with complete instructions on how to make their COBRA elections directly to Infinisource. The letter also explains our process after receipt of their COBRA election. Notice of New COBRA Administrator Infinisource can also provide a letter to individuals currently on COBRA regarding the transition to Infinisource. This letter explains there is a change occurring, and that they will receive detailed information once they are loaded into our system. Infinisource sends the notices via first class mail. Employer agrees to the following: a. Infinisource will send to Employer via e-mail a Microsoft Excel spreadsheet (Data Sheet) for providing the contact information of COBRA Electees and Possible Electees. b.Infinisource is authorized to send notices on behalf of Employer. Employer must send complete and accurate data via Infinisource’s Data Sheet. c. All Infinisource obligations under this MOA are conditioned on Employer complying with the requirements set forth in this MOA. Infinisource is not required to send notices if the data submitted is incomplete, inaccurate or untimely. d.In the event that Employer does not want to create and send the Data Sheet, Infinisource will complete the Data Sheet based on data provided by Employer or its designee, at an additional rate of $1.50 per recipient. This fee will be in addition to the fees for the Possible Electee/Electee Letter mailing. e. Undelivered notices will be returned to Employer to be re-sent at its discretion with instructions on how to complete correctly. All documentation regarding the mailing will be returned to Employer for its records. 5. Medicare Part D Notice Infinisource will provide other documents that answer key Employer questions. Please check the boxes whether the applicable plan(s) is (are) Creditable or Noncreditable (e.g., a creditable group health plan and a non-creditable health reimbursement arrangement). 6. Nondiscrimination Testing Infinisource will complete the tests and notify Employer if, based on Infinisource’s review of the results, any of the tests fail to pass. The results will be based on information received from Employer and/or any information obtained and maintained by Infinisource in the course of performing other services. Employer is solely responsible for any and all corrective action necessary based on a failed test. 7. Open Enrollment Infinisource will provide Open Enrollment notifications to current COBRA Qualified Beneficiaries, other COBRA participants, individuals who have elected but not yet paid for COBRA coverage and individuals currently within their election periods (collectively, “COBRA OE Individuals”). Employer must provide the following documents: a. Completed client questionnaire b. Audited Participant Status Report c. Current plan and rate information and, if applicable, any new plan(s) information d. All inserts that are to be included in the mailing, including benefits at a glance, enrollment forms, etc. (these documents can be e- mailed in a PDF format or mailed to us with a sufficient quantity of inserts for participants) After receiving accurate and complete information, Infinisource will: Prepare an Open Enrollment packet/notification to all COBRA OE individuals and send by first class mail Send an e-mail confirmation to Employer’s designated contact when the mailing has been completed Contact Employer for new address information in the event of returned packets (only if the COBRA OE Individual cannot be reached) 8. Plan Documents and SPDs Infinisource will prepare the text for the initial drafts of the required plan document(s) and SPDs (“Documents”) for the plans indicated above and pursuant to information provided by the Employer. Employer must have these drafts
15 E. Washington St. • PO Box 889 • Coldwater, MI 49036-0889 • 800-300-3838 • Fax: 517-278-0764 • E-mail: [email protected] Copyright © 2012 Infinisource, Inc. All rights reserved. 0139 reviewed by internal or external legal counsel to ensure that they conform with Employer’s business structure and requirements before they are officially adopted. Employer will ensure that the Documents are properly executed and delivered to plan participants as required by law. Thereafter, any amendments or changes to the documents based on new laws, regulations or plan designs are beyond the scope of this MOA and would require execution of a separate MOA for that purpose. Infinisource’s preparation of the documents will be managed, directed and reviewed by a licensed attorney with experience on flexible benefits. Such preparation does not include assistance with Form 5500 or any other required filings. These services are with the understanding that neither Infinisource nor any of its employees are engaged in rendering legal, accounting or other professional advice other than the preparation of the documents. 9. Confidentiality All information, whether printed, written or oral, in answer to an inquiry or voluntarily furnished by Employer or its agents or employees to Infinisource shall be held in confidence by Infinisource and used and disclosed solely for the purposes of fulfillment of the terms of this MOA. 10. Miscellaneous Items All Infinisource obligations under this MOA are conditioned on Employer complying with the requirements set forth above. Unless either party indicates otherwise, Infinisource will continue to provide the above selected services every year under the same terms and conditions. Infinisource will notify Employer of the need to provide new data at the appropriate time.
Compliance Notice descriptions Grandfathered Health Plan Notice Only Grandfathered health plans need to send this notice to participants that the plan or coverage is a Grandfathered health plan. This is an annual notice for every plan year in which a plan continues grandfathered status. Patient Protection Notice Non-Grandfathered plans must notify participants of their rights related to primary care physicians, OB/GYNs and pediatricians. This is an annual notice that only applies to non-grandfathered plans. Summary of Benefits & Coverage (SBC) This service only involves the distribution of the SBC to plan participants, including COBRA Qualified Beneficiaries. It does not entail creating, reviewing or editing a plan’s SBC. Fully-insured plans will receive their SBCs from insurance carriers. COBRA General Notice Informs plan participants of general COBRA rights. CHIP Notice Informs eligible employees of CHIP rights to premium assistance and special enrollment. FMLA General Notice Informs employees of FMLA Rights. HIPAA Special Enrollment Notice Informs plan participants of rights related to special enrollment and declination of coverage. HIPAA Notice of Privacy Practices (NPP) Informs plan participants about their HIPAA Privacy rights. HIPAA Notice of Availability of Notice of Privacy Practices Informs plan participants on how to obtain NPP. Medicare Part D Notice of Creditable or Noncreditable Coverage Informs plan participants whether group drug coverage is equivalent to Medicare Part D standard coverage. Notice of new COBRA administrator Infinisource can provide a letter to individuals currently on COBRA regarding the transition to Infinisource as if it is coming from the employer. Open Enrollment Infinisource will send a letter notifying the Qualified Beneficiaries that it is open enrollment time and lists updated plans and rates. Possible Electee Letter Infinisource can provide a letter to individuals currently within their election periods and those that have recently elected regarding the transition to Infinisource. Summary Annual Report (SAR) This report provides the needed data for the employer to be able file their Form 5500. Women’s Health and Cancer Rights (WHCRA) Notice Informs plan participants of the availability of required coverage under law.
Miscellaneous Benefit Activities and Required Documents Descriptions Notice Inserts Additional information exceeding one (1) page, in one or more benefit related notice(s). Nondiscrimination Testing (All Flexible Benefits) 1. Key employee concentration test (cafeteria plan) Highly compensated individual eligibility and benefits tests (Health FSA/HRA) 55% Average benefits test (Dependent Care FSA) 25% Shareholder concentration test (Dependent Care FSA) Nondiscrimination Testing (Cafeteria Plan Only) Key employee concentration test (Cafeteria Plan) Plan Documents and Summary Plan Descriptions (SPDs) This service provides the needed documents to an employer who wants to administer their own fringe benefits. Summary of Benefits & Coverage for HRAs (creation & mailing) This service includes creation and distribution of a customized HRA SBC, based on whether the HRA is stand-alone or integrated/bundled with a major medical plan, including a high deductible health plan.
This Memorandum of Agreement is hereby incorporated in any service agreement between the parties.
15 E. Washington St. • PO Box 889 • Coldwater, MI 49036-0889 • 800-300-3838 • Fax: 517-278-0764 • E-mail: [email protected] Copyright © 2012 Infinisource, Inc. All rights reserved. 0139 What Happens Next
Thank you for choosing to outsource your compliance notice administration to Infinisource, Inc. This checklist will help you submit a complete and accurate Memorandum of Agreement which expedites your service.
Your Account Setup Checklist:
Complete and sign the contact information. Check the services you are choosing to outsource. Send the completed MOA with payment to Infinisource, PO Box 889, Coldwater, MI 49036. Payment is due with agreement for Plan Documents and Discrimination Testing. We invoice for the Compliance Mailings and Open Enrollment processing.
An Infinisource Account Implementation Specialist will:
Send the appropriate Data Sheet to you (the client) for completion. After receipt of the completed Data Sheet, the appropriate document(s) will be processed and sent to you (the client) in three to five business days.
15 E. Washington St. • PO Box 889 • Coldwater, MI 49036-0889 • 800-300-3838 • Fax: 517-278-0764 • E-mail: [email protected] Copyright © 2012 Infinisource, Inc. All rights reserved. 0139