Anesthesia
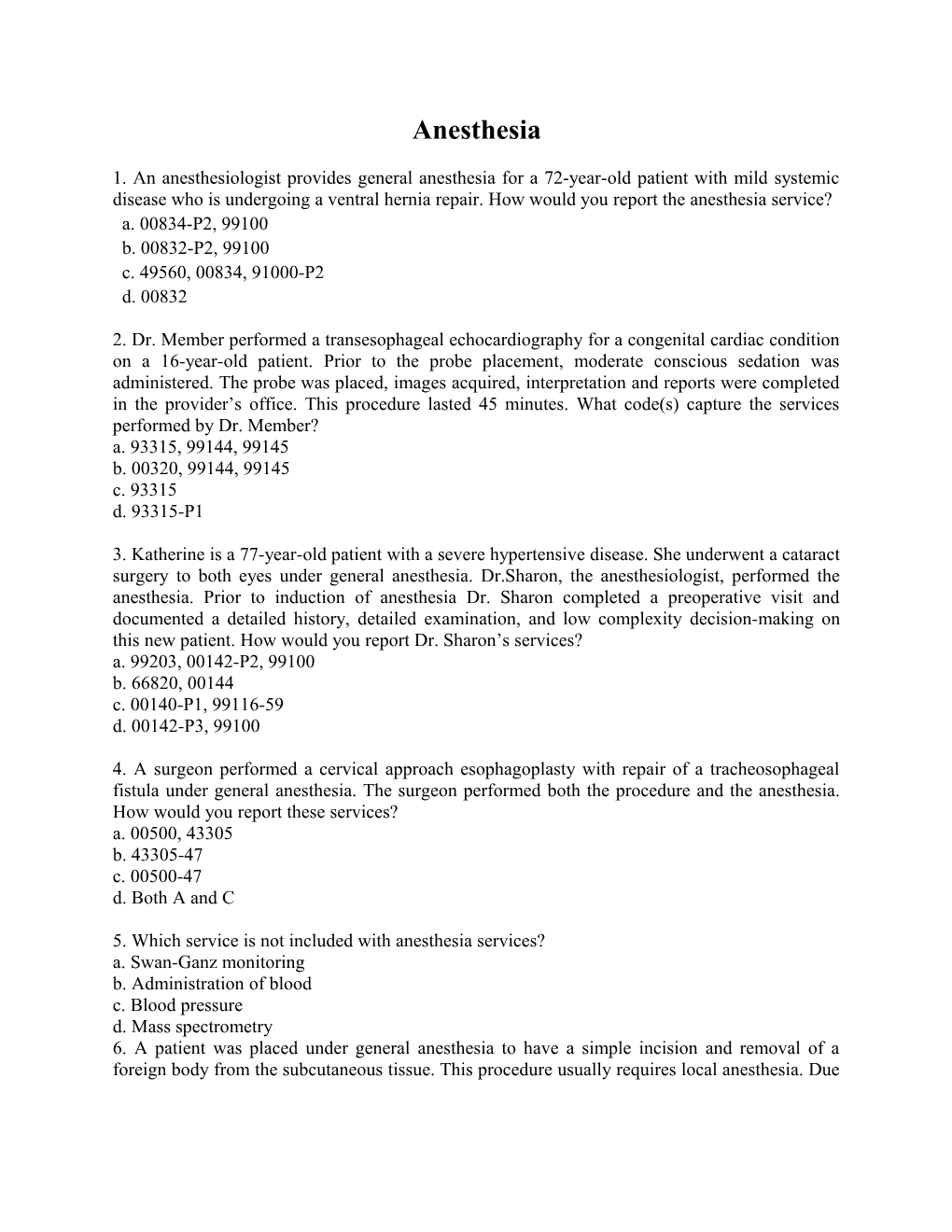
1. An anesthesiologist provides general anesthesia for a 72-year-old patient with mild systemic disease who is undergoing a ventral hernia repair. How would you report the anesthesia service? a. 00834-P2, 99100 b. 00832-P2, 99100 c. 49560, 00834, 91000-P2 d. 00832
2. Dr. Member performed a transesophageal echocardiography for a congenital cardiac condition on a 16-year-old patient. Prior to the probe placement, moderate conscious sedation was administered. The probe was placed, images acquired, interpretation and reports were completed in the provider’s office. This procedure lasted 45 minutes. What code(s) capture the services performed by Dr. Member? a. 93315, 99144, 99145 b. 00320, 99144, 99145 c. 93315 d. 93315-P1
3. Katherine is a 77-year-old patient with a severe hypertensive disease. She underwent a cataract surgery to both eyes under general anesthesia. Dr.Sharon, the anesthesiologist, performed the anesthesia. Prior to induction of anesthesia Dr. Sharon completed a preoperative visit and documented a detailed history, detailed examination, and low complexity decision-making on this new patient. How would you report Dr. Sharon’s services? a. 99203, 00142-P2, 99100 b. 66820, 00144 c. 00140-P1, 99116-59 d. 00142-P3, 99100
4. A surgeon performed a cervical approach esophagoplasty with repair of a tracheosophageal fistula under general anesthesia. The surgeon performed both the procedure and the anesthesia. How would you report these services? a. 00500, 43305 b. 43305-47 c. 00500-47 d. Both A and C
5. Which service is not included with anesthesia services? a. Swan-Ganz monitoring b. Administration of blood c. Blood pressure d. Mass spectrometry 6. A patient was placed under general anesthesia to have a simple incision and removal of a foreign body from the subcutaneous tissue. This procedure usually requires local anesthesia. Due to unusual circumstances, which required general anesthesia, what modifier would best describe this situation? a. 47 b. 22 c. 23 d. P6 7. A 42-year-old with renal pelvis cancer receives general anesthesia for a laparoscopic radical nephrectomy. The patient has controlled type II diabetes otherwise no other co-morbidities. What is the correct CPT® and ICD-9-CM code for the anesthesia services?
A. 00860-P1, 189.0, 250.00 B. 00840-P3, 189.1, 250.00 C. 00862-P2, 189.1, 250.00 D. 00868-P2, 198.0, 250.00
8. A healthy 32-year-old with a closed distal radius fracture received monitored anesthesia care for an ORIF of the distal radius. What is the code for the anesthesia service?
A. 01830-P1 B. 01860-QS-P1 C. 01830-QS-P1 D. 01860-QS- G9-P1
9. A 10-month-old child is taken to the operating room for removal of a laryngeal mass. What is the appropriate anesthesia code?
A. 00320 B. 00326 C. 00320, 99100 D. 00326, 99100 10. A 6-month-old patient is administered general anesthesia to repair a cleft palate. What anesthesia code(s) should be used for this procedure? A. 00170, 99100 B. 00172 C. 00172, 99100 D. 00176
11. A 50-year-old female had a left subcutaneous mastectomy for cancer. She now returns for reconstruction which is done with a single TRAM flap. Right mastopexy is done for asymmetry. Code the anesthesia for this procedure. A. 00404 B. 00402 C. 00406 D. 00400
12. A patient is having knee replacement surgery. The surgeon requests that in addition to the general anesthesia for the procedure that the anesthesiologist also insert a lumbar epidural for postoperative pain management. The anesthesiologist performs postoperative management for two postoperative days. A. 01400-AA, 62319 B. 01402-AA, 01996 x 2 C. 01402-AA, 62319, 01996 x 2 D. 01400-AA, 62319 13. A very large lipoma is removed from the chest measuring 8 sq cm and the defect is 12.2 cm requiring a layered closure with extensive undermining. MAC is performed by a medically directed Certified Registered Nurse Anesthetist (CRNA). Code the anesthesia service. A. 00400-QS-QX B. 00400-QS C. 00300-QS D. 00300-QS-QX
14.PREOPERATIVE DIAGNOSIS: Multivessel coronary artery disease. POSTOPERATIVE DIAGNOSIS: Multivessel coronary artery disease. NAME OF PROCEDURE: Coronary artery bypass graft x 3, left internal mammary artery to the LAD, saphenous vein graft to the obtuse marginal, saphenous vein graft to the diagonal. The patient is placed on heart and lung bypass during the procedure. Anesthesia time: 6:00 PM to 12:00 AM Surgical time: 6:15 PM to 11:30 PM What is the correct anesthesia code and anesthesia time? A. 00567, 6 hours B. 00566, 6 hours C. 00567, 5 hours and 30 minutes D. 00566, 5 hours and 30 minutes 15. A 56-year-old receives general anesthesia for an open pleura biopsy. An anesthesiologist medically directing two other cases, and medically directs a CRNA on this case. What are the appropriate codes for both providers? A. 00540-AA, 00540-QZ B. 00540-QK, 00540-QX C. 00541-AA, 00540-QZ D. 00541-QK, 00541-QX
16. The anesthesiologist performs an axillary block for postoperative pain management. The patient receives general anesthesia for a carpal tunnel release. What are the appropriate codes? A. 01810 B. 01810, 64417 C. 01810, 64417-59 D. 01830, 64417-59
17. A healthy 45-year-old is having a needle thyroid biopsy. The anesthesiologist begins to prepare the patient for surgery at 0900. The surgery begins at 0915 and ends at 0945. The anesthesiologist turns over the care of the patient to the recovery room nurse at 1000. What is the appropriate anesthesia code and what is the anesthesia time? A. 00320, one hour B. 00320, 45 minutes C. 00322, 45 minutes D. 00322, one hour 18. Patient is admitted in labor for delivery. She received a labor neuraxial epidural for a vaginal delivery. The baby goes into fetal distress and a cesarean section is performed. Following delivery the patient starts to hemorrhage. The physician decides, with family approval, to perform a hysterectomy. Code the anesthesia services. A. 01967, 00840 B. 01962 C. 01968 D. 01967, 01969 19. Angiograms reveal three artery blockages. The patient has COPD, which is a severe systemic disease. The patient undergoes a CABG X 3 venous grafts on cardiopulmonary bypass and cell saver. Code the anesthesia service. A. 00562-P3 B. 00560-P4 C. 00567-P3 D. 00566-P4 20. A healthy 11-month-old patient with bilateral cleft lip and palate undergoes surgery. The surgeon performs a bilateral cleft lip repair, single stage. Code the anesthesia service. A. 00170-P1, 99100 B. 00102-P1 C. 00102-P1, 99100 D. 00170-P1 21. The anesthesiologist performed MAC (monitored anesthesia care) for a patient undergoing an arthroscopy of the right knee. Code the anesthesia service. A. 01382-AA B. 01382-AA-QS C. 01400-AA D. 01400-AA-QS
22. General anesthesia is administered to a 9-month-old undergoing a tracheostomy. Code the anesthesia service. A. 00320, 99100 B. 00320 C. 00326 D. 00326, 99100 23. An anesthesiologist provided general anesthesia for open repair of a fractured pelvis column involving the acetabulum for a 74-year-old patient. Further documentation for this patient includes severe hypertension and uncontrolled diabetes. How should the anesthesiologist report her services? a. 01190-P3, 99100 b. 27226, 01190-P3, 99100 c. 01190-P4, 99100-51 d. 01170-P4 24. Dr. Burns, a surgeon, provided regional anesthesia and completed an exploration for postoperative hemorrhage in the neck on a 55-year-old patient with moderate cardiovascular disease. How would Dr. Burns report his services for this case? a. 00350-P2, 35800 b. 35800-47 c. 00350-P2 d. 00350-47 25. Why should the add-on code 99100 for qualifying circumstances not be reported with the following codes: 00326, 00561, 00834, and 00836? a. Age of the patient is not a factor with any anesthesia codes or add-on codes b. Age of the patient as older than 70 years is part of the code; therefore, it does not require the add-on code c. Age of child as older than 1 year is part of the code; therefore, it does not require the add-on code d. Age of child as younger than 1 year is part of the code; therefore, it does not require the add- on code 26. A patient undergoing a cervical surgery received general anesthesia for a procedure performed in a sitting position. The patient is 54 years old and healthy, aside from the current cervical problem. How should the anesthesiologist report his services? a. 00604 b. 00600-P1 c. 00604-P1 d. 00620 27. A patient underwent drainage of a pelvic abscess via transvaginal approach. The patient was under moderate sedation for the procedure, which was provided by the same operating physician. The intraservice time was clocked at 45 minutes. How should the sedation services be reported for this procedure? a. 58823, 00940 b. 00940-P2 c. 58823 d. 58823-P2 28. According to the anesthesia guidelines, what forms of monitoring are not included or bundled with anesthesia services? a. Intra-arterial b. Central venous c. Swan-Ganz d. All of the above. 29. Dr. Will, an anesthesiologist, provided three days of hospital management for epidural continuous drug administration. These services were performed after insertion of the epidural catheter. How should Dr. Will report these days of care? a. 01996-P1 x 3 b. 01996 c. 64999-P1 d. 64999 30. A patient with a third-degree burn of 54% of his body is being treated under anesthesia for excision, debridement, and extensive skin grafting. The patient’s condition is listed as severe, and he is not expected to survive without the operation. The operation is further complicated by the emergency condition of the patient, and delaying this procedure could lead to loss of body parts. How should the anesthesiologist report her services with this procedure? a. 01952-P5, 01953-P5 x 5, 99140 b. 01952-P5, 01953-P5 c. 01951, 01952, 01953 x 4 d. 01951, 01952, 01953 x 5, 99140-51 CPC Question 31. What add-on code should you report in addition to the code for the primary anesthesia procedure to describe anesthesia complicated by utilization of total body hypothermia? a.99100 b.99116 c.99135 d.99140
32. What code should you report for anesthesia for open procedures involving the hip joint; total hip arthroplasty? a01202 b01210 c01212 d01214 33. What physical status modifier should coders append to describe a patient with a severe systemic disease? a.P1 b.P2 c.P3 d.P4 34. What code should you report for anesthesia for all closed procedures on the radius, ulna, wrist, or hand bones? A 01820 b. 01829 c. 01830 d. 01832 35. What code should you report for anesthesia for all open procedures on upper ends of the tibia, fibula, and/or patella? a.01390 b.01392 c.01400 d. 01402 36. Which code should you report for evaluation and management of the critically ill or critically injured patient; first 30-74 minutes? a.99291 b.99292 c. 99293 d. 99294 37. Which code should you report for evaluation and management of the critically ill or critically injured patient, each additional 30 minutes of critical care? a. 99291 b. 99292 c. 99293 d. 99294 38 Which code(s) should you report for critical care, evaluation and management of the critically ill or critically injured patient, for 75 minutes of critical care time? a. 99291 x 1 b. 99291 x 1 and 99292 x 1 c. 99291 x 1 and 99292 x 2 d. 99291 x 1 and 99292 x 3
39. Which code should you report for initial inpatient neonatal critical care, per day, for the evaluation and management of a critically ill neonate, 28 days of age or less? a. 99293 b. 99294 c. 99295 d. 99296 40 Which code should you report for initial inpatient pediatric critical care, per day, for the evaluation and management of a critically ill infant or young child, 29 days through 24 months of age? a. 99292 b. 99293 c. 99294 d. 99295 41. When reporting for an anesthesia service using CPT codes (00100-01999), which service is not considered inherently included? a. Administration of blood b. Electrocardiogram c. Capnography d. Central venous catheter 42. An anesthesiologist administers general anesthetic to a patient undergoing an initial total hip arthroplasty. The patient is a healthy 71-year-old man. What are the correct CPT code(s)? a 27130-47, 99100 b 01214-P1, 99100-51 c 01214-P1, 99100 d 27130 43. A surgeon administers moderate sedation to a patient undergoing a diagnostic bronchoscopy in his office. The patient is a healthy 30-year-old woman and the intraservice time is 30 minutes. What are the correct CPT code(s)? a. 31622 b. 31622, 99144 c. 00520-P1 d. 00520-P1, 99100
44. A cardiologist performs a pacemaker insertion with transvenous electrodes into the patient's right atrium and ventricle in an ambulatory surgery center. The patient is a 50-year-old male with severe coronary artery disease. A different physician administers moderate sedation for this procedure. The intraservice time was 45 minutes. What are the correct CPT code(s) reported by the physician administering the anesthesia? a. 99149-P3, 99150-P3 b. 33208, 99149-P3, 99150-P3 c. Not separately reported d. 99149, 99150 45. A surgeon administers general anesthetic prior to performing a tympanostomy with a ventilation tube. The patient is an otherwise healthy nine-year-old boy with recurrent otitis media. What are the correct CPT code(s)? a. 69436-P1 b. 00126-P1 c. 69436-47 d. 00120-P1 46. Which of the following physical status modifiers would you report for a patient with severe systemic disease? a. P1 b. P2 c. P3 d. P4 47. If a provider administers anesthesia for procedures of the eye, specifically for a corneal transplant, which of the following anesthesia codes would you report? a. 00142 b. 00144 c. 00145 d. 00147
48. Code 00632 indicates that a provider administered anesthesia for which type of procedure in the lumbar region? a. Lumbar sympathectomy b. Chemonucleolysis c. Diagnostic or therapeutic lumbar puncture d. Not specified 49. Which of the following anesthesia codes is not related to the upper abdomen? a. 00730 b. 00752 c. 00790 d. 00802
50. If a patient receives anesthesia for a lower leg cast application, removal, or repair, which of the following anesthesia codes would you report? a. 01320 b. 01400 c. 01490 d. 01520
ANESTHESIA 1. “b” You should report the anesthesia services with modifier -P2 for mild systemic disease and qualifying circumstances due to the patient’s age.
2. “c” Refer to Appendix G in the CPT Professional Edition. This appendix lists the codes that include moderate conscious sedation along with guidelines to assist with reporting these services. Additionally, code 93315 has a “bulls-eye” symbol that indicates moderate conscious sedation is included with the service.
3. “d” According to the Anesthesia Guidelines in the CPT Professional Edition, the preoperative visit is “bundled” or included in the anesthesia services.
4. “b” According to the Anesthesia Guidelines in the CPT Professional Edition, “To report regional or general anesthesia provided by a physician also performing the services for which the anesthesia is being provided, see modifier -47 in Appendix A.” Appendix A describes the use of modifier -47 for a basic service when the anesthesia is provided by the surgeon.
5. “a” According to the Anesthesia Guidelines in the CPT Professional Edition, Swan-Ganz monitoring is not included.
6. “c” You can find the definition for Modifier -23 – Unusual Anesthesia in Appendix A of the CPT Professional Edition. 7. C The patient receives anesthesia for a laparoscopic radical nephrectomy. From the CPT® index, look up anesthesia/nephrectomy. You are referred to 00862. Review the code description to verify accuracy. The patient has controlled type II diabetes which supports the use of P2. The patient has renal pelvis cancer. The distinction of secondary cancer is not made so the cancer is coded as a primary neoplasm. In the neoplasm table go to the kidney/pelvis row and the primary column. You are referred to 189.1. The patient also has controlled type II diabetes. To locate, look up diabetes which refers you to 250.0x. A fifth digit is required. The scenario stated the patient is controlled with type II which is reported with a fifth digit of “0.”
8. C The patient receives monitored anesthesia care also known as MAC which is reported with HCPCS Level II modifier QS. There is no indication the patient has a history of cardiopulmonary condition so G9 would not be appropriate. From the CPT® index, look up anesthesia/forearm. You are referred to multiple codes (00400, 01810-01820, 01830-01860). Refer to these codes to determine the correct code using the code descriptions. The procedure was open and performed on the distal radius. The appropriate code is 01830.
9. B The patient receives general anesthesia for the removal of a laryngeal mass. From the CPT® index, look up anesthesia/larynx. You are referred to 00320 and 00326. Review the code descriptions. 00326 is the correct code to indicate the procedure is performed on a patient younger than one year. 99100 is not reported because the patient’s age range is included in the description of the anesthesia code. There is a parenthetical note following 00326 that states the code should not be reported with 99100. 10. C The patient receives general anesthesia for the repair of a cleft palate. From the CPT® index, look up anesthesia/cleft palate repair. You are referred to 00172. Verify the code description for accuracy. The patient is 6 months old, 99100 is appropriate for this scenario. 11. B The patient had a previous mastectomy. For this encounter the mastopexy and reconstruction is performed. From the CPT® index, look up anesthesia/breast. You are referred to 00402-00406. Refer to the code description for the correct code. 00402 is the correct code for anesthesia administered for breast reconstruction.
12. C A code is selected for the general anesthesia performed for the total knee replacement. From the CPT® index, look up anesthesia/replacement/knee. You are referred to 01402 which is the correct code. The lumbar epidural is also reported because the purpose is for postoperative pain. The procedure is reported with 62319. There is a parenthetical note following 62319 that indicates to use 01996 in conjunction with 62318-62319. 01996 is a per day code. In this scenario, the physician performs two days of daily management. Modifier AA indicates the anesthesia was performed by an anesthesiologist. 13. A MAC is performed for a procedure performed on the anterior trunk of the integumentary system. From the CPT® index, look up anesthesia/integumentary system/anterior trunk. You are referred to 00400 which is the correct code. The QS modifier is appended to identify that the type of anesthesia is MAC. The QX modifier is appended to report the service was provided by a medically directed CRNA.
14. A .The procedure performed is a coronary artery bypass. From the CPT® index, look up anesthesia/heart/coronary artery bypass grafting. You are referred to 00566 and 00567. The note indicates that the heart and lung bypass was used. Select 00567 because the code description includes “with pump oxygenator.” The anesthesia start time is 6:00 PM and the anesthesia ends at 12:00 AM which is six hours. 15. B. There is no indication that one lung ventilation is used. The correct anesthesia code for this procedure is 00540. The anesthesiologist reports the anesthesia with modifier QK to identify medical direction. The CRNA uses modifier QX to indicate it is a medically directed service.
16. C. The block is reported because it is done for postoperative pain management and not the mode of anesthesia. The block is reported with 64417. The procedure is reported with 64721, which crosswalks to 01810. In the CPT® manual look up anesthesia/wrist. The anesthesia is reported with 01810. Modifier 59 is appended because these services are bundled.
17. D. From the CPT® index, look up anesthesia/thyroid. You are referred to 00320-00322. The procedure performed is a thyroid needle biopsy, which is reported with 00322. Anesthesia time starts when the anesthesiology provider begins to prepare the patient and ends when they are no longer in personal attendance. In this case the anesthesia time starts at 0900 and ends at 1000 which is one hour. 18. D. The patient received a neuraxial epidural for labor for a planned vaginal delivery, which is reported with 01967. During the course of labor the patient requires a caesarean section. The patient begins to hemorrhage requiring a hysterectomy. The add-on code 01969 is used to report the anesthesia for the caesarean and hysterectomy.
19. C. From the index, look up anesthesia/ heart/ coronary artery bypass/grafting. You are referred to 00566 and 00567. In the scenario it states that cardiopulmonary bypass is used, which indicates that the code that includes pump oxygenator is the correct answer. The patient has COPD, which is a severe systemic disease, but there is no indication that is a threat to the patient’s life. Append physical status indicator P3.
20. C. Anesthesia is performed for cleft lip repair. From the index, look up anesthesia/cleft lip repair. You are referred to 00102. Refer to the code description to verify accuracy. The patient is healthy, which means P1 is the correct physical status modifier. 99100 is reported because the patient is under one year of age and the patient’s age is not included in the CPT® code for the anesthesia service 21. B. In this case MAC is performed, which requires modifier QS. This eliminates answer options A and C. The patient had a diagnostic arthroscopy. There is no indication that a surgical procedure was performed. Because the service was provided by an anesthesiologist, modifier AA is appended to the anesthesia code. 22. C. The patient receives anesthesia for a tracheostomy. From the CPT® index, look up anesthesia/trachea. You are referred to 00320, 00326, 00542. The patient is a 9-month-old which eliminates answer options A and B. There is a parenthetical note under code 00326 which states “Do not report 00326 in conjunction with 99100”. 23. a. One way to find this answer in the index of the CPT® Professional Edition is under the main term “Anesthesia,” “Pelvis,” then “Repair.” The guidelines for anesthesia indicate the use of physician status modifiers when reporting anesthesia codes. Additionally, the add-on code 99100 identifies the age of the patient in this question. 24. b. Review of modifier -47 in Appendix A of the CPT® Professional Edition provides instructions for placement of this modifier on the procedure code when the surgeon provides either general or regional anesthesia. 25. d. The anesthesia guidelines in the CPT® Professional Edition provide add-on codes for qualifying circumstances. The code 99100 is used to report the age of a patient as younger than 1 or older than 70 years. The parenthetical note following this add-on code provides the codes where age is a factor and already defined; therefore, the add-on code is unnecessary for correct reporting. 26. c. Anesthesia code 00604 describes the patient in a sitting position. Careful review of codes will help determine the correct reporting if there is an anatomical location and/or position included in the description. 27. c. Code 58823 includes moderate sedation. The add-on codes for qualifying circumstances and physical status modifiers are listed with anesthesia codes and should not be appended to a surgical procedure code. 28. d. The anesthesia guidelines in the CPT® Professional Edition provide a list of services that are included or bundled when provided. Additionally, the monitoring services that are not bundled are listed in the same guidelines. 29. a. This question specifies reporting for three days of hospital management. Code 01996 would be reported x 3 units. 30. a. The total body surface area (TBSA) burned is 54%. The first code, 01952, includes 9% of the burn; the add- on code 01953 would be reported for each additional 9% (five units equal 45% plus the initial 9% reaches the total 54%). ANESTHESIA
1. “b” You should report the anesthesia services with modifier -P2 for mild systemic disease and qualifying circumstances due to the patient’s age.
2. “c” Refer to Appendix G in the CPT Professional Edition. This appendix lists the codes that include moderate conscious sedation along with guidelines to assist with reporting these services. Additionally, code 93315 has a “bulls-eye” symbol that indicates moderate conscious sedation is included with the service.
3. “d” According to the Anesthesia Guidelines in the CPT Professional Edition, the preoperative visit is “bundled” or included in the anesthesia services.
4. “b” According to the Anesthesia Guidelines in the CPT Professional Edition, “To report regional or general anesthesia provided by a physician also performing the services for which the anesthesia is being provided, see modifier -47 in Appendix A.” Appendix A describes the use of modifier -47 for a basic service when the anesthesia is provided by the surgeon. 5. “a” According to the Anesthesia Guidelines in the CPT Professional Edition, Swan-Ganz monitoring is not included.
6. “c” You can find the definition for Modifier -23 – Unusual Anesthesia in Appendix A of the CPT Professional Edition. 7. C The patient receives anesthesia for a laparoscopic radical nephrectomy. From the CPT® index, look up anesthesia/nephrectomy. You are referred to 00862. Review the code description to verify accuracy. The patient has controlled type II diabetes which supports the use of P2. The patient has renal pelvis cancer. The distinction of secondary cancer is not made so the cancer is coded as a primary neoplasm. In the neoplasm table go to the kidney/pelvis row and the primary column. You are referred to 189.1. The patient also has controlled type II diabetes. To locate, look up diabetes which refers you to 250.0x. A fifth digit is required. The scenario stated the patient is controlled with type II which is reported with a fifth digit of “0.”
8. C The patient receives monitored anesthesia care also known as MAC which is reported with HCPCS Level II modifier QS. There is no indication the patient has a history of cardiopulmonary condition so G9 would not be appropriate. From the CPT® index, look up anesthesia/forearm. You are referred to multiple codes (00400, 01810-01820, 01830-01860). Refer to these codes to determine the correct code using the code descriptions. The procedure was open and performed on the distal radius. The appropriate code is 01830.
9. B The patient receives general anesthesia for the removal of a laryngeal mass. From the CPT® index, look up anesthesia/larynx. You are referred to 00320 and 00326. Review the code descriptions. 00326 is the correct code to indicate the procedure is performed on a patient younger than one year. 99100 is not reported because the patient’s age range is included in the description of the anesthesia code. There is a parenthetical note following 00326 that states the code should not be reported with 99100. 10. C The patient receives general anesthesia for the repair of a cleft palate. From the CPT® index, look up anesthesia/cleft palate repair. You are referred to 00172. Verify the code description for accuracy. The patient is 6 months old, 99100 is appropriate for this scenario.
11. B The patient had a previous mastectomy. For this encounter the mastopexy and reconstruction is performed. From the CPT® index, look up anesthesia/breast. You are referred to 00402-00406. Refer to the code description for the correct code. 00402 is the correct code for anesthesia administered for breast reconstruction.
12. C A code is selected for the general anesthesia performed for the total knee replacement. From the CPT® index, look up anesthesia/replacement/knee. You are referred to 01402 which is the correct code. The lumbar epidural is also reported because the purpose is for postoperative pain. The procedure is reported with 62319. There is a parenthetical note following 62319 that indicates to use 01996 in conjunction with 62318-62319. 01996 is a per day code. In this scenario, the physician performs two days of daily management. Modifier AA indicates the anesthesia was performed by an anesthesiologist. 13. A MAC is performed for a procedure performed on the anterior trunk of the integumentary system. From the CPT® index, look up anesthesia/integumentary system/anterior trunk. You are referred to 00400 which is the correct code. The QS modifier is appended to identify that the type of anesthesia is MAC. The QX modifier is appended to report the service was provided by a medically directed CRNA. 14. A .The procedure performed is a coronary artery bypass. From the CPT® index, look up anesthesia/heart/coronary artery bypass grafting. You are referred to 00566 and 00567. The note indicates that the heart and lung bypass was used. Select 00567 because the code description includes “with pump oxygenator.” The anesthesia start time is 6:00 PM and the anesthesia ends at 12:00 AM which is six hours. 15. B. There is no indication that one lung ventilation is used. The correct anesthesia code for this procedure is 00540. The anesthesiologist reports the anesthesia with modifier QK to identify medical direction. The CRNA uses modifier QX to indicate it is a medically directed service.
16. C. The block is reported because it is done for postoperative pain management and not the mode of anesthesia. The block is reported with 64417. The procedure is reported with 64721, which crosswalks to 01810. In the CPT® manual look up anesthesia/wrist. The anesthesia is reported with 01810. Modifier 59 is appended because these services are bundled.
17. D. From the CPT® index, look up anesthesia/thyroid. You are referred to 00320-00322. The procedure performed is a thyroid needle biopsy, which is reported with 00322. Anesthesia time starts when the anesthesiology provider begins to prepare the patient and ends when they are no longer in personal attendance. In this case the anesthesia time starts at 0900 and ends at 1000 which is one hour. 18. D. The patient received a neuraxial epidural for labor for a planned vaginal delivery, which is reported with 01967. During the course of labor the patient requires a caesarean section. The patient begins to hemorrhage requiring a hysterectomy. The add-on code 01969 is used to report the anesthesia for the caesarean and hysterectomy.
19. C. From the index, look up anesthesia/ heart/ coronary artery bypass/grafting. You are referred to 00566 and 00567. In the scenario it states that cardiopulmonary bypass is used, which indicates that the code that includes pump oxygenator is the correct answer. The patient has COPD, which is a severe systemic disease, but there is no indication that is a threat to the patient’s life. Append physical status indicator P3.
20. C. Anesthesia is performed for cleft lip repair. From the index, look up anesthesia/cleft lip repair. You are referred to 00102. Refer to the code description to verify accuracy. The patient is healthy, which means P1 is the correct physical status modifier. 99100 is reported because the patient is under one year of age and the patient’s age is not included in the CPT® code for the anesthesia service 21. B. In this case MAC is performed, which requires modifier QS. This eliminates answer options A and C. The patient had a diagnostic arthroscopy. There is no indication that a surgical procedure was performed. Because the service was provided by an anesthesiologist, modifier AA is appended to the anesthesia code. 22. C. The patient receives anesthesia for a tracheostomy. From the CPT® index, look up anesthesia/trachea. You are referred to 00320, 00326, 00542. The patient is a 9-month-old which eliminates answer options A and B. There is a parenthetical note under code 00326 which states “Do not report 00326 in conjunction with 99100”. 23. a. One way to find this answer in the index of the CPT® Professional Edition is under the main term “Anesthesia,” “Pelvis,” then “Repair.” The guidelines for anesthesia indicate the use of physician status modifiers when reporting anesthesia codes. Additionally, the add-on code 99100 identifies the age of the patient in this question. 24. b. Review of modifier -47 in Appendix A of the CPT® Professional Edition provides instructions for placement of this modifier on the procedure code when the surgeon provides either general or regional anesthesia. 25. d. The anesthesia guidelines in the CPT® Professional Edition provide add-on codes for qualifying circumstances. The code 99100 is used to report the age of a patient as younger than 1 or older than 70 years. The parenthetical note following this add-on code provides the codes where age is a factor and already defined; therefore, the add-on code is unnecessary for correct reporting. 26. c. Anesthesia code 00604 describes the patient in a sitting position. Careful review of codes will help determine the correct reporting if there is an anatomical location and/or position included in the description. 27. c. Code 58823 includes moderate sedation. The add-on codes for qualifying circumstances and physical status modifiers are listed with anesthesia codes and should not be appended to a surgical procedure code. 28. d. The anesthesia guidelines in the CPT® Professional Edition provide a list of services that are included or bundled when provided. Additionally, the monitoring services that are not bundled are listed in the same guidelines. 29. a. This question specifies reporting for three days of hospital management. Code 01996 would be reported x 3 units. 30. a. The total body surface area (TBSA) burned is 54%. The first code, 01952, includes 9% of the burn; the add- on code 01953 would be reported for each additional 9% (five units equal 45% plus the initial 9% reaches the total 54%).