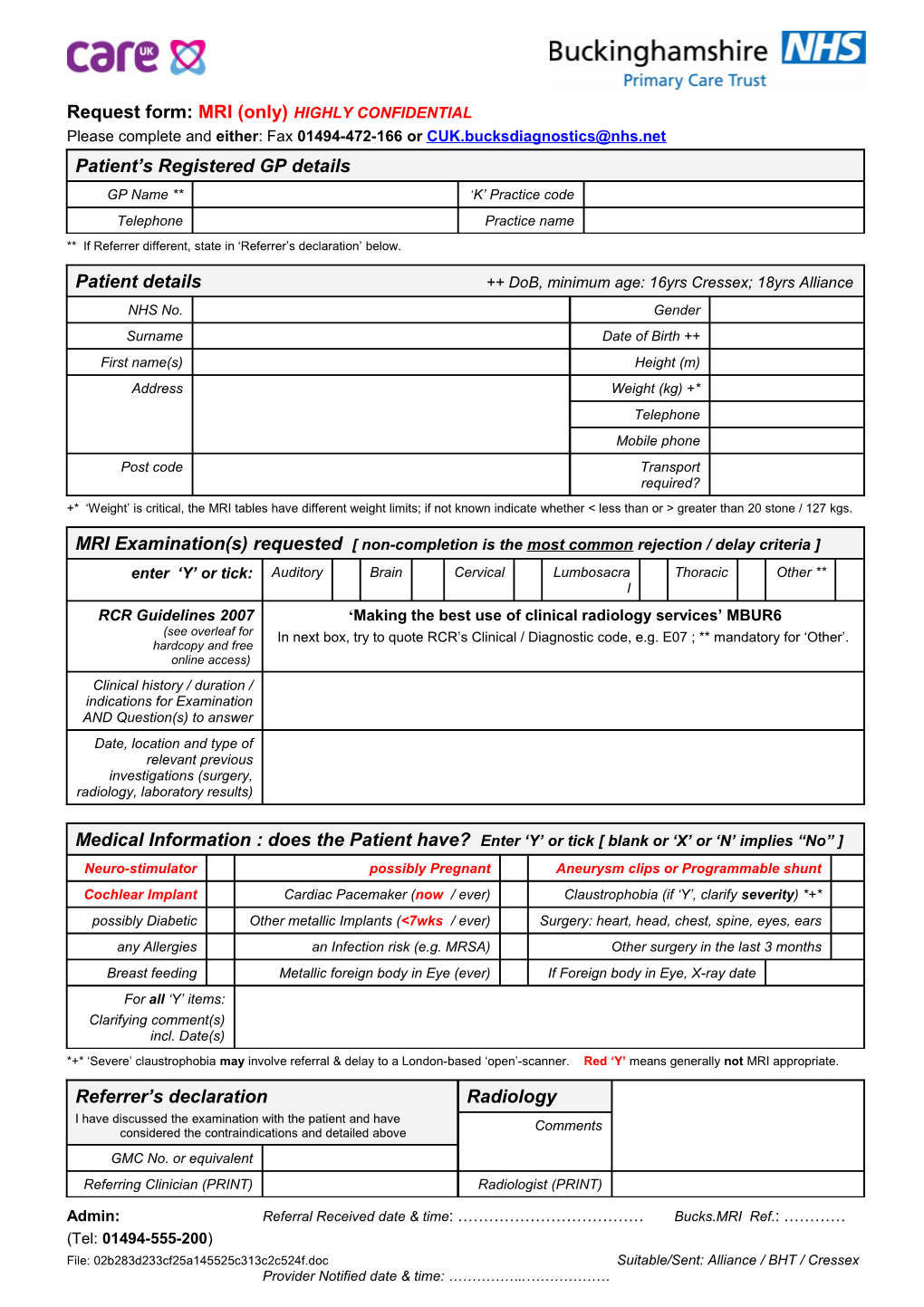
Request form: MRI (only) HIGHLY CONFIDENTIAL Please complete and either: Fax 01494-472-166 or [email protected] Patient’s Registered GP details GP Name ** ‘K’ Practice code Telephone Practice name ** If Referrer different, state in ‘Referrer’s declaration’ below.
Patient details ++ DoB, minimum age: 16yrs Cressex; 18yrs Alliance NHS No. Gender Surname Date of Birth ++ First name(s) Height (m) Address Weight (kg) +* Telephone Mobile phone Post code Transport required? +* ‘Weight’ is critical, the MRI tables have different weight limits; if not known indicate whether < less than or > greater than 20 stone / 127 kgs.
MRI Examination(s) requested [ non-completion is the most common rejection / delay criteria ] enter ‘Y’ or tick: Auditory Brain Cervical Lumbosacra Thoracic Other ** l RCR Guidelines 2007 ‘Making the best use of clinical radiology services’ MBUR6 (see overleaf for In next box, try to quote RCR’s Clinical / Diagnostic code, e.g. E07 ; ** mandatory for ‘Other’. hardcopy and free online access) Clinical history / duration / indications for Examination AND Question(s) to answer Date, location and type of relevant previous investigations (surgery, radiology, laboratory results)
Medical Information : does the Patient have? Enter ‘Y’ or tick [ blank or ‘X’ or ‘N’ implies “No” ] Neuro-stimulator possibly Pregnant Aneurysm clips or Programmable shunt Cochlear Implant Cardiac Pacemaker (now / ever) Claustrophobia (if ‘Y’, clarify severity) *+* possibly Diabetic Other metallic Implants (<7wks / ever) Surgery: heart, head, chest, spine, eyes, ears any Allergies an Infection risk (e.g. MRSA) Other surgery in the last 3 months Breast feeding Metallic foreign body in Eye (ever) If Foreign body in Eye, X-ray date For all ‘Y’ items: Clarifying comment(s) incl. Date(s) *+* ‘Severe’ claustrophobia may involve referral & delay to a London-based ‘open’-scanner. Red ‘Y’ means generally not MRI appropriate.
Referrer’s declaration Radiology I have discussed the examination with the patient and have Comments considered the contraindications and detailed above GMC No. or equivalent Referring Clinician (PRINT) Radiologist (PRINT)
Admin: Referral Received date & time: ……………………………… Bucks.MRI Ref.: ………… (Tel: 01494-555-200) File: 02b283d233cf25a145525c313c2c524f.doc Suitable/Sent: Alliance / BHT / Cressex Provider Notified date & time: ……………..……………… Referring Clinician Radiologist Signature Signature Date Date
Admin: Referral Received date & time: ……………………………… Bucks.MRI Ref.: ………… (Tel: 01494-555-200) File: 02b283d233cf25a145525c313c2c524f.doc Suitable/Sent: Alliance / BHT / Cressex Provider Notified date & time: ……………..……………… Bucks. health economy : ‘MRI Imaging Summary [not definitive OR complete]
Bucks. use The Royal College of Radiologists (RCR) guidelines ‘Making the best use of clinical radiology services’ 2007; hardcopy (£16 or less) and free NHS N3 online access http://www.rcr.ac.uk/content.aspx?PageID=995 . Guidance is not to use MRI imaging for all MSK Extremities, e.g. Ankle, Elbow, Foot, Hip, Knee, Shoulder – these are generally initially sent for X-ray, and/or referred to an MSK specialist to develop a Patient-specific pathway.
Complaint & Code Examples of Patient History / Symptoms Imaging Notes Cord damage / compression Head / neck MRI : Head Recent or complex injury Ligament injuries trauma T01 CT : Head Vertebral fractures ‘Red flags’ e.g.: Behavioural / Confusion Cognitive CT : identifies subarachnoid change : Memory loss haemorrhage CT : Head (normally 1st) Sudden / Drowsiness MRI : identifies inflammation MRI : Head ) Severe n Consciousness – loss of N/A for primary headache, i
a headache r Paralysis (partial, one side of body) e.g. tension, migraine B
( N05 Vision - blurred / loss K C
E Frequency / severity increase N
Recent start & >60years
& Triggers waking from sleep Chronic CT : Head D headache Previous tumour / disease
A Worse when cough, sneeze, strain MRI : Head E N06 N/A for primary headache, H Co-ordination loss, dizzy, tingling, e.g. tension, migraine numbness ENT specialist must evaluate Hearing / Sensorineural (90%) and Conductive MRI : IAM (Internal images & report; also do Loss E01/02 Auditory Meatus) Ave.23% occurrence in >65year olds Audiometry CT : Head URGENT TIA (Transient Ischemic Attack) Neurovascular must evaluate Stroke / TIA plus MRI if <30years [weakness in face OR arms & legs, within 7days of event N01/02 slurred speech : lasts few minutes, [may change as result of Consider Hospital / Clinic 24hrs no signs] new NICE guidelines]
Cervical Spine pain Surgery is appropriate; if (intractable) / Patient willing to Shows disc herniation Chronic (no improvement after 6 undergo surgery, then Brachialgia weeks of conservative therapy) Also refer to Orthopaedic MRI : Cervical or surgeon ) Sciatica c
i Lumbosacral
c M02/04 a r o h
T Acute (<12 wks) & ‘red flag’, e.g.:
, l
a Malignant infection / disease - known Definitive for spinal infection, r
c or signs e.g. TB (can lead to paralysis) a s MRI : Lumbosacral o Onset age <20 and >55 Evidence of cord compression b URGENT if previous – urgent referral to Oncologist m Raised plasma viscosity u Low-Back cancer history / Orthopaedic surgeon L
, pain Progressive & persistent l Intractable pain, refer to Pain a
c M05/06 Previous cancer i Service / Spinal surgeon v r HIV, drugs, steroids, etc. e C (
E Acute (<12 wks) no ‘red flag’ Post operation: advise N I features: MRI : shows disc
P Oncologist / Orthopaedic herniation S Post failed management / treatment surgeon
Thoracic (recent onset, persistent) spine pain Unresponsive to treatment MRI : Thoracic Additional markers may help M06/15 T13/14 Osteoporosis (collapse) suspected Knee Soft tissue masses – M10; Pain – M23/24; Fall/Blunt trauma – T21 X-Ray (MRI: ligaments / menisci)
File: 02b283d233cf25a145525c313c2c524f.doc