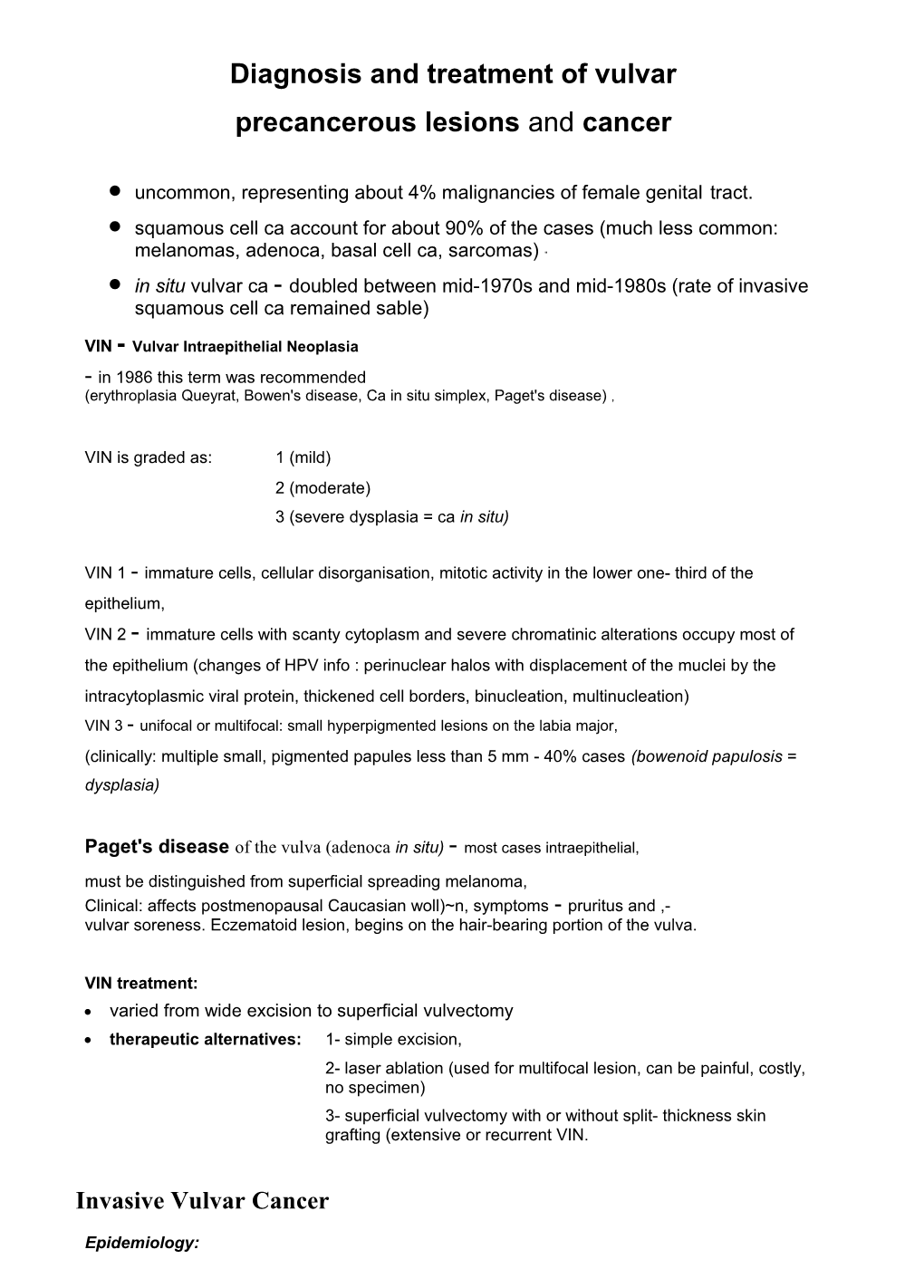
Diagnosis and treatment of vulvar precancerous lesions and cancer
uncommon, representing about 4% malignancies of female genital tract. squamous cell ca account for about 90% of the cases (much less common:
melanomas, adenoca, basal cell ca, sarcomas) " in situ vulvar ca - doubled between mid-1970s and mid-1980s (rate of invasive squamous cell ca remained sable)
VIN - Vulvar Intraepithelial Neoplasia - in 1986 this term was recommended (erythroplasia Queyrat, Bowen's disease, Ca in situ simplex, Paget's disease) ,
VIN is graded as: 1 (mild) 2 (moderate) 3 (severe dysplasia = ca in situ)
VIN 1 - immature cells, cellular disorganisation, mitotic activity in the lower one- third of the epithelium, VIN 2 - immature cells with scanty cytoplasm and severe chromatinic alterations occupy most of the epithelium (changes of HPV info : perinuclear halos with displacement of the muclei by the intracytoplasmic viral protein, thickened cell borders, binucleation, multinucleation) VIN 3 - unifocal or multifocal: small hyperpigmented lesions on the labia major, (clinically: multiple small, pigmented papules less than 5 mm - 40% cases (bowenoid papulosis = dysplasia)
Paget's disease of the vulva (adenoca in situ) - most cases intraepithelial, must be distinguished from superficial spreading melanoma, Clinical: affects postmenopausal Caucasian woll)~n, symptoms - pruritus and ,- vulvar soreness. Eczematoid lesion, begins on the hair-bearing portion of the vulva.
VIN treatment: varied from wide excision to superficial vulvectomy therapeutic alternatives: 1- simple excision, 2- laser ablation (used for multifocal lesion, can be painful, costly, no specimen) 3- superficial vulvectomy with or without split- thickness skin grafting (extensive or recurrent VIN.
Invasive Vulvar Cancer
Epidemiology: history of vulvar condylomata or granulomatous venera disease, v. ca ocassionally arise from areas of ca-in-situ, occur more frequently in women who have been treated for invasive squamous carcinomas of the cervix or vagina, more than half of the patients are between 60 and 79, fewer than 15% are under age of 40. obese, hypertensive, diabetic or nulliparous patients - more common
Etiology: HPV DNA has been reported in 20-60% of patients with invasive vulvar cancer (HPV- positive group: younger mean age, more tabacco use, presence of VIN associated with the invasive cpmponent).
Approximately 90-92% of all invasive vulvar cancers are of the squamous celr type.
Physical examination: the lesion is usually raised and may be fleshy, ulcerated, leukoplakic or warty (20%). Most squamous ca occur on the labia majora (labia minora, clitoris, perineum also may be primary sites). About 5% cases - multifocal, 10% too extensive to determine a site of origin.
Diagnosis: requires a wedge biopsy specimen, usually taken under local anesthesia. About 1 cm lesion - excisional biopsy is preferable.
Symptoms: a history of chronic vulvar irritation or soreness, a visible lesion on the labia, often sore.
Patterns of spread: 1- Local expansion (involves the contiguous structures of the urethra, vagina, perineum, anus, rectum, pubic bone. 2- Lymphatic spread: superficial inguinal nodes, deep femoral groups, pelvic nodes, 3- Hematogenous spred (advanced or recurrent cases).
Treatment:
Microinvasive ca (less than 1 cm, focal invasion no greater than 5 mm in depth, no Iymphovascular space involvement): wide (3 cm) local excision and sampling of the ipsilateral superficial inguinal nodes.
Invasive squamous ca: Stage I and II - radical vulvectomy, pelvic ratiotherapy is recommended for p. with involved nodes Stage III and IV - radical or exenterative surgery alone or in combination with radiotherapy. Five Year Survival rates: Stage 1- 71,4% Stage 2- 47,2% Stage 3- 32,0% Stage 4 - 10,5%.