Development of the GI system (both part I and part II)
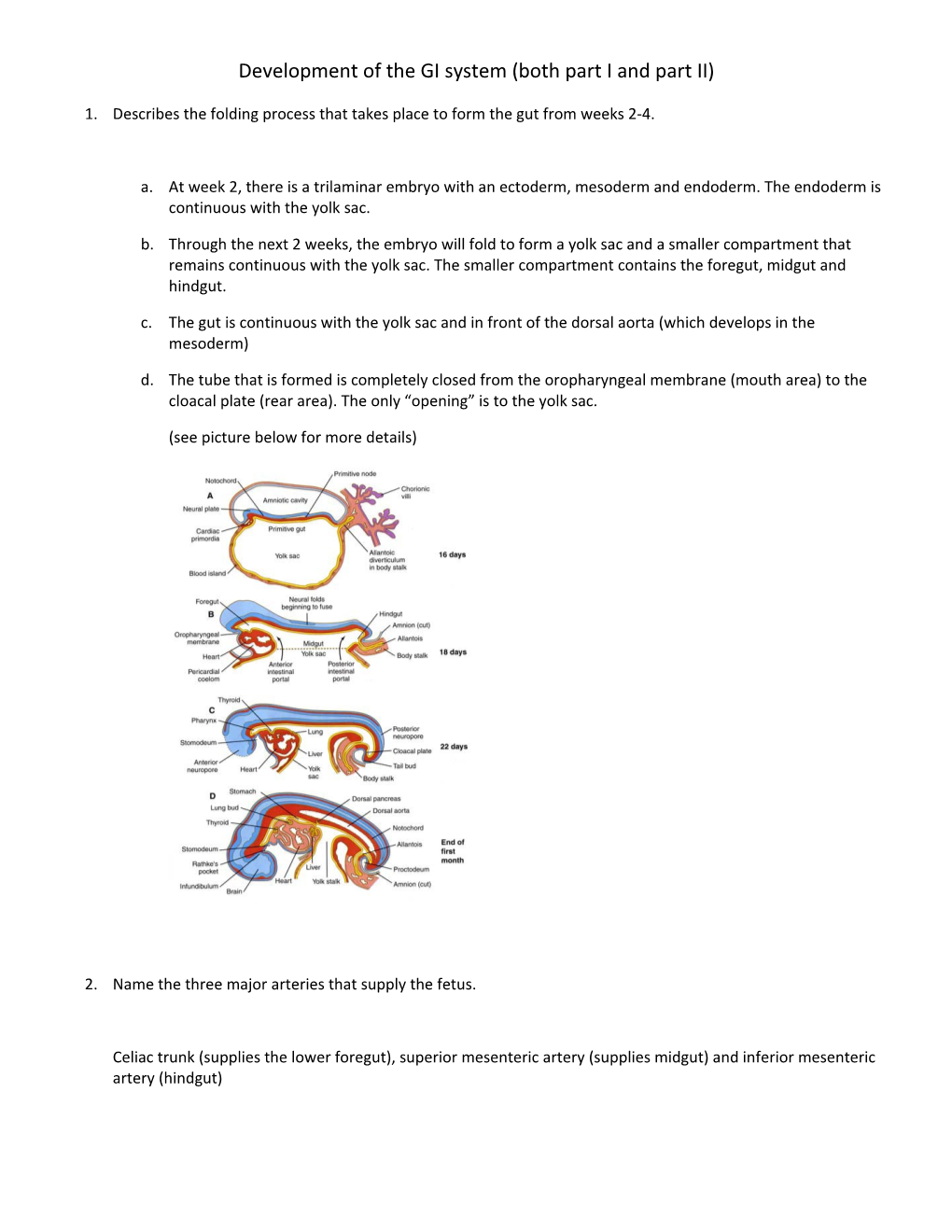
1. Describes the folding process that takes place to form the gut from weeks 2-4.
a. At week 2, there is a trilaminar embryo with an ectoderm, mesoderm and endoderm. The endoderm is continuous with the yolk sac.
b. Through the next 2 weeks, the embryo will fold to form a yolk sac and a smaller compartment that remains continuous with the yolk sac. The smaller compartment contains the foregut, midgut and hindgut.
c. The gut is continuous with the yolk sac and in front of the dorsal aorta (which develops in the mesoderm)
d. The tube that is formed is completely closed from the oropharyngeal membrane (mouth area) to the cloacal plate (rear area). The only “opening” is to the yolk sac.
(see picture below for more details)
2. Name the three major arteries that supply the fetus.
Celiac trunk (supplies the lower foregut), superior mesenteric artery (supplies midgut) and inferior mesenteric artery (hindgut) 3. What are the names of the membranes and 2 pits at either end of the embryo? What happens to them during development?
The 2 membranes are the oropharyngeal membrane (membrane at the mouth), the associated pit is the sternodeum. At the other end, the cloacal membrane closes off the gut and the proctodeum is the pit that forms. These membranes will rupture during the course of development. If this doesn’t occur then surgical treatment is needed.
4. Fill in the blanks Primordial Gut consists of a tube that is closed at the cranial and caudal ends Forms at week 4 due to folding of ______incorporating the yolk sac into the embryo. Lined primarily by ______which forms the ______Cranial end - ______lined by ______-closed by the ______Caudal end - ______lined by ______-closed by the ______Splanchnic mesenchyme surrounding the primordial gut forms the ______of the digestive tract.
Answers:
1. Folding of the head, tail and lateral walls
2. Endoderm
3. Epithelium/ lining of the digestive tract
4. Stomodeum
5. Ectoderm
6. Oropharyngeal membrane
7. Proctoderm
8. Ectoderm
9. Cloacal plate or membrane
10. Muscle and CT layers 5. How is the primitive gut divided? What do each of the divisions become?
a. The foregut is the first division, it becomes the esophagus, duodenum, liver and pancreas
b. The midgut is the second division, it becomes the distal half of the duodenum, jejunum, ileum, cecum, appendix, ascending colon and right 2/3 of transverse colon .
c. The hindugut is the last division, it becomes the left 1/3 of transverse colon, the descending colon, sigmoid colon, and rectum down to the pectinate line located in the anal canal.
6. Describe genetic controls in the primordial gut.
Hox genes expressed by the endoderm and splanchnic mesoderm regulate regional differentiation of the primordial gut.
7. Go through the organs, arteries, mesenteries and nerve supply of the foregut, midgut and hindgut.
8. Name and describe the 3 important time points in gut development
a. At the end of the first month- the primordial gut has formed
b. At the end of 3 months- the adult intestinal system has formed with the large intestine surrounding the small one. c. Late fetal period (before birth)- The digestive system is fully functional. Parietal cells have developed, smooth muscle of the digestive system is innervated.
9. Describe the mesentery of the digestive system.
The mesentery is a flexible conduit that provides the nerve fibers and blood vessels necessary to perfuse the organs of the digestive system. The mesentery is formed by a double layer of mesothelium that suspends the gut from the dorsal wall of the foregut to the hindgut. A layer of mesothelium lines the whole coelomic cavity that forms the parietal peritoneum and visceral peritoneum that lines the abdominal organs. The gut is almost entirely initially intraperitoneal. Over time, some parts of the mesentery will either expand (forming the omentum) or shrink to the abdominal wall, (forming secondarily retroperitoneal organs).
10. What is the importance of neural crest cells in GI system development?
Neural crest cells lead to the development of sympathetic and parasympathetic nerves.
11. Describe the parasympathetic innervations of the gut wall.
It is formed by Auberbach’s and Missern’s Plexuses present on the wall of the gut. It travels within the vagus nerve.
12. Describe the formation of the enteric nervous system.
It is formed from neural crest cells migrating to the Auerbach’s and Meissner’s plexi
13. Describe Hirschprung’s Disease.
This disease is called an aganglionic megacolon. It occurs when there is no innervation to part of the colon. Therefore, stool collects in this part and the colon becomes very large. Lack of innervations means the colon cannot continue to dry and move stool along. It normally occurs in the descending and sigmoid colons.
14. Describe the development of the esophagus. What is the derivation of the esophagus?
The esophagus starts as a hollow tube, then there is so much cell proliferation in the endoderm that occurs that the tube becomes completely occluded (filled in). Then, through the process of cell death, small canals form (recanulation). Finally, the tube completely hollows out and is wider than before. Problems that occur in this process are caused by lack of cell death. You can have stenosis or duplication. The skeletal muscle of the muscularis externa of the upper 1/3 of the esophagus is derived from the mesenchyme of the caudal pharyngeal arches. The smooth muscle of the lower 1/3 of the esophagus is derived from splanchnic mesenchyme.
15. Name the 4 developmental anomalies associated with esophageal development.
a. Esophageal atresia- a “blind end” in the esophagus
b. Polyhydraminos- Excess amniotic fluid in the fetus, develops because of lower atresia.
c. Esophageal stenosis- Narrowing of the lumen
d. Congenital short esophagus (aka a congenital hiatal hernia), occurs when esophagus is too short, so the stomach is pulled through the hiatus.
16. Describe the formation of the stomach and the lesser sac.
Stomach:
a. Stomach starts out as the primordial tube.
b. There is then differential growth, leading to the greater and lesser curvatures
c. At the same time, the stomach is going to rotate 90 degrees. This places the greater curvature on the left, the lesser curvature on the right. The previous dorsal surface of the stomach becomes the new right side and the previous ventral side of the stomach becomes the new left. This is the final resting point for the stomach. Note: only the “bottom” of the stomach rotates.
Formation of the lesser sac:
a. The dorsal mesogastrium (mesentery of the stomach) changes shape as the stomach itself rotates.
b. As the stomach rotates, the megogastrium enlarges and is pulled to the left, so that it grows both transversally and cranially, this places the lesser sac in between the stomach and the posterior abdominal wall.
c. As the stomach grows, the lesser sac expands in a superior/inferior direction
d. The dorsal mesogastrium itself will expand (along the greater curvature) to eventually form the greater omentum.
e. Many organs such as the pancreas and spleen grow into the dorsal mesogastrium.
17. Describe the formation of the duodenum. What are some issues with duodenal formation?
It is formed from the caudal end of the foregut and the cranial end of the midgut. The duodenum will form a C shape after the stomach rotates 90 degrees. The endoderm of the duodenum will grow so rapidly that it will occlude the canal, recanalization is needed to hollow out the cord. Issues: stenosis (narrowing), atresia (blockage, some part is missing) and polyhydraminos
18. Describe Liver formation
a. A diverticulum forms on the ventral surface of the caudal foregut called the hepatic diverticulum.
b. This diverticulum grows into the septum transversum, the reflections of the ventral mesentery on to the diaphragm become the coronary and triangular ligaments that surround the bare area of the liver
c. Proliferating endodermal cells form cords of hepatic cells around the endothelium lined spaces that are forming hepatic sinusoids. (the growing liver is composed of red mesoderm-becomes sinusoids and yellow endoderm-becomes hepatocytes)
d. Note: CT, endothelial cells, hematopoietic tissue and kupffer cells all arise from the splanchnic mesenchyme of the septum transversum
19. Describe gall bladder formation.
a. Form from the caudal part of hepatic diverticulum
b. The biliary apparatus is initially made from cords, but eventually form canals
c. The gall bladder moves from being attached to the ventral surface of the duodenal loop after the loop rotates.
20. Describe pancreatic formation, include duct information.
a. The pancreas arises from 2 evaginations called pancreatic buds. Most of the pancreas arises from the dorsal pancreatic bud, but the uncinate process (part that attaches to the head) arises from the ventral pancreatic bud.
b. The main pancreatic duct arises from BOTH the ventral pancreatic bud and most of the dorsal pancreatic bud. The accessory pancreatic bud, however, only arises from the dorsal pancreatic bud. This is the reason that the main pancreatic duct interacts with the common bile duct as it enters the duodenum.
c. Endodermal cells form both the exocrine and endocrine pancreatic tissues
d. Splanchnic mesenchyme forms the connective tissue elements of the pancreas.
21. Describe 2 pancreatic developmental abnormalities.
a. Accessory pancreatic tissue- when there is pancreatic tissue in another GI organ. It can cause the release of pancreatic enzymes which will create ulcers in different parts of the GI, because the pancreatic enzymes irritate the lumen of those organs.
b. Anular pancreas- If the dorsal and ventral pancreatic buds do not come together, 2 parts of the ventral pancreatic buds go around to meet and will constrict the duodenum. 22. How does the spleen develop?
The spleen develops spontaneously within the dorsal mesenchyme, unlike other GI tissues, there is no endodermal component to the spleen. The spleen ends up on the left after rotation.
23. Describe the development of the midgut into the intestines.
a. The midgut will form a loop within the abdominal cavity. There are 2 ends to this loop, the cranial end and the caudal end. The cranial end will become the distal duodenum, all of the jejunum and part of the ileum. The caudal end will become the distal ileum, all of the ascending colon and the proximal transverse colon. b. The apex of this loop is connected to the yolk stalk within the umbilical cord c. As the midgut continues to grow, it will grow larger than the existing abdominal cavity, so it herniates into the umbilical cord. d. As the herniation occurs, the loop will rotate 90 degrees so that the caudal portion is on the left and the cranial portion is on the right. e. The caudal portion will form a cecal bulge that will eventually lead to the formation of the cecum itself f. Finally, the abdominal cavity will grow large enough to incorporate the intestines again. g. As the intestines re-enter the body, they will rotate 180 degrees counterclockwise so that the cranial part will go to the left and the caudal loop goes to the right. The cranial limb retracts first because the cecal bulge on the caudal loop prevents the caudal loop from entering. Now, the cranial limb is on the left and the caudal limb is on the right. h. Initially, the cecum is placed by the liver. As the ascending colon elongates, the cecum descends down to the lower right quadrant. i. The yolk stalk should disappear and the ascending and descending colons will become secondarily retroperitoneal.
24. Describe the fixation of the intestines to the posterior abdominal wall.
Once the intestines are in place, the mesenteries of the ascending and descending colon, the pancreas and most of the duodenum (except for the first 2 cm) fuse with the posterior abdominal wall to become secondarily retroperitoneal. As these form, they will form the outlies for the paracolic gutters.
25. How do the cecum and appendix develop?
They develop from a bulge on the caudal limb of the intestinal loop. Differential growth of the caudal limb creates a cecal diverticulum. Then the appendix grows as a evagination of the cecum. All of this occurs at the same time as herniation and rotation. 26. Identify each of these midgut abnormalities
A- Nonrotation (minimal rotation) of the midgut- You have the initial 90 degree rotation, but not the secondary 180 degree rotation. It leads the the cecum on the left side and the small intestines on the right side.
B- Mixed rotation/volvulus- Faulty rotation causes misplacement of the cecum, placing the cecum inferior to the duodenum. The cecum normally forms a connective tissue layer to be fixed to the posterior abdominal wall, these bands of connective tissue extend from the cecum, along with intestinal twisting, lead to constriction of the duodenum.
C- Reverse rotation- the initial 90 degree rotation occurs clockwise instead of counterclockwise. Therefore, the duodenum and superior mesenteric artery end up anterior to the transverse colon. This means that the ascending colon is freely moveable (not fixed to posterior abdominal wall) and can constrict around the adjacent small intestine
D- Subhepatic cecum- occurs when the cecum stays near the liver, cecum does not migrate down to the lower right quadrant.
E- Internal hernia- part of the SI forms a pouch in the sigmoid colon, forming a hernia inside of the peritoneal cavity. The small intestine gets trapped in the sigmoid mesocolon, small intestine is surrounded by pocket of mesentery.
F- Midgut volvulus- The large intestine twists around, therefore the volvulus can obstruct the lulmen of the duodenum. This obstruction can also cause constriction of the blood supply to a specific area of the duodenum. 27. Name 4 problems that could occur because of the failure of the return of intestines to the abdominal cavity
a. Omphalocele- Failure of a portion of the intestine to return to the abdominal cavity, the herniated mass is surrounded by epithelium of the umbilical cord
b. Gastroschisis- Hernia of abdominal viscera through the wall of the abdomen, due to a defect in the closure of the lateral folds during week 4 when lateral walls are formed, the herniated viscera is not covered by anything.
c. Umbilical hernia- develops after successful return of the intestine to the abdominal cavity. It is due to a defect in the closure of the umbilicus, the herniated mass is surrounded by skin.
d. Internal hernia- caused by a loop of small intestine being stuck in the mesentery of the midgut loop. Can cause problems if that part of the small intestine is constricted and is not vascularized.
28. What is an ileal diverticulum? What is the main clinical problem that can result from it?
An ileal diverticulum results when part of the ileum is still connected to the umbilicus. The old connection that used to exist to the yolk sac is not obliterated. This connection can either be fibrous, form a cyst, or remain patent (a patent one means that food can leak out from the ileum to the skin). However, the biggest problem occurs when there is ectopic tissue located within this diverticulum. This can lead to ulcers (caused by release of hydrochloric acid or pancreatic enzymes) when pancreatic or gastric tissue is placed within the diverticulum.
29. Describe the types and how duplications occur in the small intestine.
There are 2 main types of duplications:
a. Cystic type- a cyst forms adjacent to the small intestine. This cyst does not communicate with the small intestine
b. Tubular type- a series of cysts that form a tube will form. This may or may not communicate with the lumen of the small intestine.
Duplications occur because of problems with recanalization. Normally after the vacuoles are formed, they will all come together to form one connected vacuole. However, if there is a problem a band of tissue persists between different vacuoles, causing problems.
30. What is the cloaca? Cloacal membrane? The cloaca is the endoderm lined chamber that at the caudal end of the fetus that is in contact with ectoderm at the cloacal membrane. The cloaca is continuous with the allantois and hindgut above it.
The cloacal membrane is the membrane that sits atop the cloaca. It is composed of ectoderm of the proctodeum and the endoderm of the cloaca. It develops in the angle in between allantois and hindgut.
31. Describe the partitioning of the cloaca into the rectum and urogenital sinus.
a. The Urorectal septum is mesenchyme that divides the cloaca into dorsal and ventral parts. As this septum develops, it will create an infolding of the cloaca.
b. Eventually these infoldings will fuse together and form 2 different parts, the urogenital sinus and the rectum. The point of attachment between these 2 things is called the perineum. The perineum acts as a point of attachment for many different muscles.
c. Finally, when the urorectal septum fuses with the cloacal membrane, it divides the membrane into a smaller anal membrane and a larger urogenital membrane. The urorectal septum has to contact the cloacal membrane at the correct spot.
d. The urorectal septum will divide the cloacal sphincter (muscles that develop around the cloaca)into an anterior and posterior part. The Anterior part becomes the muscles of the urogenital triangle and the posterior part becomes the external anal sphincter.
e. In the final step, the anal membrane ruptures, putting the distal digestive tract in contact with the amniotic cavity.
32. Describe the derivation of the anal canal. What is the pectinate line?
The upper 2/3rd is derived from the hindgut, while the bottm 1/3rd is derived from the ectoderm of the proctodeum. The pectinate line is a line on the inner surface of the anal canal. In the adult, this line represents the approximate location of the obliterated anal canal. The line represents the transition between parts derived from hindgut and parts derived from ectoderm of proctodeum.
33. What is the allantois? What does it ultimately become in the adult?
The allantois is continuous with the cloaca. It eventually becomes the urachus which will eventually become the median umbilical fold in the adult. 34. Identify each rectal abnormality.
A- The septum does not fuse with the cloacal membrane, this leads to a persistent cloaca and a common vaginal, rectal opening.
B- The septum has travelled too far, therefore the lumen is too narrow.
C- Anal membrane does not obliterate. Known as a persistent anal membrane, membranous anal atresia, imperforate anus
D- Anal agenesis with a perineal fistula- The rectum travels too far inferiorly, opens up at the perineum (around the area of the scrotum in the male) instead of at correct location.
E- Same as D in a female
F- Anal agenesis with a recttovaginal fistula. Rectum forms a fistula with the vagina
G- Anorectal agenesis with rectrourethral fistula. Rectum forms a fistula with the urethra because the rectum misses the anal pit
H- Rectal atresia. The anal canal is separated from the rectum. The rectum ends blindly.
I- Rectal atresia. The proximal and distal parts of the anus form, but the middle part is missing.