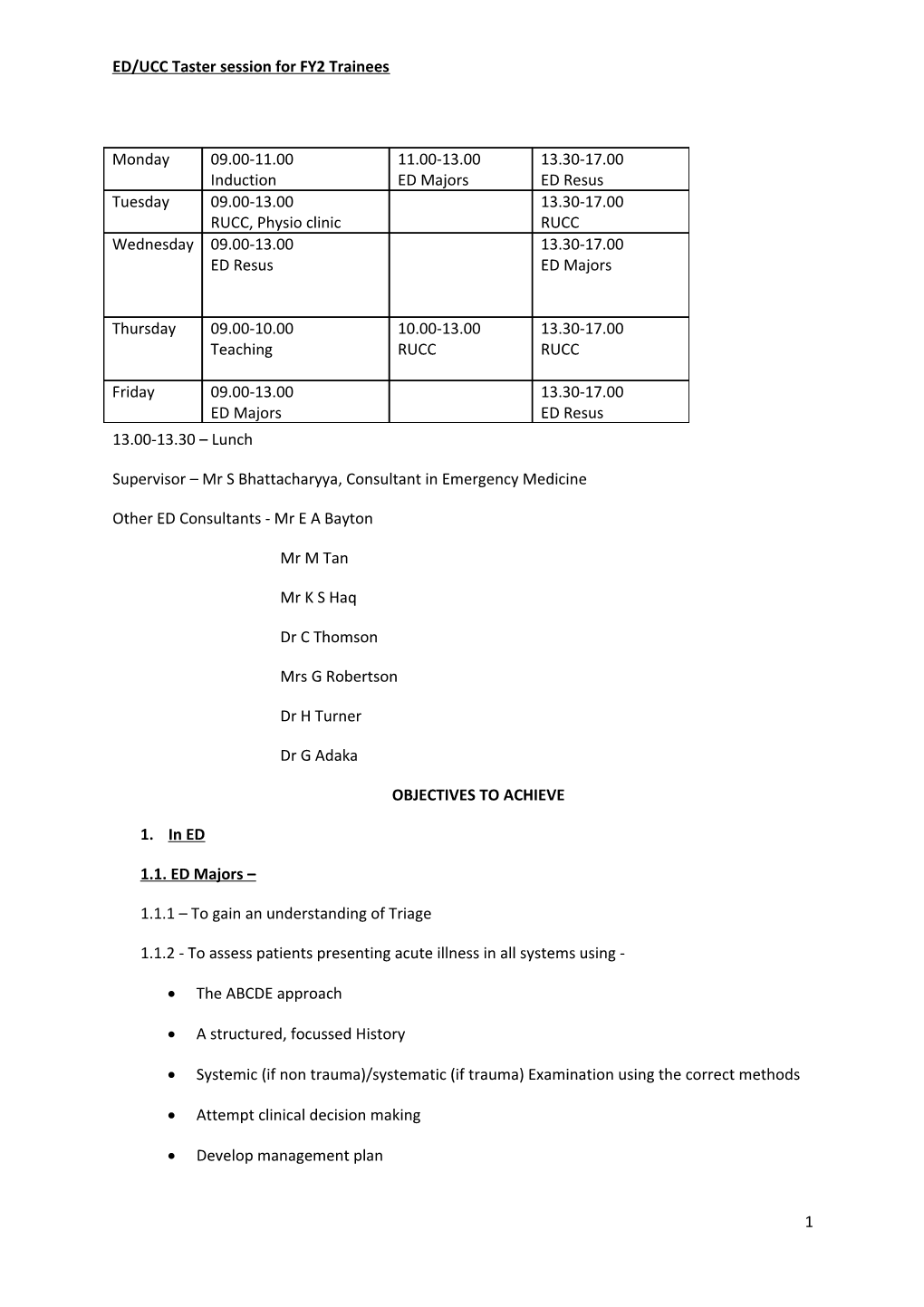
ED/UCC Taster session for FY2 Trainees
Monday 09.00-11.00 11.00-13.00 13.30-17.00 Induction ED Majors ED Resus Tuesday 09.00-13.00 13.30-17.00 RUCC, Physio clinic RUCC Wednesday 09.00-13.00 13.30-17.00 ED Resus ED Majors
Thursday 09.00-10.00 10.00-13.00 13.30-17.00 Teaching RUCC RUCC
Friday 09.00-13.00 13.30-17.00 ED Majors ED Resus 13.00-13.30 – Lunch
Supervisor – Mr S Bhattacharyya, Consultant in Emergency Medicine
Other ED Consultants - Mr E A Bayton
Mr M Tan
Mr K S Haq
Dr C Thomson
Mrs G Robertson
Dr H Turner
Dr G Adaka
OBJECTIVES TO ACHIEVE
1. In ED
1.1. ED Majors –
1.1.1 – To gain an understanding of Triage
1.1.2 - To assess patients presenting acute illness in all systems using -
The ABCDE approach
A structured, focussed History
Systemic (if non trauma)/systematic (if trauma) Examination using the correct methods
Attempt clinical decision making
Develop management plan
1 ED/UCC Taster session for FY2 Trainees
Administer essential treatment including drugs
1.2. In the ED Resuscitation –
1.2.1 – To consolidate ABCDE assessment system
1.2.2 – To assess and manage under supervision –
Cardiac arrest in adults and children
Major trauma
Severe sepsis
COPD exacerbation with respiratory failure needing BIPAP
Shocked patient
Severe Head Injury
Peri arrest Arrhythmia
2. In RBH UCC –
2.1 – To assess minor injuries and illness using the Look, Feel, Move technique
2.2 – To decide the need for X-ray request in injury
2.3 – To interpret X-ray under supervision
2.4 – To devise a management plan
2.5 – To see patients with the following emergencies –
Eye
ENT
Maxillo-facial
3. Generic skills – To consolidate the following -
Communication
Consent
Documentation
Referral to specialty(orthopaedics, paediatrics) and handover using SBAR
2 ED/UCC Taster session for FY2 Trainees
Referral to agencies ie – OT, Physio, Alcohol team, Age UK, RAT, Neurosurgeons at RPH
4. Procedural skills – To perform under supervision (US) & independently (IP) and to get SLE’s done in –
IV access - IP
Venepuncture - IP
Blood culture - IP
Blood tests incl. interpretation and action if abnormal - IP
ABG incl. interpretation and action if abnormal - IP
ECG interpretation - US
Fascia Iliac Compartment Block (FICB) for # NOF patient – US
Femoral nerve block for femoral shaft # patients – US
Digital nerve block – US
Chest drain – US
CPR – IP
Defibrillation – US
Wound assessment, management including closure techniques - US
Log roll a patient with spinal injury - US
C-spine immobilisation – US
Airway management using basic manoeuvres & adjuncts
MUA of simple colles # in the elderly, Dislocation of Shoulder & Elbow, #-dislocation of ankle
5. To try and obtain exposure to and manage the following –
Patients with Chest pain with diagnosis of – STEMI, NSTEMI, Unstable angina,
Patients with Breathlessness with diagnosis of - Acute Asthma, COPD exacerbation, Pneumonia, ?PE
Patients in Shock with diagnosis of - Haemorrhagic, anaphylactic, Septic, Hypovolemic, Cardiogenic
Patients with Abdominal pain with diagnosis of – Acute Cholecystitis, Acute pancreatitis, Acute Appendicitis, Acute Intestinal Obstruction,
3 ED/UCC Taster session for FY2 Trainees
Patients with Bleeding PV in early pregnancy
Patients with Upper and Lower GI Haemorrhage
Patients with Neurological emergencies with diagnosis of – Stroke, TIA, Cauda-Equina syndrome
Patients with Collapse in the elderly
Patients with DKA
Patients with diagnosis of - #NOF
To use care Bundles like – Sepsis, #NOF, Stroke, pneumonia, COPD, DKA
To use NICE guidelines (CT scan in head Injury, COPD, GI Haemorrhage, DVT, PE), BTS guidelines(Asthma, Pneumonia)
4