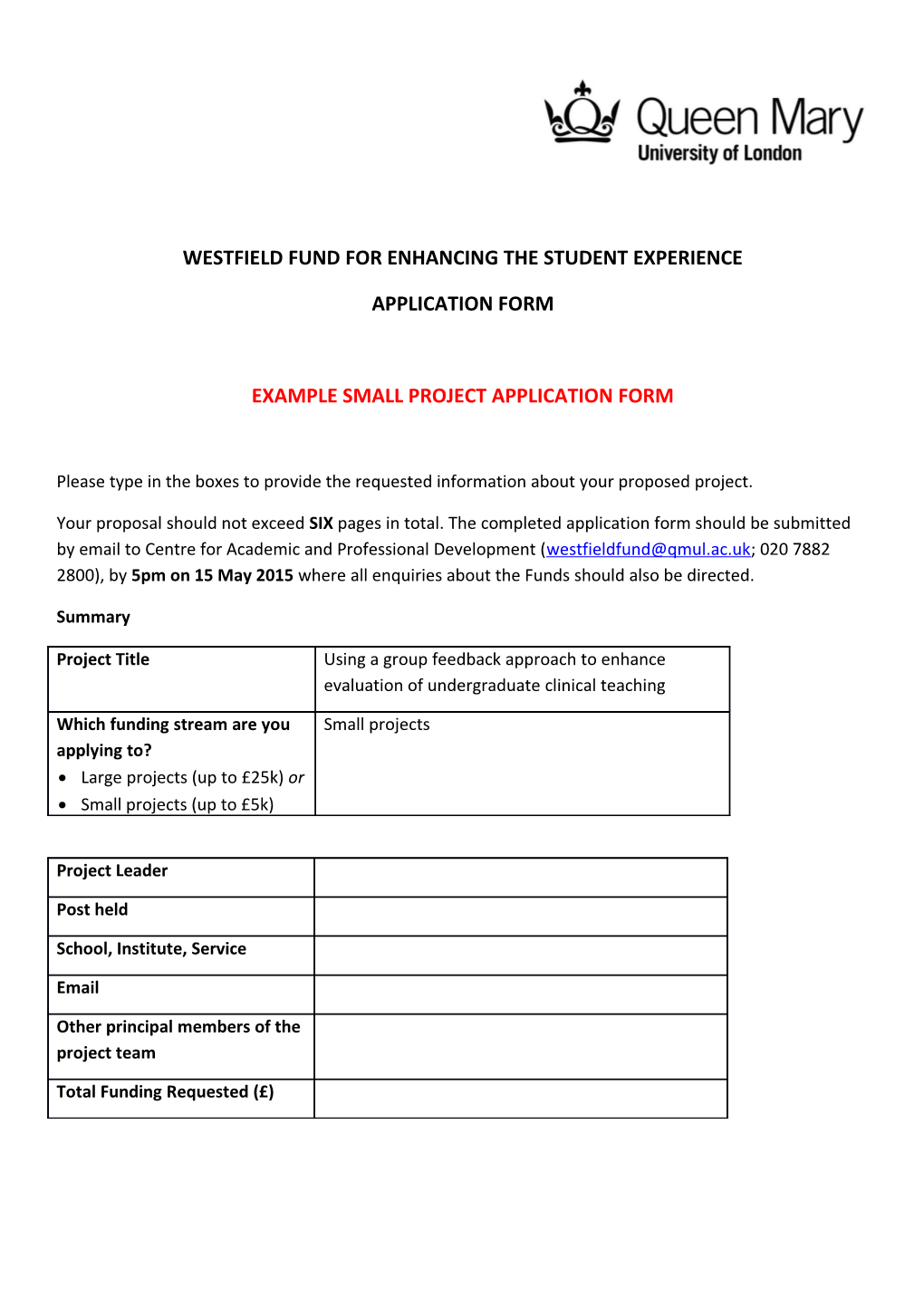
WESTFIELD FUND FOR ENHANCING THE STUDENT EXPERIENCE
APPLICATION FORM
EXAMPLE SMALL PROJECT APPLICATION FORM
Please type in the boxes to provide the requested information about your proposed project.
Your proposal should not exceed SIX pages in total. The completed application form should be submitted by email to Centre for Academic and Professional Development ([email protected]; 020 7882 2800), by 5pm on 15 May 2015 where all enquiries about the Funds should also be directed.
Summary
Project Title Using a group feedback approach to enhance evaluation of undergraduate clinical teaching
Which funding stream are you Small projects applying to? Large projects (up to £25k) or Small projects (up to £5k)
Project Leader
Post held
School, Institute, Service
Other principal members of the project team
Total Funding Requested (£) Project Details
Project Summary
Please provide a brief summary of the project and its broad aim(s). Include any current baseline data or information that has been gathered for the importance/relevance of the project.
In order to maintain and improve quality of teaching, student engagement with the provision of feedback on their learning experience is essential. Currently in the Medical School we ask all students to complete an electronic BOS questionnaire at the end of each clinical placement.
Medicine in Society (MedSoc) is a unit of teaching delivered by primary care clinicians in Year 1 MBBS; students attend GP surgeries, in groups of 6-8 for 12 placement days spread throughout the year; where they undertake small group teaching, meet local voluntary organisations and have some direct patient contact.
In Year 1 feedback response rates for MedSoc range between 20 and 30 %; this means that there are tutors that get no feedback at all, and most get feedback from one or two students. The feedback tends to be polarized; students that were very happy or very unhappy fill it in but rarely provide specific information about what a tutor is doing well or what the student would like to see changed.
This project aims to improve medical student engagement with evaluation of teaching and to help them to develop their skills in giving feedback by asking them to discuss and complete their feedback on their first clinical placement as a group.
A further aim is to improve the quality of the teaching the students receive by providing more detailed feedback for tutors which represents the views of all the students on the placement.
Group feedback is used as a technique at Hull York Medical School (HYMS), students use a template to structure their feedback on their clinical placements and their final product is discussed as a group with placement colleagues and finalized with a facilitator present (Booth, Collins, Hammond, 2008). We have adapted the HYMS template for our context and our pilot tested whether our students, who have been using PBL as a learning method from the beginning of year 1 could discuss and produce a piece of written feedback without a facilitator present. Logistically it would be impossible for a member of faculty to be present at 50 + placement sites across North East London.
Our project addresses the three primary SETLA aims: 1. Ensuring a high quality learning experience for all students. We need feedback that represents the views of all students in order to help tutors deliver a high quality learning experience for all students 2. Supporting students’ achievement through all stages of their educational, personal and professional development. As future doctors, our students will be required to give feedback to senior and junior colleagues, medical students and other healthcare professionals throughout their working lives. This project provides them with an opportunity to discuss the feedback they give on their first clinical placement with their colleagues, as a group they refine their feedback until the group is happy that their comments are a fair reflection of their experience. Negative comments are welcomed but should be presented with constructive suggestions for improvement. 3. Developing staff excellence in teaching and student support. Faculty and clinical tutors want and need more, and better feedback to help them improve their teaching. Our pilot in 2014/15 involved eight placement sites and 50 students. During their penultimate placement day the group of students were allocated an hour during the day when they were asked to undertake a group discussion, reflecting on their own experiences throughout the year. It was suggested that they organised themselves as they do for PBL i.e. appointing a chair to lead the discussion and a scribe to record. The output was a synthesis of comments and feedback for their GP tutor using a template to structure the discussion and the written feedback. This was made available to the tutors after the students had finished their placement.
In 2015/16 (pending Ethics committee approval to extend) we would like to roll this model out to all Year 1 Medicine in Society placements (approximately 320 students at 55-60 sites – 280 MBBS students, 40 GEP students). We would also like to undertake further evaluation of the process with students and tutors at the end of the academic year.
Additional funding will be needed to ensure ongoing GP input into this project. CM will no longer be working as a clinical teaching fellow in 2015/16
Project outcomes
Please provide details of the project outcomes to be delivered with an explicit statement on how the project will impact on the QM student experience. Please relate this to specific areas of activity defined in the National Student Survey.
The aims of the project are to facilitate meaningful engagement of students in the process of evaluating teaching and to encourage reflective practice and development of communication skills through the use of group discussion. In our pilot all students present on the data gathering day took part in the provision of feedback (3 students were unwell across the 8 sites) i.e. 100% of students present contributed to the feedback (cf 20-30% response rate to e-questionnaire). There is further work to be done to see if early engagement with giving feedback in a supportive setting will be sustained but if we can increase student engagement this should improve the response rates including in the NSS.
In addition, by providing personalised, informative evaluation material for teachers we will enable them to develop as educators and to provide a better learning experience for subsequent students thus helping to improve student satisfaction with the teaching, and assessment and feedback areas in the NSS.
Innovative Involvement of students (if appropriate)
All students in MBBS Year 1 will be invited to take part in the project and to attend the seminars on providing group feedback on teaching run by the investigators. Students will have the option to opt out if they do not wish to participate.
Three students involved in focus group discussion as part of the initial pilot project this year will be involved in running the extended project next year. Their roles will include:
Assisting in introducing the concept and aims of the project to first year students who will be participating in the study in 2015.
Co-facilitating focus group discussions (May 2015).
Co-presenting results of the project to GP tutors at the Community-Based Medical Education tutor day June 2016.
Co-presenting at national conference
Project timetable (large projects only)
Please provide an outline timetable (and/or Gantt chart), showing the timescale, key milestones and main activities of the project. This should include the start and completion dates for the project along with a statement of any factors that may affect these.
Sep 2015 –GP tutors informed of project roll-out at training event
Nov 2015 -with participating year 2 students meet MBBS Year 1 students to explain the project and introduce the evaluation proforma.
Feb-Mar 2016 (penultimate placement day) Students undertake group feedback. Students upload group evaluation proforma directly to QM+ (secure virtual learning environment). Students will be reminded about the need to complete this feedback at regular intervals, GP tutors will also be reminded of the need to allocate time and privacy for the students to complete their evaluation. Any groups that fail to submit their evaluation will be asked to complete this on the last placement day (unless the entire group has opted out)
Apr 2016 –Feedback released to relevant tutors via QM+
April 2016 –Focus groups with students
May 2016 –data analysis, preliminary results presented to students and faculty colleagues at the Junior Staff-Student Liaison Committee (JSSLC)
Jun 2016 –disseminate results internally
July 2016 –present results to GP tutors at annual GP tutor training event
Summer 2016 present results at medical education conference and submit abstract for publication
Project Management (large projects only)
Please provide a statement on the proposed project management arrangements to ensure effective delivery of the outcomes, including a clear description of internal (School/Institute) reporting lines.
How you will judge success of the project (large projects only)
Please indicate any indictors to be used during the lifetime of the project and on completion to help ensure that the project goals are met. Quality and quantity of qualitative feedback generated by students
Student opt-out rates
Student focus group feedback
Tutor feedback
Project Evaluation
Please outline the evaluation strategy for the project.
Student focus group discussion – all students will be invited to participate in a focus group to discuss their experience of providing group feedback
GP Tutors will be invited to comment on the process and the feedback they receive and also to participate in a focus group discussion at a tutor education day
Student opt-out numbers will be recorded and monitored over time
Comparative analysis of data from group feedback project with usual (Bristol Online Survey) feedback data
Dissemination
Please provide a brief statement on how the lessons learned in the project can be disseminated to others in the College.
Results of student feedback to be presented to GP tutors at summer education day.
Results will be fed back to students via the Junior Staff-student Liaison Committee
Interim results of pilot project (undertaken this year) were presented at Society for Academic Primary Care (SAPC) conference in Cambridge in January 2015.
Poster will be submitted to QMUL teaching and learning conference.
Abstract will be submitted to a national education conference.
Equality and Diversity (large projects only)
Please briefly state how equality and diversity issues will be incorporated into the project. N/A
Risk management (large projects only)
For large projects please provide a brief risk assessment of the project and a description of the measures that would be taken to mitigate the identified risks.
It is made clear to all students, including those participating in this study that the placement evaluation process is separate to the complaints process. If there is a problem with the teaching they are receiving or if they have concerns about any aspect of clinical care they have seen they should contact the Community-Based Medical Education team to discuss their concerns and if appropriate make a complaint –this should be done when the problem arises. Placement evaluation, whether online or as a group discussion is done to provide feedback for tutors on the teaching. Funding Details
Please provide a detailed itemized breakdown of the use of the proposed funding, clearly identify pay and non-pay costs (expand table as necessary).
Detail of cost Cost (£)
GP tutor input - 14 sessions (7 days in total) over the academic year
Transcription costs (five hours of focus group data)
Dissemination cost – contribution to attendance at national conference, academics and students
Refreshments for focus groups (5 focus groups)
Total (£)
Approval of Head of School/Director of Institute or Professional Service