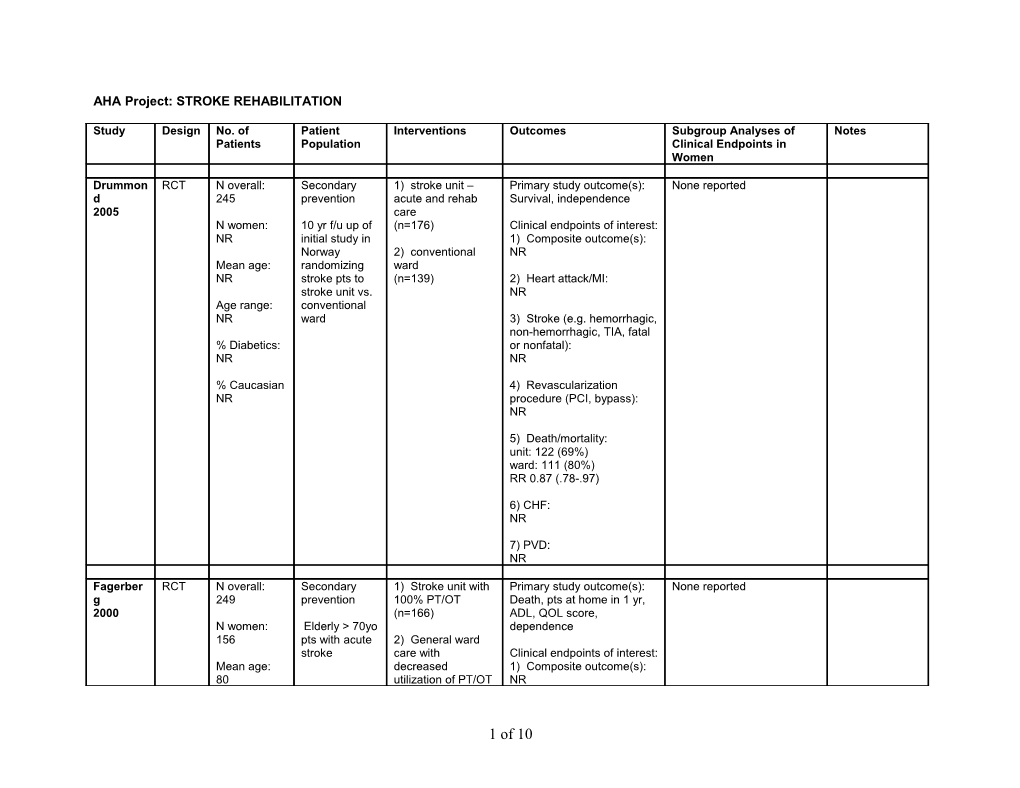
AHA Project: STROKE REHABILITATION
Study Design No. of Patient Interventions Outcomes Subgroup Analyses of Notes Patients Population Clinical Endpoints in Women
Drummon RCT N overall: Secondary 1) stroke unit – Primary study outcome(s): None reported d 245 prevention acute and rehab Survival, independence 2005 care N women: 10 yr f/u up of (n=176) Clinical endpoints of interest: NR initial study in 1) Composite outcome(s): Norway 2) conventional NR Mean age: randomizing ward NR stroke pts to (n=139) 2) Heart attack/MI: stroke unit vs. NR Age range: conventional NR ward 3) Stroke (e.g. hemorrhagic, non-hemorrhagic, TIA, fatal % Diabetics: or nonfatal): NR NR
% Caucasian 4) Revascularization NR procedure (PCI, bypass): NR
5) Death/mortality: unit: 122 (69%) ward: 111 (80%) RR 0.87 (.78-.97)
6) CHF: NR
7) PVD: NR
Fagerber RCT N overall: Secondary 1) Stroke unit with Primary study outcome(s): None reported g 249 prevention 100% PT/OT Death, pts at home in 1 yr, 2000 (n=166) ADL, QOL score, N women: Elderly > 70yo dependence 156 pts with acute 2) General ward stroke care with Clinical endpoints of interest: Mean age: decreased 1) Composite outcome(s): 80 utilization of PT/OT NR
1 of 10 Study Design No. of Patient Interventions Outcomes Subgroup Analyses of Notes Patients Population Clinical Endpoints in Women (n=83) Age range: 2) Heart attack/MI: NR NR
% Diabetics: 3) Stroke (e.g. hemorrhagic, 20.4 non-hemorrhagic, TIA, fatal or nonfatal): % Caucasian NR NR 4) Revascularization procedure (PCI, bypass): NR
5) Death/mortality: 12 mo mortality unit : 45 (27%) ward: 19 (23%)
6) CHF: NR
7) PVD: NR
Kalra RCT N overall: Secondary 1) training care Primary study outcome(s): None reported 2004 300 prevention givers in basic Cost of care, caregiving nursing and burden, functional state, N women: Pts with stroke facilitation of psychological state 140 admitted to personal care Pt institutionalisation stroke rehab techniques 1 yr mortality Mean age: units (n=151) NR Clinical endpoints of interest: 2) conventional 1) Composite outcome(s): Age range: care NR NR (n=149) 2) Heart attack/MI: % Diabetics: NR NR 3) Stroke (e.g. hemorrhagic, % Caucasian non-hemorrhagic, TIA, fatal NR or nonfatal):
2 of 10 Study Design No. of Patient Interventions Outcomes Subgroup Analyses of Notes Patients Population Clinical Endpoints in Women NR
4) Revascularization procedure (PCI, bypass): NR
5) Death/mortality: training:16 (10.6%) conventional 16 (10.4%) p=0.88
6) CHF: NR
7) PVD: NR
Kalra RCT N overall: Secondary 1) acute and rehab Primary study outcome(s): None reported 2000 457 prevention stroke unit Death or institutionalization (n=148) at 12 mos N women: Pts with acute 145 stroke 2) general wards w Clinical endpoints of interest: stroke team 1) Composite outcome(s): Mean age: support NR NR (n=150) 2) Heart attack/MI: Age range: 3) home stroke NR NR care (n=149) 3) Stroke (e.g. hemorrhagic, % Diabetics: non-hemorrhagic, TIA, fatal NR or nonfatal): NR % Caucasian NR 4) Revascularization procedure (PCI, bypass): NR
5) Death/mortality: unit: 13 (9%) team: 34 (23%) home 21 (15%)
3 of 10 Study Design No. of Patient Interventions Outcomes Subgroup Analyses of Notes Patients Population Clinical Endpoints in Women
Odds ratio (95% CI) unit vs team 0.37 (.21-.66), p=0.001 unit vs home 0.59 (.31-1.11), p=0.10 team vs home 1.56 (.96- 2.53), p = 0.07
6) CHF: NR
7)PVD: NR
Kalra RCT N overall: Secondary 1) stroke Primary study outcome(s): None reported 1995 71 prevention rehabilitation unit Mortality (n=34) Destination of discharge N women: Pts with severe - multidisciplinary Barthel Index score 48 stroke planning, emphasis LOS (OPS>5) on rehab care, Mean age: caregiver Clinical endpoints of interest: 78 involvement, 1) Composite outcome(s): counseling NR Age range: NR 2) general medical 2) Heart attack/MI: ward NR % Diabetics: (n=37) NR 3) Stroke (e.g. hemorrhagic, non-hemorrhagic, TIA, fatal % Caucasian or nonfatal): NR NR
4) Revascularization procedure (PCI, bypass): NR
5) Death/mortality: unit: 7 (21%) ward: 17 (46%) p< 0.05 RRR=0.54
4 of 10 Study Design No. of Patient Interventions Outcomes Subgroup Analyses of Notes Patients Population Clinical Endpoints in Women
6) CHF: NR
7) PVD: NR
Langham RCT N overall: Secondary 1) Motor Primary study outcome(s): None reported mer 61 prevention Relearning Motor evaluation, mortality 2003 Programme – at 1 and 4 yrs N women: Pts with 1st physiotherapy with NR time stroke task-oriented Clinical endpoints of interest: strategies 1) Composite outcome(s): Mean age: (n=33) NR NR 2) Bobath 2) Heart attack/MI: Age range: programme – NR NR physiotherapy with facilitation/inhibition 3) Stroke (e.g. hemorrhagic, % Diabetics: strategies non-hemorrhagic, TIA, fatal NR (n=28) or nonfatal): NR % Caucasian NR 4) Revascularization procedure (PCI, bypass): NR
5) Death/mortality: 1 YR: MRP: 6 (18%) bobath: 7 (25%) 4 YRS: MRP: 12 (36%) bobath 12 (43%)
6) CHF: NR
7) PVD: NR
5 of 10 Study Design No. of Patient Interventions Outcomes Subgroup Analyses of Notes Patients Population Clinical Endpoints in Women Musicco Cohort N overall: Secondary Days from stroke to Primary study outcome(s): None reported 2003 study 1,716 prevention rehab initiation Death, early and late rehab 1) <7 (n=515) failure N women: Stroke pts 2) 8-14 (n=264) 842 admitted to 3) 15-30 (n=489) Clinical endpoints of interest: rehab centers 4) >30 (n=448) 1) Composite outcome(s): Mean age: in Italy in 1997- NR 69.5 1998 with and mod-severe 2) Heart attack/MI: Age range: disability Rehab duration NR 20-96 (no n reported) 1) <30d 3) Stroke (e.g. hemorrhagic, % Diabetics: 2) 30d-60d non-hemorrhagic, TIA, fatal NR 3) >60d or nonfatal): NR % Caucasian NR 4) Revascularization procedure (PCI, bypass): NR
5) Death/mortality: Relative risk compared to initiation of rehab 7d from stroke 18-14d: OR 0.90 (95% CI: 0.51-1.56) 15-30d: 0.61 (0.37-1.00) >30d: 1.06 (0.66-1.70)
Relative risk compared to > 60d of rehab duration <30d: 1.37 (0.63-3.01) 30-60d: 2.05 (0.88-4.79)
6) CHF: NR
7) PVD: NR
Ronning RCT N overall: Secondary 1) hospital-based Primary study outcome(s): None reported
6 of 10 Study Design No. of Patient Interventions Outcomes Subgroup Analyses of Notes Patients Population Clinical Endpoints in Women 1998 251 prevention subacute rehab Death, need for long-term unit care, disability N women: Pts in Norway (n=127) 120 were acute Clinical endpoints of interest: stroke pts >60 2) municipality 1) Composite outcome(s): Mean age: yo with SSS health services NR 75.5-76.5 score 12-52. (local environment) (n=124) 2) Heart attack/MI: Age range: NR NR 3) Stroke (e.g. hemorrhagic, % Diabetics: non-hemorrhagic, TIA, fatal 13.5 or nonfatal): NR % Caucasian NR 4) Revascularization procedure (PCI, bypass): NR
5) Death/mortality: hospital: 12 (9.4%) municipality: 20 (16.1%) OR 0.54 (95% CI 0.25-1.16) p=0.11
6) CHF: NR
7) PVD: NR
Rudd RCT N overall: Secondary 1) specialist Primary study outcome(s): None reported 1997 331 prevention community rehab Disability, LOS N women: 3 mos individually- 146 Medically tailored care plan Clinical endpoints of interest: stable stroke n=167 1) Composite outcome(s): Mean age: pts NR 71 2) conventional care 2) Heart attack/MI: Age range: n=164 NR 27-103 3) Stroke (e.g. hemorrhagic,
7 of 10 Study Design No. of Patient Interventions Outcomes Subgroup Analyses of Notes Patients Population Clinical Endpoints in Women % Diabetics: non-hemorrhagic, TIA, fatal NR or nonfatal): NR % Caucasian NR 4) Revascularization procedure (PCI, bypass): NR
5) Death/mortality: 12-mo mortality specialist: 26 (16%) conventional: 34 (21%), p=0.22
6) CHF: NR
7) PVD: NR
Sulch RCT N overall: Secondary 1) integrated care Primary study outcome(s): None reported 2000 152 prevention pathway LOS and functional outcome coordinated by N women: Pts with acute experienced nurse Clinical endpoints of interest: 74 stroke within (n=76) 1) Composite outcome(s): past 2 wks NR Mean age: 2) conventional 74 multidisciplinary 2) Heart attack/MI: care NR Age range: (n=76) NR 3) Stroke (e.g. hemorrhagic, non-hemorrhagic, TIA, fatal % Diabetics: or nonfatal): NR NR
% Caucasian 4) Revascularization NR procedure (PCI, bypass): NR
5) Death/mortality: integrated 10 (10%) conventional 6 (8%), p=NS
8 of 10 Study Design No. of Patient Interventions Outcomes Subgroup Analyses of Notes Patients Population Clinical Endpoints in Women Odds Ratio (95% CI) 0.6 (0.3-2.3)
6) CHF: NR
7) PVD: NR
Thorsen RCT N overall: Secondary 1) Early supported Primary study outcome(s): None reported 2005 83 prevention discharge with Survival, motor capacity, home rehab dysphagial, ADL scale, N women: Pts with mild- (14 wks with 12 subjective dysfunction, falls 25 mod home visits, foci of impairement home visits were Clinical endpoints of interest: Mean age: 5d-7d after speech, 1) Composite outcome(s): 71 acute stroke communication, NR ADL, ambulation Age range: (n=42) 2) Heart attack/MI: NR NR 2) conventional % Diabetics: rehab 3) Stroke (e.g. hemorrhagic, 2.8 (n=41) non-hemorrhagic, TIA, fatal or nonfatal): % Caucasian NR NR 4) Revascularization procedure (PCI, bypass): NR
5) Death/mortality: early: 8 (19%) conventional: 12 (29%) p=NS
6) CHF: NR
7) PVD: NR
9 of 10 REFERENCES:
Drummond, A. E., Pearson, B., Lincoln, N. B., et al. Ten year follow-up of a randomised controlled trial of care in a stroke rehabilitation unit. BMJ. 2005;331(7515):491-2.
Fagerberg, B., Claesson, L., Gosman-Hedstrom, G., et al. Effect of acute stroke unit care integrated with care continuum versus conventional treatment: A randomized 1-year study of elderly patients: the Goteborg 70+ Stroke Study. Stroke. 2000;31(11):2578-84.
Kalra, L. and Eade, J. Role of stroke rehabilitation units in managing severe disability after stroke. Stroke. 1995;26(11):2031-4.
Kalra, L., Evans, A., Perez, I., et al. Alternative strategies for stroke care: a prospective randomised controlled trial.[see comment]. Lancet. 2000;356(9233):894-9.
Kalra, L., Evans, A., Perez, I., et al. Training carers of stroke patients: randomised controlled trial. BMJ. 2004;328(7448):1099-101.
Langhammer, B. and Stanghelle, J. K. Bobath or motor relearning programme? A follow-up one and four years post stroke. Clinical Rehabilitation. 2003;17(7):731- 4.
Musicco, M., Emberti, L., Nappi, G., et al., and Italian Multicenter Study on Outcomes of Rehabilitation of Neurological Patients. Early and long-term outcome of rehabilitation in stroke patients: the role of patient characteristics, time of initiation, and duration of interventions. Archives of Physical Medicine & Rehabilitation. 2003;84(4):551-8.
Ronning, O. M. and Guldvog, B. Outcome of subacute stroke rehabilitation: a randomized controlled trial. Stroke. 1998;29(4):779-84.
Rudd, A. G., Wolfe, C. D., Tilling, K., et al. Randomized controlled trial to evaluate early discharge scheme for patients with stroke. BMJ. 1997;315(7115):1039-44.
Sulch, D., Perez, I., Melbourn, A., et al. Randomized controlled trial of integrated (managed) care pathway for stroke rehabilitation. Stroke. 2000;31(8):1929-34.
Thorsen, A. M., Holmqvist, L. W., de Pedro-Cuesta, J., et al. randomized controlled trial of early supported discharge and continued rehabilitation at home after stroke: five-year follow-up of patient outcome. Stroke. 2005;36(2):297-303.
10 of 10