On Target for Stroke Prevention and Care
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Notice of Election.Qxd
22001188 NN OOTTIICCEE OOFF EELLEECCTTIIOONN AANNdd NNOOMMIINNAATTIIOONN GGuuIIddEE FFOOrr ddIIssTTrrIICCTTss 44 AANNdd 55 College of Chiropractors of Ontario (CCO) January 2018 NOTICE ELECTION TIMETABLE Pursuant to By-law 6: Election of Council January 23, 2018: Notice of Election and Members, notice is hereby given that Nomination Guide sent electronically to elections to CCO Council will be held in members in Districts 4 and 5. Districts 4 and 5. One member will be elected from each of the following districts: February 16, 2018: Nomination Date: Nomination papers, candidate undertakings district 4: Central comprised of the and biographical information in a format 4 city of Toronto and the regional suitable for distribution to voters must be municipality of York. received by CCO by 4 p.m. CCO provides candidates with a copy of the official voters’ list for his/her district. district 5: Central West comprised of 5 the counties of Brant, Dufferin, February 23, 2018: Deadline for Wellington, Haldimand and Norfolk, candidates to withdraw from the election the regional municipalities of Halton, by 4 p.m. Niagara, Peel and Waterloo, and the city of Hamilton. March 2, 2018: List of candidates, biographical information, and voting ELECTION PrOCEdurEs procedures sent electronically to all eligible voters. • Upon receiving completed nomination papers and following the closing of March 27, 2018: Votes for District 4 must be nominations, CCO will provide each received by CCO by 4 p.m. candidate with a copy of the official voters’ list for his/her district. The list March 28, 2018: Unofficial election results shall contain information recorded on announced for District 4. -

Rank of Pops
Table 1.3 Basic Pop Trends County by County Census 2001 - place names pop_1996 pop_2001 % diff rank order absolute 1996-01 Sorted by absolute pop growth on growth pop growth - Canada 28,846,761 30,007,094 1,160,333 4.0 - Ontario 10,753,573 11,410,046 656,473 6.1 - York Regional Municipality 1 592,445 729,254 136,809 23.1 - Peel Regional Municipality 2 852,526 988,948 136,422 16.0 - Toronto Division 3 2,385,421 2,481,494 96,073 4.0 - Ottawa Division 4 721,136 774,072 52,936 7.3 - Durham Regional Municipality 5 458,616 506,901 48,285 10.5 - Simcoe County 6 329,865 377,050 47,185 14.3 - Halton Regional Municipality 7 339,875 375,229 35,354 10.4 - Waterloo Regional Municipality 8 405,435 438,515 33,080 8.2 - Essex County 9 350,329 374,975 24,646 7.0 - Hamilton Division 10 467,799 490,268 22,469 4.8 - Wellington County 11 171,406 187,313 15,907 9.3 - Middlesex County 12 389,616 403,185 13,569 3.5 - Niagara Regional Municipality 13 403,504 410,574 7,070 1.8 - Dufferin County 14 45,657 51,013 5,356 11.7 - Brant County 15 114,564 118,485 3,921 3.4 - Northumberland County 16 74,437 77,497 3,060 4.1 - Lanark County 17 59,845 62,495 2,650 4.4 - Muskoka District Municipality 18 50,463 53,106 2,643 5.2 - Prescott and Russell United Counties 19 74,013 76,446 2,433 3.3 - Peterborough County 20 123,448 125,856 2,408 2.0 - Elgin County 21 79,159 81,553 2,394 3.0 - Frontenac County 22 136,365 138,606 2,241 1.6 - Oxford County 23 97,142 99,270 2,128 2.2 - Haldimand-Norfolk Regional Municipality 24 102,575 104,670 2,095 2.0 - Perth County 25 72,106 73,675 -
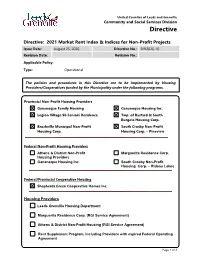
2021 Market Rent Index & Indices for Non-Profit Projects
United Counties of Leeds and Grenville Community and Social Services Division Directive Directive: 2021 Market Rent Index & Indices for Non-Profit Projects Issue Date: August 25, 2020 Directive No.: DIR2020-10 Revision Date: Revision No.: Applicable Policy: Type: Operational The policies and procedures in this Directive are to be implemented by Housing Providers/Cooperatives funded by the Municipality under the following programs. Provincial Non-Profit Housing Providers Gananoque Family Housing Gananoque Housing Inc. Legion Village 96 Seniors Residence Twp. of Bastard & South Burgess Housing Corp. Brockville Municipal Non-Profit South Crosby Non-Profit Housing Corp. Housing Corp. – Pineview Federal Non-Profit Housing Providers Athens & District Non-Profit Marguerita Residence Corp. Housing Providers Gananoque Housing Inc. South Crosby Non-Profit Housing Corp. – Rideau Lakes Federal/Provincial Cooperative Housing Shepherds Green Cooperative Homes Inc. Housing Providers Leeds Grenville Housing Department Marguerita Residence Corp. (RGI Service Agreement) Athens & District Non-Profit Housing (RGI Service Agreement) Rent Supplement Program, including Providers with expired Federal Operating Agreement Page 1 of 3 United Counties of Leeds and Grenville Community and Social Services Division Directive Directive: 2021 Market Rent Index & Indices for Non-Profit Projects Issue Date: August 25, 2020 Directive No.: DIR2020-10 Revision Date: Revision No.: BACKGROUND Each year, the Ministry provides indices for costs and revenues to calculate subsidies under the Housing Services Act (HSA). The indices to be used for 2021 are contained in this directive. PURPOSE The purpose of this directive is to advise housing providers of the index factors to be used in the calculation of subsidy for 2021. ACTION TO BE TAKEN Housing providers shall use the index factors in the table below to calculate subsidies under the Housing Services Act, 2011 (HSA) on an annual basis. -

Ontario Bird Records Committee Report for 1984
2 Ontario Bird Records Committee Report for 1984 by Alan Wormington This is the third annual report of New reports should continue to be the Ontario Field Ornithologists' sent to the OBRC Secretary. We Ontario Bird Records Committee further encourage documentation (OBRC). It contains a total of 190 of rare birds which are not on the records, of which 136 have been Committee's official review list accepted. These figures represent these reports can also be an acceptance rate of about 72%. forwarded to the OBRC Secretary This report officially adds or sent directly to the Royal Mongolian Plover and Swainson's Ontario Museum (Ornithology Warbler to Ontario's Checklist of Dept) where they will be Birds, bringing the provincial total permanently filed. to 429 species. Additionally, The documents and photographs changes to the North/South lists forming the basis for records for Ontario (see Ontario Birds published by the OBRC, together 2:13-23) are: (1) deletion of with all Committee votes and Prairie Warbler from the North, comments, are permanently and (2) addition of American housed in the Ornithology Swallow-tailed Kite to the North Department of the Royal Ontario based on a previously accepted Museum, Toronto. All photo record (Ontario Birds 2:56), but graphic material received by the mistakenly overlooked by OBRC Committee is incorporated into the as a northern Ontario occurrence. existing ROM photographic The 1984 Committee consisted collection; the purposes of this of Robert Curry (Chairman), Alan collection have been outlined Wormington (Secretary), A. previously by James (1977). All David Brewer, G. Thomas Hince, interested parties are at liberty to RD. -

Public Consultation Reports
Citizens' Assembly on Electoral Reform Public Consultation Reports February 2007 overview what we heard what we read special outreach focus groups ONTARIO CITIZENS’ ASSEMBLY ON ELECTORAL REFORM CONSULTATION REPORTS overview From October 2006 through January 2007, the Citizens’Assembly on Electoral Reform undertook consultations with Ontario citi- In addition, many Assembly members undertook out- zens to learn what they value in an electoral system. reach in their own communities to get the word out The Assembly began the process with the release of about the Assembly and to find out what people in its public consultation guide,“Citizens Talking to their ridings thought about electoral reform. Citizens.”The guide asked the public four questions: While people participated in the consultation in 1. Which electoral system principles are most different ways, they had at least one thing in common: important to you? Why? a concern for the future of Ontario and the shape • Are there other principles you think are of one of its most important political institutions. important? Why? Altogether, about 3,000 people shared their views 2. Does Ontario’s current electoral system reflect the with the Assembly.They were people who had principles that are important to you? If yes, why? studied electoral systems and people who had not; If no, why not? people who were young and not so young; individual citizens and representatives of organizations; and 3. Do you think Ontario should keep its current people diverse in occupation, political stripe, electoral system or change to a different one? culture, experience, and point of view.The • If you think Ontario should change to a participants were as diverse as the Assembly itself. -

Province Approves 13 New Ontario Health Teams
BACKGROUNDER Province Approves 13 New Ontario Health Teams November 18, 2020 Oce of the Premier The Ontario government is announcing the approval of 13 new Ontario Health Teams across the province. Ontario Health Teams are a new way of delivering care that brings together health care providers and organizations to work as one coordinated team to improve patient outcomes, strengthen local services, and make it easier for patients and families to navigate the system and transition between health care providers. The 13 new Ontario Health Teams are: · Brantford Brant Ontario Health Team in Brantford and Brant County. · Downtown East Toronto Ontario Health Team in Downtown East Toronto. · Frontenac, Lennox & Addington Ontario Health Team in the Frontenac, Lennox and Addington region, including Kingston, Greater Napanee and surrounding rural communities. · Kawartha Lakes Ontario Health Team in the City of Kawartha Lakes and surrounding areas. · Kitchener, Waterloo, Wellesley, Wilmot and Woolwich Ontario Health Team in Kitchener, Waterloo, Wilmot, Woolwich and Wellesley. · Lanark, Leeds and Grenville Ontario Health Team in the United Counties of Leeds and Grenville, and southern Lanark County area. · Mid-West Toronto Ontario Health Team in the west end of downtown Toronto. · Oxford and Area Ontario Health Team in Oxford County and the surrounding area. · Rainy River Ontario Health Team in the Rainy River District. · Sarnia Lambton Ontario Health Team in the Sarnia-Lambton region. · Scarborough Ontario Health Team in Scarborough and surrounding communities. · South Georgian Bay Ontario Health Team in the South Georgian Bay Region, including Collingwood, Wasaga Beach, Clearview and The Blue Mountains. · West Toronto Ontario Health Team in West Toronto. -

Candidate's Statement of Unpaid Claims and Loans 18 Or 36 Months
Candidate’s Statement of Unpaid Claims and Loans 18 or 36 Months after Election Day (EC 20003) – Instructions When to use this form The official agent for a candidate must submit this form to Elections Canada if unpaid amounts recorded in the candidate’s electoral campaign return are still unpaid 18 months or 36 months after election day. The first update must be submitted no later than 19 months after the election date, covering unpaid claims and loans as of 18 months after election day. The second update must be submitted no later than 37 months after election day, covering unpaid claims and loans as of 36 months after election day. Note that when a claim or loan is paid in full, the official agent must submit an amended Candidate’s Electoral Campaign Return (EC 20120) showing the payments and the sources of funds for the payments within 30 days after making the final payment. Tips for completing this form Part 1 ED code, Electoral district: Refer to Annex I for a list of electoral district codes and names. Declaration: The official agent must sign the declaration attesting to the completeness and accuracy of the statement by hand. Alternatively, if the Candidate’s Statement of Unpaid Claims and Loans 18 or 36 Months after Election Day is submitted online using the Political Entities Service Centre, handwritten signatures are replaced by digital consent during the submission process. The official agent must be the agent in Elections Canada’s registry at the time of signing. Part 2 Unpaid claims and loans: Detail all unpaid claims and loans from Part 5 of the Candidate’s Electoral Campaign Return (EC 20121) that remain unpaid. -

Made to Order Christmas Fare at the Brantford Farmers' Market
DECEMBER 2019 BRANTFORD | BRANT SIX NATIONS FREE EVENT GUIDE PAGES 11-12, 17 Book Today: 519-442-4452 www.ParisDentalCentre.com [email protected] LIVE MUSIC EVERY FRIDAY AND SATURDAY ALL ROADS LEAD HERE 190 King George Road Brantford, Ontario (519) 304-7625 BSCENE FOOD SCENE Our Kitchen Brantford page 5 BSCENE WITH BSCENE pages 10, 18, 23, 26 & 27 YOUR NEIGHBOURHOOD EXPERTS page 8 - 9 BRANTFORD SYMPHONY OPRCHESTRA More Christmas Bells page 6 COUNTY OF BRANT PUBLIC LIBRARY Made to order Christmas fare at New Website Launched page 19 the Brantford Farmers’ Market A LOOK BACK Settlement Growth in Upper STORY PAGE 3 Canada: Canada West page 24 - 25 2 Entertainment & Community Guide INSIDE BE SEEN WITH this issue DEC 2019 Vol. 6, Edition 3 BScene is a local Entertainment & Community Made to Order Fare at The Guide, showcasing the #BRANTastic features of 3 Brantford Farmers Market Brantford, Brant and Six Nations through engaging BSCENE content and with the Best Event Guide in our community. Brant Food for Thought 4 BScene is distributed free, every month through Steve's Teas 4 key community partners throughout Brantford, Brant and Six Nations. BScene has a local network BSCENE Food Scene of over 500 distribution points including local 5 BSCENE AROUND advertisers, retail outlets, dining establishments, Our Kitchen Brantford and community centres. For a complete list, please visit bscene.ca Sultans of String 6 TOWN IN NOVEMBER As a community paper and forum for sharing Brantford Symphony Orchestra 6 thoughts and experiences, the views expressed in the magazine are not necessarily those of the Publisher, Editor, other contributors, advertisers BSCENE Music Scene 7 or distributors unless otherwise stated. -

The Horan Family Diaspora Since Leaving Ireland 191 Years Ago
A Genealogical Report on the Descendants of Michael Horan and Mary Minnock by A.L. McDevitt Introduction The purpose of this report is to identify the descendants of Michael Horan and Mary Minnock While few Horans live in the original settlement locations, there are still many people from the surrounding areas of Caledon, and Simcoe County, Ontario who have Horan blood. Though heavily weigh toward information on the Albion Township Horans, (the descendants of William Horan and Honorah Shore), I'm including more on the other branches as information comes in. That is the descendants of the Horans that moved to Grey County, Ontario and from there to Michigan and Wisconsin and Montana. I also have some information on the Horans that moved to Western Canada. This report was done using Family Tree Maker 2012. The Genealogical sites I used the most were Ancestry.ca, Family Search.com and Automatic Genealogy. While gathering information for this report I became aware of the importance of getting this family's story written down while there were still people around who had a connection with the past. In the course of researching, I became aware of some differences in the original settlement stories. I am including these alternate versions of events in this report, though I may be personally skeptical of the validity of some of the facts presented. All families have myths. I feel the dates presented in the Land Petitions of Mary Minnock and the baptisms in the County Offaly, Ireland, Rahan Parish registers speak for themselves. Though not a professional Genealogist, I have the obligation to not mislead other researchers. -

2014 Reports) Is Indicated in Secretary ([email protected])
Ontario Bird Records Committee Report for 2014 Mike V.A. Burrell and Barbara N. Charlton Introduction This is the 33rd annual report of the The members of the 2014 Committee Ontario Bird Records Committee were Brandon R. Holden (chair), Mike (OBRC) of the Ontario Field Ornitholo - V.A. Burrell (non-voting secretary), Bar - gists. The OBRC reviews rare bird reports bara N. Charlton (non-voting assistant to in Ontario based on documentation that the secretary), Ross W. Wood, William J. has been submitted by the birding com - Crins, Peter S. Burke, Mark Gawn, Ron munity and would cease to function with - Ridout and Bruce M. Di Labio (Figure 1). out this effort and support. Species and Mark K. Peck acted as Royal Ontario subspecies evaluations are based on the Museum (ROM) liaison for the OBRC. Review Lists for Ontario, which can be found on the OFO website (www.ofo.ca). Changes to the Checklist of Ontario Birds Any new species, subspecies, or first No new species were added to the Ontario breeding records for Ontario are also list, leaving the total at 490 species. reviewed. This report deals with the Changes to the Review Lists review of 187 records by the OBRC in 2014 of which 80% were accepted. All This report is the first to utilize three reports reviewed by the 2014 Committee review zones (Lowlands, Central and will be added to the permanent file kept at South). See Holden (2014) for more the Royal Ontario Museum. details on this change. Visit the OFO website (www.ofo.ca) or contact the sec - retary ([email protected]) directly for the full review lists. -

The Canadian Parliamentary Guide
NUNC COGNOSCO EX PARTE THOMAS J. BATA LI BRARY TRENT UNIVERSITY us*<•-« m*.•• ■Jt ,.v<4■■ L V ?' V t - ji: '^gj r ", •W* ~ %- A V- v v; _ •S I- - j*. v \jrfK'V' V ■' * ' ’ ' • ’ ,;i- % »v • > ». --■ : * *S~ ' iJM ' ' ~ : .*H V V* ,-l *» %■? BE ! Ji®». ' »- ■ •:?■, M •* ^ a* r • * «'•# ^ fc -: fs , I v ., V', ■ s> f ** - l' %% .- . **» f-•" . ^ t « , -v ' *$W ...*>v■; « '.3* , c - ■ : \, , ?>?>*)■#! ^ - ••• . ". y(.J, ■- : V.r 4i .» ^ -A*.5- m “ * a vv> w* W,3^. | -**■ , • * * v v'*- ■ ■ !\ . •* 4fr > ,S<P As 5 - _A 4M ,' € - ! „■:' V, ' ' ?**■- i.." ft 1 • X- \ A M .-V O' A ■v ; ■ P \k trf* > i iwr ^.. i - "M - . v •?*»-• -£-. , v 4’ >j- . *•. , V j,r i 'V - • v *? ■ •.,, ;<0 / ^ . ■'■ ■ ,;• v ,< */ ■" /1 ■* * *-+ ijf . ^--v- % 'v-a <&, A * , % -*£, - ^-S*.' J >* •> *' m' . -S' ?v * ... ‘ *•*. * V .■1 *-.«,»'• ■ 1**4. * r- * r J-' ; • * “ »- *' ;> • * arr ■ v * v- > A '* f ' & w, HSi.-V‘ - .'">4-., '4 -' */ ' -',4 - %;. '* JS- •-*. - -4, r ; •'ii - ■.> ¥?<* K V' V ;' v ••: # * r * \'. V-*, >. • s s •*•’ . “ i"*■% * % «. V-- v '*7. : '""•' V v *rs -*• * * 3«f ' <1k% ’fc. s' ^ * ' .W? ,>• ■ V- £ •- .' . $r. « • ,/ ••<*' . ; > -., r;- •■ •',S B. ' F *. ^ , »» v> ' ' •' ' a *' >, f'- \ r ■* * is #* ■ .. n 'K ^ XV 3TVX’ ■■i ■% t'' ■ T-. / .a- ■ '£■ a« .v * tB• f ; a' a :-w;' 1 M! : J • V ^ ’ •' ■ S ii 4 » 4^4•M v vnU :^3£'" ^ v .’'A It/-''-- V. - ;ii. : . - 4 '. ■ ti *%?'% fc ' i * ■ , fc ' THE CANADIAN PARLIAMENTARY GUIDE AND WORK OF GENERAL REFERENCE I9OI FOR CANADA, THE PROVINCES, AND NORTHWEST TERRITORIES (Published with the Patronage of The Parliament of Canada) Containing Election Returns, Eists and Sketches of Members, Cabinets of the U.K., U.S., and Canada, Governments and Eegisla- TURES OF ALL THE PROVINCES, Census Returns, Etc. -

Consultation Guide Final
Citizens Talking to Citizens Public Consultation Guide Ontario Citizens’ Assembly on Electoral Reform Contact Information Print copies of this document are available at ServiceOntario/Government Information Centres in more than 60 communities around the province. For the location closest to you, please visit www.serviceontario.ca. Electronic copies are available in .pdf.Visit the Citizens’Assembly website at www.citizensassembly.gov.on.ca. Alternative-format copies are available on request at [email protected] Une publication équivalente est disponible en français au site web suivant : www.assembleedescitoyens.gouv.on.ca. © Queen’s Printer for Ontario, 2006 O ntario has changed significantly since Get Involved our first parliament was elected in 1792. Since that time the electoral system has The Assembly would like to hear from as never been publicly considered or evaluated. many Ontarians as possible: those who Some people think the current system know a lot about electoral systems, and has stood the test of time. Other people those who are just beginning to think or think it’s time for a change.The Citizens’ learn about the subject.The consultation Assembly process gives all Ontarians an period will run from late October 2006 to opportunity to learn more about Ontario’s the end of January 2007.What you tell us current electoral system, as well as others, will assist the Assembly when we discuss and to decide which one they think is what to recommend to the government. best for this province. This guide will help you present your The Citizens’ Assembly wants to ideas to the Assembly, however you hear what you think.