Online Documents
Appendix 1 – Search strategy
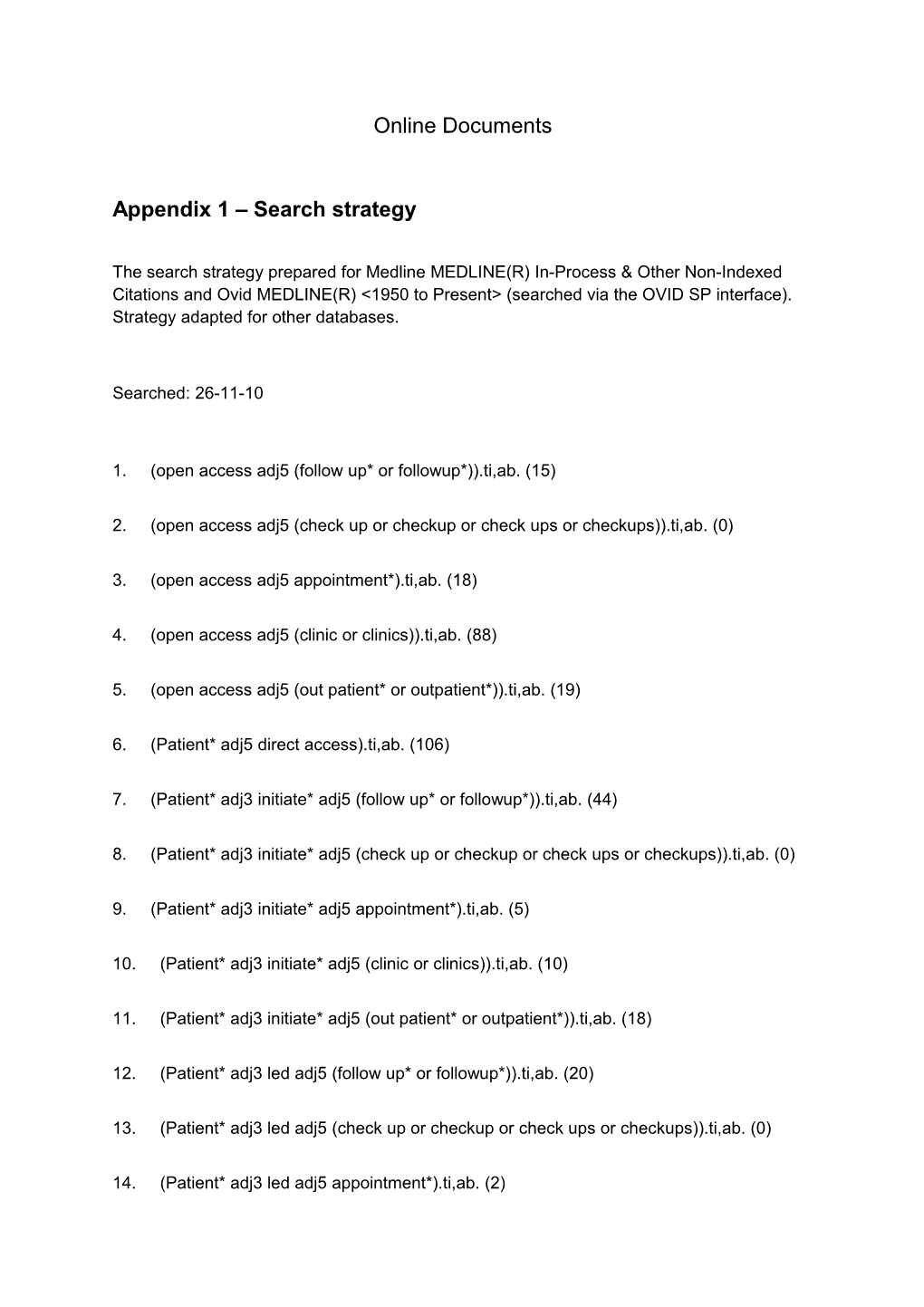
The search strategy prepared for Medline MEDLINE(R) In-Process & Other Non-Indexed Citations and Ovid MEDLINE(R) <1950 to Present> (searched via the OVID SP interface). Strategy adapted for other databases.
Searched: 26-11-10
1. (open access adj5 (follow up* or followup*)).ti,ab. (15)
2. (open access adj5 (check up or checkup or check ups or checkups)).ti,ab. (0)
3. (open access adj5 appointment*).ti,ab. (18)
4. (open access adj5 (clinic or clinics)).ti,ab. (88)
5. (open access adj5 (out patient* or outpatient*)).ti,ab. (19)
6. (Patient* adj5 direct access).ti,ab. (106)
7. (Patient* adj3 initiate* adj5 (follow up* or followup*)).ti,ab. (44)
8. (Patient* adj3 initiate* adj5 (check up or checkup or check ups or checkups)).ti,ab. (0)
9. (Patient* adj3 initiate* adj5 appointment*).ti,ab. (5)
10. (Patient* adj3 initiate* adj5 (clinic or clinics)).ti,ab. (10)
11. (Patient* adj3 initiate* adj5 (out patient* or outpatient*)).ti,ab. (18)
12. (Patient* adj3 led adj5 (follow up* or followup*)).ti,ab. (20)
13. (Patient* adj3 led adj5 (check up or checkup or check ups or checkups)).ti,ab. (0)
14. (Patient* adj3 led adj5 appointment*).ti,ab. (2) 15. (Patient* adj3 led adj5 (clinic or clinics)).ti,ab. (21)
16. (Patient* adj3 led adj5 (out patient* or outpatient*)).ti,ab. (8)
17. (Patient* adj3 request* adj5 (follow up* or followup*)).ti,ab. (58)
18. (Patient* adj3 request* adj5 (check up or checkup or check ups or checkups)).ti,ab. (2)
19. (Patient* adj3 request* adj5 appointment*).ti,ab. (28)
20. (Patient* adj3 request* adj5 (clinic or clinics)).ti,ab. (26)
21. (Patient* adj3 request* adj5 (out patient* or outpatient*)).ti,ab. (11)
22. (self* adj1 referr* adj5 (follow up* or followup*)).ti,ab. (13)
23. (self* adj1 referr* adj5 (check up or checkup or check ups or checkups)).ti,ab. (1)
24. (self* adj1 referr* adj5 appointment*).ti,ab. (1)
25. (self* adj1 referr* adj5 (clinic or clinics)).ti,ab. (47)
26. (self* adj1 referr* adj5 (out patient* or outpatient*)).ti,ab. (15)
27. (patient adj5 (led or request* or initiate*) adj5 review).ti,ab. (25)
28. 1 or 2 or 3 or 4 or 5 or 6 or 7 or 8 or 9 or 10 or 11 or 12 or 13 or 14 or 15 or 16 or 17 or
18 or 19 or 20 or 21 or 22 or 23 or 24 or 25 or 26 or 27 (553)
29. "Delivery of Health Care"/ (53544)
30. "Referral and Consultation"/ (44989)
31. Health Services Accessibility/ (39281)
32. outpatient clinics, hospital/ (13274)
33. 29 or 30 or 31 or 32 (143984)
34. 28 and 33 (161) Figure S21 Logic model of traditional and Patient Initiated Clinic appointment systems Table S1 – Characteristics of patient initiated clinics in included studies
Study Written Telephone help Initial Annual
information line consultation checkup
Brown (2002) √ √ × √
Sheppard (2009) × √ × √
Kennedy (2003) √ √ √ √ (some
(guidebook) cases)
Robinson (2001) √ √ √ √ (some
(guidebook) cases)
Williams (2000) × √ (+ GP × √ (24mths)
contact)
Hewlett (2000) × √ (+ GP × ×
contact)
Kirwan (2003) × √ × √ (24mths)
Hewlett (2005) × √ × √ (24mths)
Sands (2009) × √ √ × Table S23: Study Quality
Key
? = unclear X = not reported in study = reported in study N/A = not applicable
Partial = only some of the data was reported or applicable
Brown Hewlett, Hewlett, Kennedy, Kirwan, Robinson, Sands, Sheppard, Williams,
2002 2000 2005 2003 2003 2001 2009 2009 2000
Design RCT RCT RCT RCT RCT RCT Cross- RCT RCT
sectional
Eligibility criteria specified
Power X X calculation
Sample size ? ? X ? ? X ? adequate
Adequately ? ? ? ? N/A randomised
Allocation ? ? ? X ? X N/A X concealed
Baseline details X
Groups similar ? at baseline
Adequately N/A N/A X ? X N/A N/A N/A adjusted analysis
Co-interventions X ?
Patients blinded N/A N/A N/A N/A N/A N/A N/A X N/A to treatment
Assessors ? ? X X ? X X X X blinded Compliance with ? ? ? ? treatment
Sub group N/A N/A N/A N/A N/A N/A N/A N/A analysis justified
Valid measures Partial Partial Partial Partial X Partial X
Reliable Partial Partial Partial Partial X Partial X measures
All participants Partial X accounted for
Appropriate Partial Partial ? analysis
ITT analysis X X X X X X ?
> 80% X X X participants in follow-up
Conclusions X X ? supported by results
Inter centre X N/A N/A ? N/A ? N/A N/A ? variability Appendix 2
Data Extraction and Quality Appraisal form
B I B L I O G R A P H I C D E T A I L S
Reference no: First author: Title: Year: Citation:
S T U D Y I N T E R V E N T I O N
Country: Description of Intervention: Setting: Description of Comparator: Recruitment dates: Notes: Is the intervention described in sufficient detail for it to be Study design: replicated elsewhere? Funding source: Notes:
S U B J E C T S
Total number: Inclusion criteria: Exclusion criteria:
P A T I E N T C H A R A C T E R I S T I C S O U T C O M E M E A S U R E S
Mean interventio Primary outcome measure: (SD) control n Secondary measures: N: Age yrs: Method of assessing outcomes: Sex: Length of follow-up: M F Notes: This section should include a list of outcomes measured and the methods of measuring them not the results. Are the questionnaires validated? Is the primary outcome measure specified?
R E S U L T S
Total number of participants enrolled: Number lost to follow-up (if appropriate):
interventi control on mean n mean (sd) n (sd) Outcome s
Adverse events: Type of analysis (intention to treat, per protocol): Results of study analysis (e.g. Dichotomous: odds ratio, risk ratio and confidence intervals, p-value; Continuous: mean difference, confidence intervals): Notes: Q U A L I T Y A P P R A I S A L
1. Study design {RCT; X-over trial: CCT; pre-post study} 2. Were the study eligibility criteria specified? {yes; no; partial} 3. Was a power calculation performed? {yes; no} 4. Is the sample size adequate? {yes; no; unclear} 5. Is the number randomized stated? {yes; no; not applicable} 6. Is the study properly randomized ┼ {yes: no; not applicable; unclear} 7. Is allocation of treatment concealed? ╪ {yes; no; not applicable; unclear} 8. Are adequate baseline details escribed? {yes; no; partial} 9. Are groups similar at baseline? {yes; no; partial; not applicable} 10. Are baseline imbalances adequately adjusted for in the analysis? {yes; no; not applicable; unclear} 11. Are similar co-interventions administered? {yes; no; unclear; not applicable} 12. Are patient’s blinded to treatment allocation?
13. Are outcome assessors blinded? {yes; no; unclear} 14. Is compliance with treatment adequate? {yes; no; unclear; not reported} 15. Were any sub-group analysis justified? {yes; no; not applicable} 16. Were data collection tools shown or known to be valid for the outcome of interest?± {yes; no; unclear} 17. Were the data collection tools known or were shown to be consistent and accurate in measuring the outcome of interest?* {yes; no; unclear} 18. Were all study participants accounted for? {yes; no} 19. Are data analyses appropriate? {yes; no; partial; unclear} 20. Is analysis conducted on an ITT basis? {yes; no; not applicable} 21. Are greater than 80% of patients included in the follow-up assessment? {yes; no; unclear} 22. Are the conclusions supported by the results? {comment} 23. Generalisability {comment} 24. Inter-centre variability {comment} 25. General comments {comment} ┼ Adequate approaches top sequence generation: computer-generated random numbers, random number tables; inadequate approaches: use of alternation, case record numbers, birth dates or week days ╪ Adequate approaches to concealment allocation: centrally or pharmacy-controlled randomisation, inadequate approaches: serially numbered envelopes, use of alternation, open random number lists ± The tools are known to be valid or were shown to measure what they are intended to measure * The tools are known to be reliable or were shown to be consistent and accurate in measuring the outcome of interest (e.g. test-retest, Cronback’s alpha, interrater reliability)
G E N E R A L C O M M E N T S
Data extraction performed by: Date: Data extraction checked by: Date: Appendix 3
Psychological and HRQOL Outcomes (results as in original articles)
Study Outcomes Results
Intervention Standard Care comments
Mean (Std. Deviation) M (SD)
Brown, et al. (2002) At 12mths NA
BC EORTC QLQ-C30
- Physical funct 5 (5,8) – 1 6 (5,8) – 2 - Role funct - Pain 2 (2,3) – 0 2 (2,3) – 0 - Dyspnoea 1 (1,3) – 1 1 (1,3) – 1 - Constipation - Diarrhoea 1 (1,3) – 1 1 (1,4) – 1 - Cognitive funct - Emotional funct 1 (1,3) – 0 1 (1,3) – 0 - Social funct - Fatigue 1 (1,2) – 0 1 (1,2) – 0 - Nausea 3 (2,4) – 1 3 (2,6) – 1 - Sleep disturb - Loss appetite 5 (4,15) – 3 6 (4,15) – 3.5
2 (2,4) – 0 2 (2,5) – 0.25
4 (3,9) – 1.5 5 (3,8) – 2
2 (2,3) – 0 2 (2,4) – 0
1.5 (1,3) – 1 2 (1,4) – 1 1 (1,3) – 0 1 (1,2) – 0 HAD
- Anxiety 4 (0,12) 6.5 (0,16)* *P=0.069 - Depression 1 (0,7) 2 (0,8)* *P=0.232
EORTC QLQ-BR23
- Arm symptoms 3 (3,6) – 1 4 (3,7) – 2 - Breast symps - Systemic 4 (4,7) – 1 5 (4,8) – 2 P=0.024 therapy side eff 9 (7,13) – 3.25 9 (7,14) – 2.5 - Body image - Sexual funct Future perspect 5 (4,10) – 2.25 5 (4,8) – 2
2 (2,12) – 4 2 (1,12) – 1.5 1 (1,3) – 1 2 (1,3) – 0
Sheppard et al. (2009) At 18mths NA BC GHQ (likert)
Aggregate score 22.8 23.0
Cases>4 15 (14%) 21 (20%)
FACT-G 81.4 81.3 NA
FACT Breast 20.1 21.8
FACT endocrine 57.4 58.7
FACT B+ES 158.9 161.9
Fear 5.6 5.0 NA Kennedy et al (2003) At entrance IBD Enablement (after 4.0 (3.9) 3.0 (3.9) P=0.026 consultation)
Satisfaction with initial consultation 65.4 (12.0) 62.1 (12.3) P=0.09
At 12mths
IBDQ score 172.3 (36.6) 167.7 (37.5) P=0.45
SF36 –
Physical functioning 78.1 (25.3) 75.8 (26.6) P=0.21
Role limitations physical 61.4 (44.1) 60.3 (43.2) P=0.91
Role limitations emotional 72.2 (41.0) 72.3 (39.6) P=0.71 Social functioning
Mental health 74.8 (31.2) 72.2 (29.5) P=0.13 Energy 70.3 (20.9) 67.8 (21.3) P=0.40 Pain 51.8 (24.5) 48.2 (25.4) P=0.09 General health perception 69.5 (27.6) 67.1 (23.6) P=0.22 53.2 (25.1) 49.4 (1.8) P=0.12
HADS 11.7 (7.9) 12.3 (7.6) P=0.40 Satisfaction with hospital 54.6 (8.5) 53.6 (9.1) P=0.62 visits
Preferred fixed appt 25.7% 40.6% P<0.001 Preferred flexible appt 74.3% 59.4% P<0.001 Changed thought of illness (%yes) 25.0% 13.2%
Changed managed illness (%yes) 20.2% 6.9% Changed thought consultant (%yes) 15.2% 12.3%
Mean EQ-5D score 0.7071 0.6909
Robinson et al, (2001) At 14 mths
IBD Acceptability patient 82% preferred new int 95% preferred new int
100% pref new int
Acceptability clinician 100% pref new int
IBDQ QOL 189 183 P=0.16 Williams et al, (2000) At 24mths Mean difference
IBD SF36 –
- Physical funct Control better -3.7 (3.2, -10.5) - Role limits (physical probs) Control better -2.7 (11.4, -16.8) - Role limits (emotion probs) - Social funct Control better -5.3 (11.4, -22.0) - Mental health - vitality - bodily pain - General health Control better -0.4 (8.1, -8.9) perception Control better -3.7 (2.4, -9.9)
Control better -3.7 (3.3, -10.7)
Control better -2.5 (5.0, -10.0)
Control better -3.5 (2.0, -8.9)
UKIBDQ – bowel Intervention better 0.3 (7.7, -7.1) movements/use of fac
- General bowel symptoms Control better -3.5 (4.0, -10.9) - Systemic funct - emotional function Intervention better 2.2 (9.9, -5.6) - Social function Control better -1.3 (3.4, -5.9)
Intervention better 0.4 (6.5, -5.7) - Patient 85% 41% preference INT - GP preference INT 55 patients 53 patients - GP preference CON
15 patients 20 patients
Hewlett, 2000 At 24 months
(RA) Anxiety Increased 3% Increased 11% NS
Depression Increased 4% Increased 14% NS
Self efficacy 63 55 P=0.053
Patient satisfaction 8.56cm 7.89cm P<0.05
Confidence in system 8.5cm 7.5cm P<0.05
GP satisfaction 7.66cm 7.39cm
GP confidence (in sys) 7.46cm 7.65cm
Kirwan, 2003 Change in scores 0- 48mths (RA) Anxiety 0.5 0.5
Depression 0.2 0.3
Helplessness -0.2 1.0
Self-efficacy – pain 5.1 7.4 Self-efficacy - function -1.4 -7.3
Self-efficacy – other 0.4 -4.4
Satisfaction 0.5 -0.8 P<0.001
Confidence 0.5 -0.6 P<0.001
Hewlett, 2005 Median change and range at 6 years
Anxiety 0 (-2.0 – 3.0) 0 (-2.0 – 3.0) P=0.95
Depression 0 (-1.0 – 3.0) 0 (-1.0 – 2.75) P=0.80
Helplessness 1.5 (-3.0 – 3.0) 1.0 (-1.75 – 4.0) P=0.20 Self-efficacy – pain 2.0 (12.0 – 16.0) 1.0 (-10.0 – 19.0) P=0.49 -6.6 (-20.6 – 2.40) Self-efficacy - function -2.75 (-15.9 – 5.0) P=0.19 6.7 (-15.0 – 6.7) Self-efficacy – other -3.30 (-11.6 – 8.3) P=0.25
Satisfaction 0 (-0.7 – 0.9) 1.1 (-2.70 – 0.25) P=0.0004
Confidence 0.15 (-0.73 – 0.43) -1.0 (-2.35 – 0.20) P=0.0005
GP satisfaction 8.4 (7.5 – 9.6) 7.5 (5.5 – 8.57) P=0.005
GP Confidence 8.4 (7.25 – 9.45) 8.0 (5.72 – 8.7) P=0.04
Sands, 2009 QOL AIMS2-SF score 19.25 (7.79) 18.71 (7.33) P=0.746
(RA) Anxiety and Depression 14.78 (8.10) 14.54 (7.73) P=0.890 (HADS score)
P satisfaction 7.15 (3.41) 7.17 (3.02) P=0.990
P confidence 7.35 (3.23) 7.39 (2.85) P=0.995 PLUS