RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, BANGALORE KARNATAKA
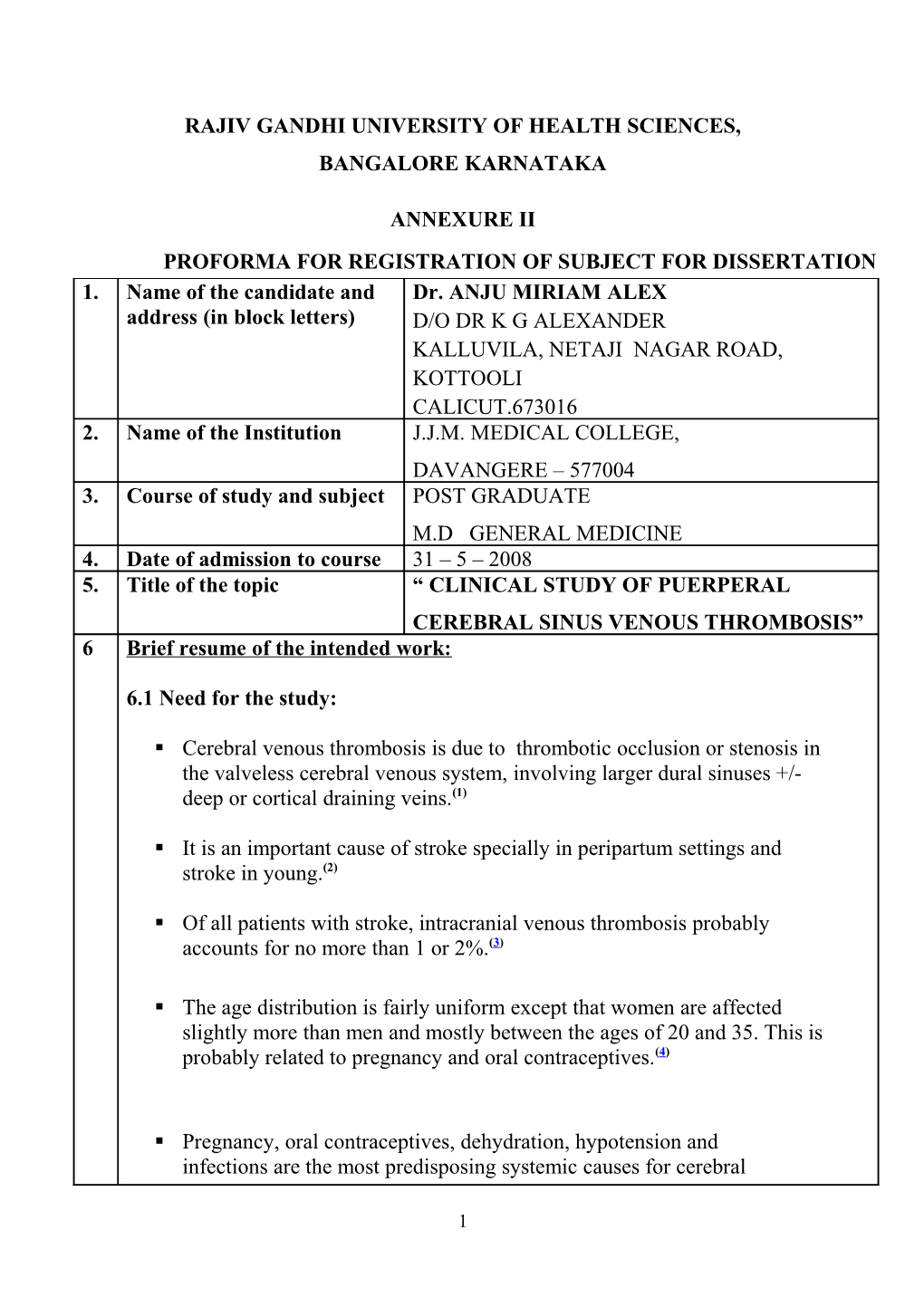
ANNEXURE II PROFORMA FOR REGISTRATION OF SUBJECT FOR DISSERTATION 1. Name of the candidate and Dr. ANJU MIRIAM ALEX address (in block letters) D/O DR K G ALEXANDER KALLUVILA, NETAJI NAGAR ROAD, KOTTOOLI CALICUT.673016 2. Name of the Institution J.J.M. MEDICAL COLLEGE, DAVANGERE – 577004 3. Course of study and subject POST GRADUATE M.D GENERAL MEDICINE 4. Date of admission to course 31 – 5 – 2008 5. Title of the topic “ CLINICAL STUDY OF PUERPERAL CEREBRAL SINUS VENOUS THROMBOSIS” 6 Brief resume of the intended work:
6.1 Need for the study:
. Cerebral venous thrombosis is due to thrombotic occlusion or stenosis in the valveless cerebral venous system, involving larger dural sinuses +/- deep or cortical draining veins.(1)
. It is an important cause of stroke specially in peripartum settings and stroke in young.(2)
. Of all patients with stroke, intracranial venous thrombosis probably accounts for no more than 1 or 2%.(3)
. The age distribution is fairly uniform except that women are affected slightly more than men and mostly between the ages of 20 and 35. This is probably related to pregnancy and oral contraceptives.(4)
. Pregnancy, oral contraceptives, dehydration, hypotension and infections are the most predisposing systemic causes for cerebral
1 venous thrombosis.(5)
. Cerebral venous thrombosis occuring in puerperium is about 10 to 12 times more frequent in India than in western countries. A clinical study of 135 patients with cerebrovascular accidents in early puerperium was conducted in Madurai medical college, Madurai, India. It showed cortical vein thrombosis is common and arterial thrombosis rare (6/135) .The illness usually occurs within the first two weeks, after normal delivery at full term, in a multiparous woman, with multi focal seizures, stupor or coma, regressing focal signs or at times as pseudotumour cerebri.(6)
. Intracranial venous thrombosis appears to have become more common in recent years. However this has occurred as modern imaging techniques have improved diagnosis.(7)
. Functional outcome from cerebral venous thrombosis is better than arterial strokes, the outcome of cerebral venous thrombosis remains unpredictable and may lead to sequelae or even death if not recognised and treated early. (8)
. Hence the present study aims at making a thorough clinical study of cases having the suspicion about the likely diagnosis of cerebral venous thrombosis, to be confirmed by imaging techniques , treat the patient in time and follow up the cases for any sequelae , as the timely approach gives good prognosis.
6.2 Review of literature:
. There are many possible contributory factors and more than one may be present.(9)
Infection from frontal sinus is the commonest. Many different organisms may cause infection but Staphylococcus aureus is the commonest pathogen. Trauma can result in cerebral sinus thrombosis. Pregnancy, dehydration and puerperium are associated with a predisposition to venous thrombosis, including intracranial venous thrombosis.
Hypercoagulable states associated with the antiphospholipid syndrome and thrombophilia including protein S and C deficiencies, antithrombin III
2 deficiency, lupus anticoagulant, and Leiden factor V mutation increase risk. Congenital varieties of thrombophilia account around 15% of cases. Haematological conditions include paroxysmal nocturnal haemoglobinuria, thrombotic thrombocytopenia purpura, sickle cell disease and polycythaemia rubra vera. Vascular diseases include SLE, Wegener's granulomatosis and Behcet's disease. A survey from Saudi Arabia found Behcet's syndrome to be a common aetiological factor.(3)
. Although numerous conditions can cause or predispose to cerebral venous thrombosis the causal factors by which they induce thrombosis may be grouped into a triad of blood disorders leading to a prothrombotic state, venous stasis and direct involvement of venous wall.(10) . The study compared 78 people with cerebral venous thrombosis in Germany to 201 healthy people. Researchers found that a variant of the gene called factor XII C46T is more common in people with cerebral venous thrombosis than in healthy people.(11)
. Cerebral infarction can result from tissue congestion and obstruction. Cerebral haemorrhage may occur with the venous thrombosis and may even be a presenting feature.(7) . Clinical presentations are related to involvement of different parts of the cerebral venous system. Initial symptoms include headache of varying severity and raised intracranial pressure and cerebral venous infarcts, which are frequently hemorrhagic and may lead to seizures, neurologic deficits or even death. Obstruction of the sinuses often causes intracranial hypertension as a result of impaired drainage of the cerebrospinal fluid which may cause papilledema and altered vision. On the other hand sinuses, particularly the lateral sinuses, can be occluded with out any infarcts or intracranial hypertension.(12) . Heparin should be considered seriously in the management of cerebral venous thrombosis. Conversion to warfarin as maintenance therapy is then suggested. Subcutaneous low-molecular-weight heparin (Lovenox) also has been used in patients with venous sinus thrombosis. (13)
. The complications of cerebral venous thrombosis may be divided into the acute stage and those that are associated with the chronic stage of cerebral venous thrombosis. They are venous infarction and haemorrhage, subarachnoid haemorrhage, a rapid progression and pulmonary embolism.
3 In the chronic stages of CVT, dural AV--fistula, progressive psychiatric disease, residual epilepsy and recurrence.(14)
. Location of venous thrombosis is also an important factor because deep cerebral and cerebellar veins thrombosis is associated with a higher mortality than thrombosis of superficial veins. It is also important that cerebral venous thrombosis associated with postpartum has a good prognosis with a 90% survival.(8)
. The mortality of cerebral venous thrombosis ranges between 5% and 15%. (15)
. High plasma concentrations of homocysteine and low plasma folate levels were associated with an increase risk of cerebral venous thrombosis in which low socioeconomic conditions and deficient nutritional status may contribute to its relatively high incidence.(16)
6.3 Aims and objectives of the study:
. To study the clinical profile of cerebral venous thrombosis including the investigations, the treatment and the response of the patient.
. To assess any possible prognostic factors.
Materials and methods:
7 7.1 Source of data:
Cases for the study will be sourced from admissions to Bapuji Hospital, Chigateri Hospital attached to J.J.M. Medical College, Davangere.
7.2 Method of data collection:
. A minimum number of 50 patients admitted in hospital during the study period who has clinical and CT features [direct and indirect] suggestive of cerebral sinus venous thrombosis will be selected.
4 . The period of study is from November 2008 to November 2010.
. A prestructured Proforma will be used to collect all the relevant data from the patients.
. All patients selected will be subjected to detailed history, clinical examination and investigated.
Inclusion criteria :
. All patients aged >18yrs . An acute or subacute neurological illness in a patient under appropriate clinical condition whose CT features [direct and indirect] are suggestive of cerebral venous thrombosis. . The examination should have suggested constellation of signs of raised ICT/ neurological deficits/ seizures.
Exclusion criteria : . Patients <18yrs . Stroke due to arterial thrombosis, haemorrhage and patients with intra cranial space occupying lesion.
7.3 Does the study require any investigations or interventions to be conducted on patients, other humans or animals? If so, please describe briefly.
YES
. Complete blood picture . Blood sugar . Blood urea . Serum creatinine . CSF Analysis [where ever deemed necessary] . Serology for HIV 1 & 2 . Urine culture and sensitivity . Computed tomography [CT] scan
7.4 Has ethical clearance been obtained from your institution in case of 7.3?
YES.
5 References :
8 1. Bousser M.G. Cerebral venous thrombosis: diagnosis and management. Journal of Neurology 2000;247:252-258.
2 . Gijn,J.Van. Stroke. In:David A .Warell, Timothy M. Cox, John D. Firth, Edward J.Benz Jr . 4 th. Oxford textbook of medicine:New York:2003;vol [3]:1029.
3 . Daif A, Awada A, al-Rajeh S; Cerebral venous thrombosis in adults. A study of 40 cases from Saudi Arabia. Stroke. 1995 July;26(7):1193-5.
4 . de Bruijn S.F, Stam J, Vandenbroucke J.P; Increased risk of cerebral venous sinus thrombosis with third-generation oral contraceptives. Cerebral Venous Sinus Thrombosis Study Group. Lancet. 1998 May 9;351(9113):1404.
5. Allen C.M.C, Lueck C.J, Dennis M. Neurological diseases. Nicholas A.Boon, Nicki R.Colledge, Brain R.Walker, John A.A.Hunter. Davidson’s Principles and Practice of Medicine.20th edition 2006:1211-1212.
6 . Kalita J, Bansal V, Misra U.K. Cerebral venous sinus thrombosis in a teritary care setting in India. QJM, July 1,2006;99[7]:491-492.
7 . McElveen W; Cerebral Venous Thrombosis. eMedicine, Oct 2006.
8 . Ferro J.M.M, Canhao P, Stam J. Prognosis of cerebral vein and dural sinus thrombosis: results of international study on cerebral vein and dural sinus thrombosis [ISCVT]. Stroke 2004;335:664-670.
9 . Deschiens M.A, Conard J, Horellou M.H.Coagulation studies, factor V Leiden, and anticardiolipin antibodies in 40 cases of cerebral venous thrombosis. Stroke. 1996 Oct;27(10):1724-30.
10 . Enevoblson T, Ross Russel R.W. Cerebral venous thrombosis. New causes for an old syndrome?.QJ Med 1999;289:1255-1275.
11 . Reuner K.H . Factor XII C46T gene polymorphism and the risk of cerebral venous thrombosis. Neurology 2008 Jan 8; 70:129.
12 . Daif A, Awada A. Cerebral venous thrombosis in adults. Stroke
6 1995;26:1193-1195.
13 . Einhaupl K.M, Villringer A, Meister W. Heparin treatment in sinus venous thrombosis.Lancet. Sep 7 1991;338(8767):597-600
14 . Siddique F.M, Kamal A.K. Complications associated with cerebral venous thrombosis. J Pak Med Assoc.2006 Nov;56(11):547-551.
15 . Conoor S.E.J, Jarosz J.M. Magnetic resonance imaging of cerebral venous sinus thrombosis. Clinical Radiology 2002;57:449-461.
16 . Carlos Cantu, Elisa Alonso, Aurelio Jara. Hyperhomocysteinemia, low folate and vitamin B12 concentrations and methylene tetrahydrofolate reductase mutations in cerebral venous thrombosis. Stroke 2004;35:1790- 1794.
9. Signature of the Candidate 10. Remarks of the Cerebral venous thrombosis is one among many causes g Guide of stroke in young patients specially the female patients in peripartum period. Patients may have neurological deficits, may come with history of convulsions and they may be admitted with altered consciousness. The condition needs to be differentiated from other common conditions giving rise to similar clinical symptoms eg: arterial infarcts, meningitis, encephalitis, brain abscess etc. Cerebral venous thrombosis if suspected early , if the patient is investigated promptly and if treatment is started early in the course of the disease, they respond very well without leaving any deficits behind. Because of this better outcome, there is a need to study the suspected cases in detail clinically, supported by relevant investigations particularly CT scan of brain to confirm the diagnosis, to start the treatment promptly and to follow the response of the patient.
7 11. 11.1 Guide DR. B D CHAVAN M.D Name and PROFFESOR de designation (in GENERAL MEDICINE b block letters) J. J. M. MEDICAL COLLEGE, DAVANGERE – 577004
11.2 Signature
11.3 Co guide (if any) None
11.4 Signature
11.5 Head of Department DR. P M UPASI M.D PROFFESOR & HEAD OF DEPARTMENT GENERAL MEDICINE J. J. M. MEDICAL COLLEGE, DAVANGERE – 577004 11.6 Signature
12. 12.1 Remarks of the Chairman & pri Principal
12.2 Signature
8