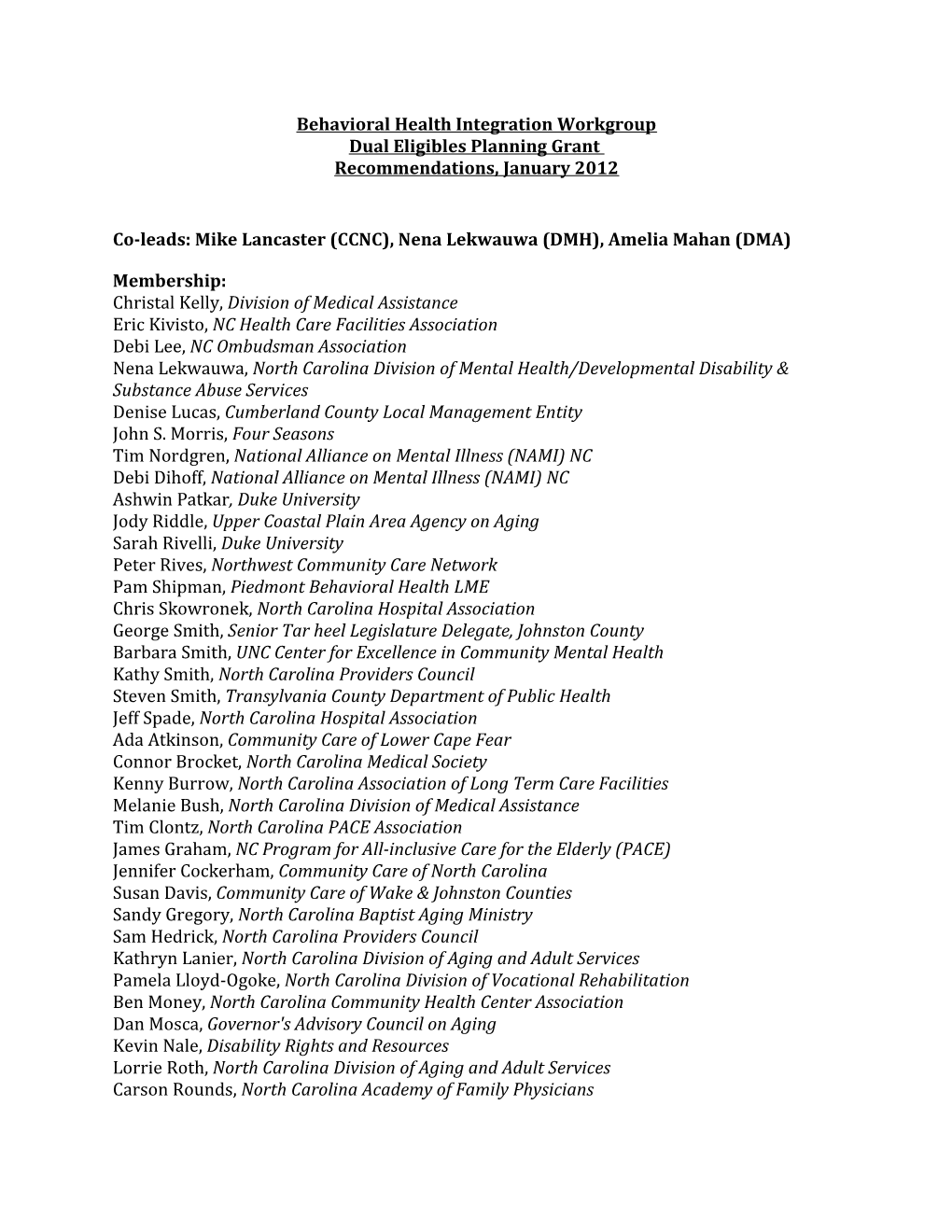
Behavioral Health Integration Workgroup Dual Eligibles Planning Grant Recommendations, January 2012
Co-leads: Mike Lancaster (CCNC), Nena Lekwauwa (DMH), Amelia Mahan (DMA)
Membership: Christal Kelly, Division of Medical Assistance Eric Kivisto, NC Health Care Facilities Association Debi Lee, NC Ombudsman Association Nena Lekwauwa, North Carolina Division of Mental Health/Developmental Disability & Substance Abuse Services Denise Lucas, Cumberland County Local Management Entity John S. Morris, Four Seasons Tim Nordgren, National Alliance on Mental Illness (NAMI) NC Debi Dihoff, National Alliance on Mental Illness (NAMI) NC Ashwin Patkar, Duke University Jody Riddle, Upper Coastal Plain Area Agency on Aging Sarah Rivelli, Duke University Peter Rives, Northwest Community Care Network Pam Shipman, Piedmont Behavioral Health LME Chris Skowronek, North Carolina Hospital Association George Smith, Senior Tar heel Legislature Delegate, Johnston County Barbara Smith, UNC Center for Excellence in Community Mental Health Kathy Smith, North Carolina Providers Council Steven Smith, Transylvania County Department of Public Health Jeff Spade, North Carolina Hospital Association Ada Atkinson, Community Care of Lower Cape Fear Connor Brocket, North Carolina Medical Society Kenny Burrow, North Carolina Association of Long Term Care Facilities Melanie Bush, North Carolina Division of Medical Assistance Tim Clontz, North Carolina PACE Association James Graham, NC Program for All-inclusive Care for the Elderly (PACE) Jennifer Cockerham, Community Care of North Carolina Susan Davis, Community Care of Wake & Johnston Counties Sandy Gregory, North Carolina Baptist Aging Ministry Sam Hedrick, North Carolina Providers Council Kathryn Lanier, North Carolina Division of Aging and Adult Services Pamela Lloyd-Ogoke, North Carolina Division of Vocational Rehabilitation Ben Money, North Carolina Community Health Center Association Dan Mosca, Governor's Advisory Council on Aging Kevin Nale, Disability Rights and Resources Lorrie Roth, North Carolina Division of Aging and Adult Services Carson Rounds, North Carolina Academy of Family Physicians Janet Schanzenbach, North Carolina Association of Long Term Care Facilities Don Herring, Western Highlands Network Amy Whited, North Carolina Medical Society Peggy Balak, Saguaro Group LLC/ Triumph Regina Dickens, North Carolina Foundation of Advanced Health Programs Susan Osborne, North Carolina Association of County Directors of Social Services Emery Cowan, North Carolina Division of Mental Health/Developmental Disability & Substance Abuse Services Heather Brewer, Easter Seals UCP of NC & VA, Inc Laurie Cocker, NC Consumer Advocacy, Networking, and Support Organization (NC CANSO Marc Jacques, Consumer
Charge for the Workgroup: Explore current practices in behavioral health care in the State and identify opportunities for better integration and delivery of supports and services
Explore integration of behavioral health and physical health services, as well as the risk sharing for behavioral health services and supports Explore medical home and related supports for adult care home residents Define communication, care coordination and accountability strategies to support integrated care Define processes and components of integration desired in the new delivery system
STRATEGIC FRAMEWORK/OVERARCHING POLICY:
The Behavioral Health Workgroup believes that improving access to integrated care that is recovery-focused for dual eligibles may lead to short-term increases in cost but will lead to long-term savings and a healthier population. We believe that North Carolina has the infrastructure necessary and that we can build on the existing health home model and utilize and expand peer support options.
A. Recommendations for immediate implementation:
1) Streamline the billing process to make it more efficient – a) Ensure providers are paid in a timely fashion, b) For services that Medicare does not cover, providers should be able to submit claims directly to Medicaid without having to first get a denial from Medicare. This recommendation, if implemented will increase access, as more providers would be willing to accept Medicare/Medicaid. 2) Create a state-wide repository of original credentialing documents Providers can submit the credentialing documents once and then the credentialing agencies can get the information from the repository. This has been done before in NC and could be done again.
3) Better integrate with existing Gero-teams and expand if needed into the health home.
4) Build on existing centralized resource lines and resource centers to provide a single outlet for information Ensure that those answering the phones and those working there have up-to- date information on dual benefits and resources as well as behavioral health- specific resources. This could be done locally, but it would also be useful to have a statewide resource number/webpage.
5) Build on existing care coordination/care management models – Expand focus to include “Integrated Care Coordinators” with smaller caseloads who work specifically with the dual eligible population with BH diagnosis. Care coordinators should be cross-trained and should have access to specialists for consultation.
6) Increase and encourage collocation and reverse collocation between primary care and specialty behavioral health.
B. Recommendations for mid to longer term implementation
1) Development of a flexible system that allows individuals to engage in services based on their needs and allows them to move through the system without fear of losing their benefits (allows them to work, engage in recovery, etc.).
2) System should include social needs in addition to healthcare needs (housing, transportation, etc.) which will greatly reduce healthcare costs long-term and will improve quality of life for the dual population.
3) Focus on Recovery Education Centers that allow for walk-ins for a recipient, regardless of what phase of recovery that they are in – could be peer-operated wellness center that utilizes peer wellness/health coaches.
C. PARKING LOT
1) In order to increase access to care, increase the number of providers who can serve dual eligibles. Align Medicare credentials which are limited to LCSWs and psychologists, to Medicaid credentials which can include LPCs, LMFTs, LCASs, etc. Particularly in rural areas, it can be very difficult to find the providers who are able to work with duals because of the Medicare restrictions. 2) As NC moves behavioral health services into a 1915 b/c waiver environment where multiple LME/MCO/PHPs are going to be managing behavioral health services for Medicaid recipients, continuous efforts will need to be made to ensure that the behavioral health and the physical health sides are collaborating with one another to ensure that the dual eligible population is receiving the right services at the right time in the most effective way possible.
Items to send to other groups: 1) Finance group needs to look at the ‘streamlining the billing process’ recommendation. 2) The Behavioral Health Workgroup felt strongly that there needs to be a “no wrong door” policy for duals to receive a comprehensive assessment and enter services.
Who will do the assessment and what type of assessment needs to be done that will capture the person’s physical and behavioral health needs to be determined. Members of the Behavioral Health Workgroup are willing to work with the Needs Determination/Assessment Workgroup.