Blue Preferred® Rx Prescription Drug Coverage with $15 / $50 50% / $70 minimum / $100 maximum / Nonformulary Brand Name Triple-Tier Copay Open Formulary Benefits-at-a-Glance for Midland County ESA #48292-006, 009
This is intended as an easy-to-read summary and provides only a general overview of your benefits. It is not a contract. Additional limitations and exclusions may apply to covered services. For a complete description of benefits, please see the applicable Blue Cross Blue Shield of Michigan certificates and riders. Payment amounts are based on the Blue Cross Blue Shield of Michigan approved amount, less any applicable deductible and/or copay amounts required by your plan. This coverage is provided pursuant to a contract entered into in the state of Michigan and will be construed under the jurisdiction of and according to the laws of the state of Michigan.
Specialty Drugs – The mail order pharmacy for specialty drugs is Walgreens Specialty Pharmacy, LLC, an independent company. Specialty ® ® prescription drugs (such as Enbrel and Humira ) are used to treat complex conditions such as rheumatoid arthritis. These drugs require special handling, administration or monitoring. Walgreens Specialty Pharmacy will handle mail order prescriptions only for specialty drugs while many retail pharmacies will continue to dispense specialty drugs (check with your local pharmacy for availability). Other mail order prescription medications can continue to be sent to Medco. (Medco is an independent company providing pharmacy benefit services for Blues members.) A list of specialty drugs is available on our Web site at bcbsm.com. Log in under “I am a Member.” If you have any questions, please call Walgreens Specialty Pharmacy customer service at 1-866-515-1355. BCBSM reserves the right to limit the initial quantity of select specialty drugs. Your copay will be reduced by one-half for this initial fill (15 days).
If you are enrolled in one of our integrated medical-surgical prescription drug products, your prescription drug benefits, including mail order drugs, are subject to the same deductible and lifetime dollar maximum required under your medical-surgical coverage. Benefits are not payable until after you have met the annual deductible. After you have satisfied the deductible you are required to pay the copays listed below, which may be limited to an annual out-of-pocket maximum.
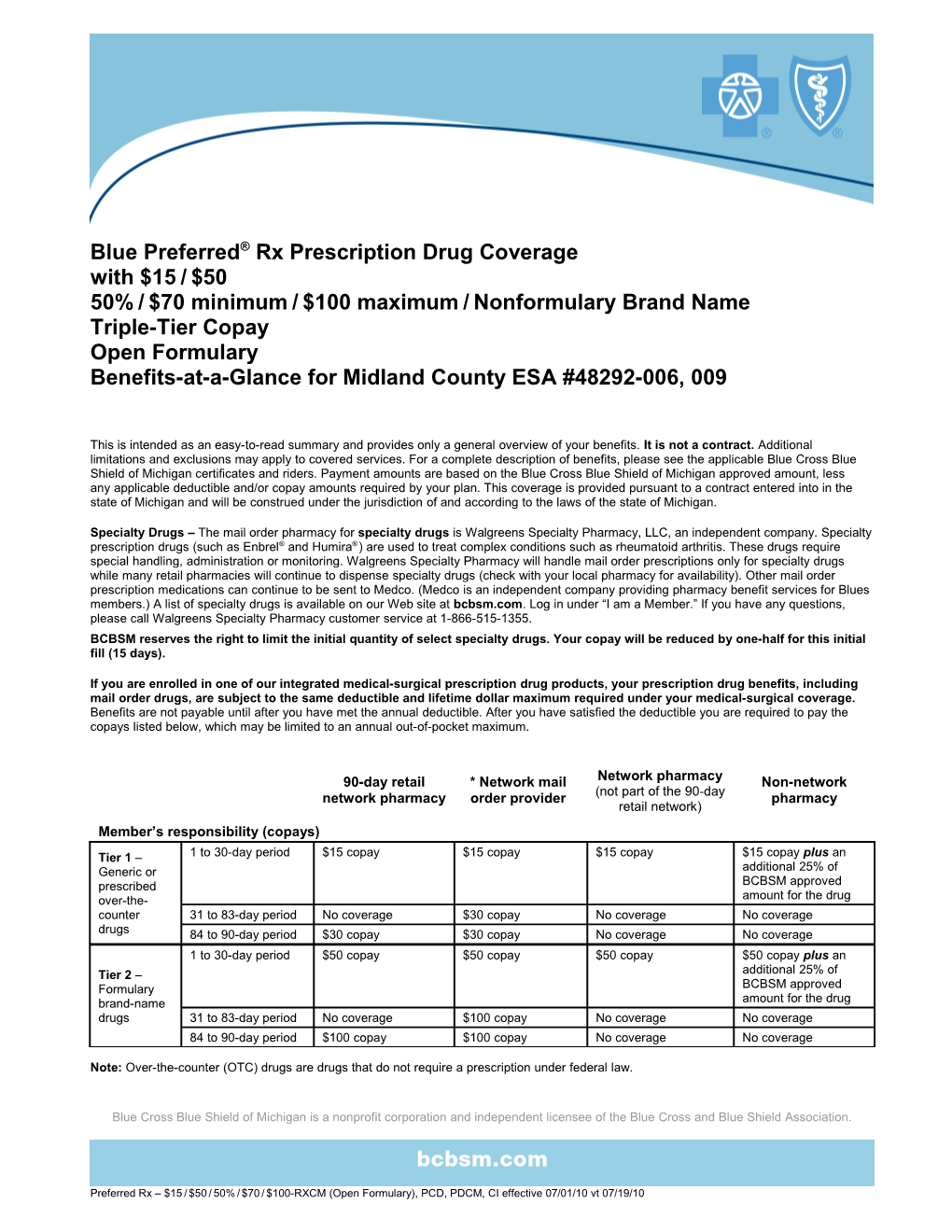
90-day retail * Network mail Network pharmacy Non-network network pharmacy order provider (not part of the 90-day pharmacy retail network) Member’s responsibility (copays)
Tier 1 – 1 to 30-day period $15 copay $15 copay $15 copay $15 copay plus an Generic or additional 25% of prescribed BCBSM approved over-the- amount for the drug counter 31 to 83-day period No coverage $30 copay No coverage No coverage drugs 84 to 90-day period $30 copay $30 copay No coverage No coverage 1 to 30-day period $50 copay $50 copay $50 copay $50 copay plus an Tier 2 – additional 25% of Formulary BCBSM approved brand-name amount for the drug drugs 31 to 83-day period No coverage $100 copay No coverage No coverage 84 to 90-day period $100 copay $100 copay No coverage No coverage
Note: Over-the-counter (OTC) drugs are drugs that do not require a prescription under federal law.
Blue Cross Blue Shield of Michigan is a nonprofit corporation and independent licensee of the Blue Cross and Blue Shield Association.
Preferred Rx – $15 / $50 / 50% / $70 / $100-RXCM (Open Formulary), PCD, PDCM, CI effective 07/01/10 vt 07/19/10 90-day retail * Network mail Network pharmacy Non-network network pharmacy order provider (not part of the 90-day pharmacy retail network) Member’s responsibility (copays), continued 1 to 30-day period $70 or 50% of the $70 or 50% of the $70 or 50% of the $70 or 50% of the approved amount approved amount approved amount approved amount (whichever is greater), (whichever is (whichever is greater), (whichever is greater), but no more than $100 greater), but no but no more than but no more than $100 more than $100 $100 plus an additional 25% of BCBSM approved amount for the drug Tier 3 – 31 to 83-day period No coverage $140 or 50% of the No coverage No coverage Nonformulary approved amount brand-name (whichever is drugs greater), but no more than $200 84 to 90-day period $140 or 50% of the $140 or 50% of the No coverage No coverage approved amount approved amount (whichever is greater), (whichever is but no more than $200 greater), but no more than $200 Covered services FDA-approved drugs 100% of approved 100% of approved 100% of approved 75% of approved amount less plan amount less plan amount less plan amount less plan copay copay copay copay Prescribed over-the-counter drugs – 100% of approved 100% of approved 100% of approved 75% of approved when covered by BCBSM amount less plan amount less plan amount less plan amount less plan copay copay copay copay State-controlled drugs 100% of approved 100% of approved 100% of approved 75% of approved amount less plan amount less plan amount less plan amount less plan copay copay copay copay Disposable needles and syringes – 100% of approved 100% of approved 100% of approved 75% of approved when dispensed with insulin or other amount less plan amount less plan amount less plan amount less plan copay covered injectable legend drugs copay for the insulin or copay for the insulin copay for the insulin for the insulin or other Note: Needles and syringes have no other covered or other covered or other covered covered injectable copay. injectable legend drug injectable legend injectable legend drug legend drug drug
* Note: BCBSM will not pay for drugs obtained from non-network mail order providers, including Internet providers.
Preferred Rx – $15 / $50 / 50% / $70 / $100-RXCM (Open Formulary), PCD, PDCM, CI effective 07/01/10 vt 07/19/10 Features of your prescription drug plan Mandatory preauthorization A process that requires a physician to obtain approval from BCBSM before select prescription drugs (drugs identified by BCBSM as requiring preauthorization) will be covered. Step Therapy, an initial step in the “Prior Authorization” process, applies criteria to select drugs to determine if a less costly prescription drug may be used for the same drug therapy. Some over-the-counter medications may be covered under step therapy guidelines. This also applies to mail order drugs. Claims that do not meet Step Therapy criteria require preauthorization. Details about which drugs require preauthorization or step therapy are available online site at bcbsm.com. Log in under “I am a Member” and click on “Prescription Drugs.” Mandatory maximum allowable If your prescription is filled by any type of network pharmacy, and the pharmacist fills it with a generic cost (MAC) drugs equivalent drug, you pay only the copay. If you obtain a formulary brand name drug when a generic equivalent drug is available, you MUST pay the difference in cost between the formulary brand name drug dispensed and the maximum allowable cost for the generic drug plus your copay regardless of whether you or your doctor requests the formulary brand name drug. If you obtain a nonformulary brand-name drug when a generic equivalent is available, the nonformulary brand-name drug is not a covered benefit. Exception: If your physician requests and receives authorization for a nonformulary brand-name drug with a generic equivalent from BCBSM and writes “Dispense as Written” or “DAW” on the prescription order, you pay only your applicable copay. Physician-administered Injectable drugs administered by a health care professional (not self-administered) are not covered injectable drugs under the pharmacy benefit, but may be covered under your medical benefit. Drug interchange and Certain drugs may not be covered for future prescriptions if a suitable alternate drug is identified by generic copay waiver BCBSM, unless the prescribing physician demonstrates that the drug is medically necessary. A list of drugs that may require authorization is available at bcbsm.com. If your physician rewrites your prescription for the recommended generic or OTC alternate drug, you will only have to pay a generic copay. If your physician rewrites your prescription for the recommended brand-name alternate drug, you will have to pay a brand-name copay. In select cases BCBSM may waive the initial copay after your prescription has been rewritten. BCBSM will notify you if you are eligible for a waiver. Quantity limits Select drugs may have limitations related to quantity and doses allowed per prescription unless the prescribing physician obtains preauthorization from BCBSM. A list of these drugs is available at bcbsm.com.
Additional riders Rider CI, contraceptive injections Adds coverage for contraceptive injections, physician-prescribed contraceptive devices such as Rider PCD, prescription diaphragms and IUDs, and FDA-approved oral, or self-injectable contraceptive medications as contraceptive devices identified by BCBSM (non-self-administered drugs and devices are not covered). Rider PD-CM, prescription Note: These riders are only available as part of a prescription drug package. contraceptive medications Riders CI and PCD are part of your medical-surgical coverage, subject to the same deductible and copay, if any, you pay for medical-surgical services. (Rider PCD waives the copay for services provided by a network provider.) Rider PD-CM is part of your prescription drug coverage, subject to the same copay you pay for prescription drugs.
Preferred Rx – $15 / $50 / 50% / $70 / $100-RXCM (Open Formulary), PCD, PDCM, CI effective 07/01/10 vt 07/19/10