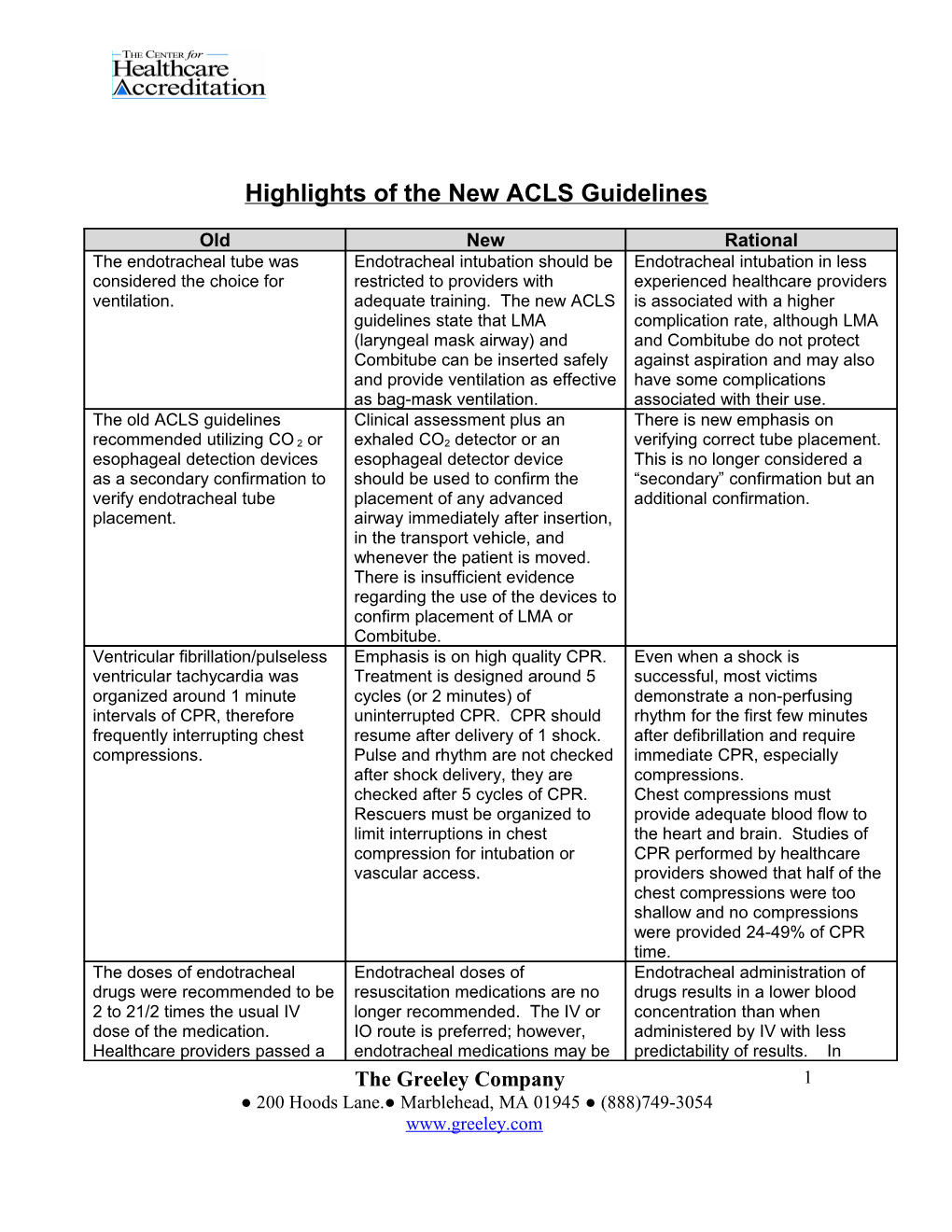
Highlights of the New ACLS Guidelines
Old New Rational The endotracheal tube was Endotracheal intubation should be Endotracheal intubation in less considered the choice for restricted to providers with experienced healthcare providers ventilation. adequate training. The new ACLS is associated with a higher guidelines state that LMA complication rate, although LMA (laryngeal mask airway) and and Combitube do not protect Combitube can be inserted safely against aspiration and may also and provide ventilation as effective have some complications as bag-mask ventilation. associated with their use. The old ACLS guidelines Clinical assessment plus an There is new emphasis on recommended utilizing CO 2 or exhaled CO2 detector or an verifying correct tube placement. esophageal detection devices esophageal detector device This is no longer considered a as a secondary confirmation to should be used to confirm the “secondary” confirmation but an verify endotracheal tube placement of any advanced additional confirmation. placement. airway immediately after insertion, in the transport vehicle, and whenever the patient is moved. There is insufficient evidence regarding the use of the devices to confirm placement of LMA or Combitube. Ventricular fibrillation/pulseless Emphasis is on high quality CPR. Even when a shock is ventricular tachycardia was Treatment is designed around 5 successful, most victims organized around 1 minute cycles (or 2 minutes) of demonstrate a non-perfusing intervals of CPR, therefore uninterrupted CPR. CPR should rhythm for the first few minutes frequently interrupting chest resume after delivery of 1 shock. after defibrillation and require compressions. Pulse and rhythm are not checked immediate CPR, especially after shock delivery, they are compressions. checked after 5 cycles of CPR. Chest compressions must Rescuers must be organized to provide adequate blood flow to limit interruptions in chest the heart and brain. Studies of compression for intubation or CPR performed by healthcare vascular access. providers showed that half of the chest compressions were too shallow and no compressions were provided 24-49% of CPR time. The doses of endotracheal Endotracheal doses of Endotracheal administration of drugs were recommended to be resuscitation medications are no drugs results in a lower blood 2 to 21/2 times the usual IV longer recommended. The IV or concentration than when dose of the medication. IO route is preferred; however, administered by IV with less Healthcare providers passed a endotracheal medications may be predictability of results. In The Greeley Company 1 ● 200 Hoods Lane.● Marblehead, MA 01945 ● (888)749-3054 www.greeley.com Old New Rational catheter beyond the tip of the used if there is no IV or IO access. addition, epinephrine endotracheal tube, stopped The dose of endotracheal drugs administered by endotracheal compressions to inject the drug, are still generally 2 to 21/2 times route may produce detrimental followed with several quick the usual IV dose. effects causing hypotension, ventilations, and then resumed lower coronary artery perfusion CPR. and reduced potential for the return of spontaneous circulation. During pulseless arrest, dugs When drugs are indicated during These recommendations were administered in a drug- pulseless arrest, they should be minimize interruptions in chest CPR-shock cycle immediately administered during CPR; the compressions. Administering the after a rhythm check. Rhythm administration should not interrupt drugs after a rhythm check checks were performed about CPR. Drugs should be allows the rescuers to treat the every minute during administered as soon as possible rhythm seen at the rhythm check. resuscitation, resulting in after a rhythm check, therefore, frequent interruptions of CPR. require some advanced preparation to avoid delays. This scenario does require organization and planning. Epinephrine or vasopressin Vasopressors are administered Vasopressin has not shown could be given for ventricular when an IV or IO line is in place, improved rates of survival to fibrillation/pulseless ventricular generally after the first or second discharge; therefore, a single tachycardia. For asystole/PEA, shock. Epinephrine may be given dose may be used as an epinephrine was recommended. every 3 to 5 minutes. One dose of alternative to the first or second vasopressin may be given instead dose of epinephrine. of the first or second dose of epinephrine. If VF/VT persists after When VF or pulseless VT There is more documentation on defibrillation and a vasopressor, continues after 2 or 3 the effectiveness of amiodarone. consider using amiodarone or defibrillations plus CPR and a lidocaine. vasopressor, consider using amiodarone. Lidocaine is used only if amiodarone is unavailable. For asystole or PEA, 1 mg of Epinephrine 1 mg IV or IO can be Vasopressors can improve aortic epinephrine was recommended given every 3 to 5 minutes for blood pressure and coronary every 3 to 5 minutes. Atropine asystole or PEA. One dose of artery perfusion pressure; was considered for asystole or vasopressin (40 Units IV or IO) however, vasopressors have not slow PEA every 3 to 5 minutes may be substituted for the first or been shown to improve survival as needed, up to 0.04 mg/kg. second dose of epinephrine. from cardiac arrest. Atropine (1 mg IV or IO) may still be considered for asystole or slow PEA, up to 3 doses. For symptomatic bradycardia, The treatment of choice for a high- Studies showed that an effective the range of atropine dosing degree block is transcutaneous dose of atropine for symptomatic was 0.5mg to 1 mg IV. pacing. Atropine 0.5 mg may also bradycardia is 0.5mg. dopamine, epinephrine or be used while waiting for the Isoproterenol was eliminated The Greeley Company 2 ● 200 Hoods Lane.● Marblehead, MA 01945 ● (888)749-3054 www.greeley.com Old New Rational isoproterenol could also be pacer. Atropine may be repeated from the algorithm because there considered. up to 3 mg. Epinephrine infusion was no documentation of its or a dopamine infusion may also efficacy. be used while preparing for the pacemaker and if pacing is ineffective. Tachycardia algorithms divided Immediate synchronized The goal was to simplify therapy. treatments into patients with cardioversion is still recommended adequate ventricular function for the unstable patients. For the and those with poor ventricular stable patient, there are ejection fraction. algorithms for tachycardia with narrow or wide complexes, and regular or irregular rhythms. It was thought that mild Unconscious adult patients with In 2 randomized clinical trials, hypothermia might be beneficial ROSC (return of spontaneous induced hypothermia (within after a cardiac arrest; however, circulation) after out-of-hospital minutes to hours after ROSC) it should not be actively cardiac arrest should be cooled to resulted in improved survival and induced. 32 degrees C for 12 to 24 hours neurological outcome in adults when the initial rhythm was VF. who remained comatose after Similar benefit may be seen in initial resuscitation after out-of- patients with non-VF cardiac hospital VF cardiac arrest. arrest out-of-hospital arrest or for in hospital arrest. Further research is needed. No specific neurological signs Post resuscitation care may A meta-analysis of 11 studies were noted to be prognostic. include vasoactive support, documented that the 5 clinical glucose control, and a period of signs strongly predicted death or hypothermia. poor neurological outcome. A Clinical signs that strongly meta-analysis also demonstrated correlate with death or poor that bilateral absence of cortical neurological outcome include: response to median nerve -Bilateral absence of cortical somatosensory-evoked response to median nerve potentials predicted poor somatosensory-evoked potentials outcome with 100% specificity measured 72 hours after hypoxic- when used in patients that were ischemia (asphyxial) insult in the comatose for at least 72 hours normothermic patient and were normothermic. -Absent corneal reflex at 24 hours -Absent pupillary response to pain at 24 hours -Absent withdrawal response to pain at 24 hours -No motor response at 24 hours -No motor response at 72 hours
The Greeley Company 3 ● 200 Hoods Lane.● Marblehead, MA 01945 ● (888)749-3054 www.greeley.com