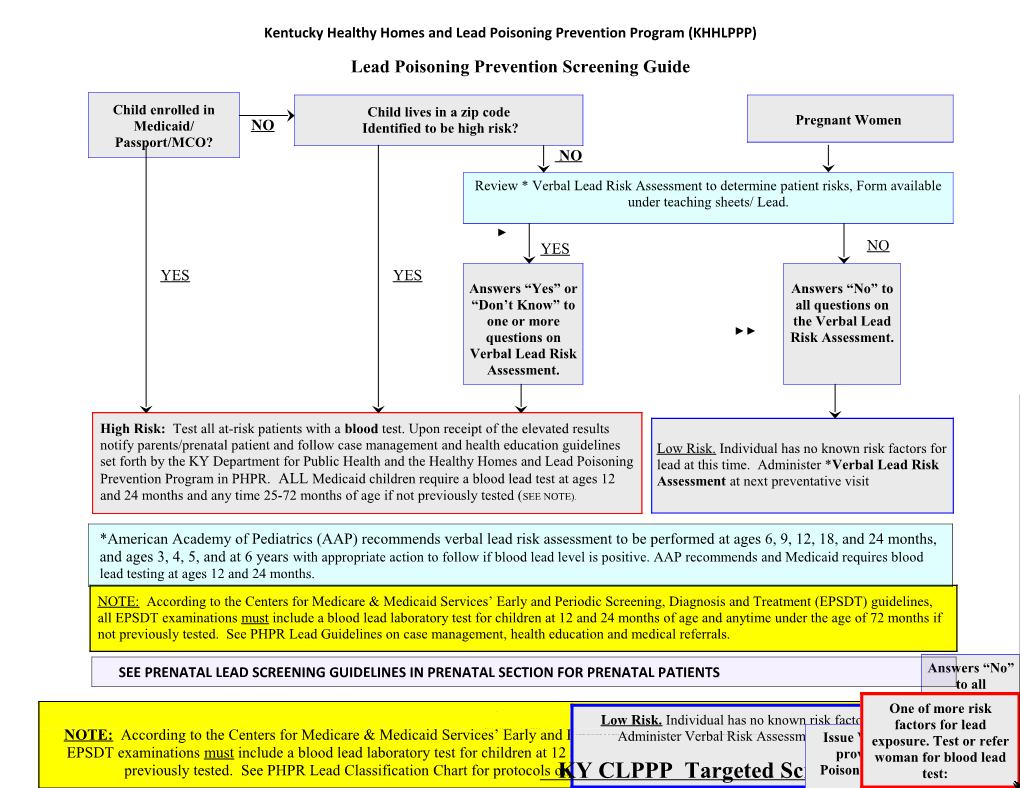
Kentucky Healthy Homes and Lead Poisoning Prevention Program (KHHLPPP) Lead Poisoning Prevention Screening Guide
Child enrolled in Child lives in a zip code Pregnant Women Medicaid/ NO Identified to be high risk? Passport/MCO? NO
Review * Verbal Lead Risk Assessment to determine patient risks, Form available under teaching sheets/ Lead.
YES NO YES YES Answers “Yes” or Answers “No” to “Don’t Know” to all questions on one or more the Verbal Lead questions on Risk Assessment. Verbal Lead Risk Assessment.
High Risk: Test all at-risk patients with a blood test. Upon receipt of the elevated results notify parents/prenatal patient and follow case management and health education guidelines Low Risk. Individual has no known risk factors for set forth by the KY Department for Public Health and the Healthy Homes and Lead Poisoning lead at this time. Administer *Verbal Lead Risk Prevention Program in PHPR. ALL Medicaid children require a blood lead test at ages 12 Assessment at next preventative visit and 24 months and any time 25-72 months of age if not previously tested (SEE NOTE).
*American Academy of Pediatrics (AAP) recommends verbal lead risk assessment to be performed at ages 6, 9, 12, 18, and 24 months, and ages 3, 4, 5, and at 6 years with appropriate action to follow if blood lead level is positive. AAP recommends and Medicaid requires blood lead testing at ages 12 and 24 months. NOTE: According to the Centers for Medicare & Medicaid Services’ Early and Periodic Screening, Diagnosis and Treatment (EPSDT) guidelines, all EPSDT examinations must include a blood lead laboratory test for children at 12 and 24 months of age and anytime under the age of 72 months if not previously tested. See PHPR Lead Guidelines on case management, health education and medical referrals.
SEE PRENATAL LEAD SCREENING GUIDELINES IN PRENATAL SECTION FOR PRENATAL PATIENTS AnswersAnswers “No” “Yes”to all or “Don’tquestions Know” on Page 1 of 18 One of more risk Kentucky Public Health Practice Reference to theone Verbal or more Section: LeadTest child atLow age Risk. 12 and Individual 24 months has of no age known and any risk time factors under for the factorslead age at of thisfor 72 leadtime. months questionsRisk on NOTE: According to the Centers for Medicare & Medicaid Services’January Early 31, 2012if and not PeriodicpreviouslyAdminister Screening, tested. Upon Verbal Diagnosis receipt Risk of Assessmentand the Treatment resultsIssueIssue atnotify nextVerbal (EPSDT) Verbal parentspreventativeexposure. Risk Risk andguidelines Assessment TestAssessmentfollow visit. or case allrefer ChildChildPregnant lives enrolled in awomanVerbalAssessment. zipin Medicaid code Risk EPSDT examinations must include a blood lead laboratory test for children atmanagement 12 and 24 andmonths health of education age and anytimeguidelines underprovided set forth theprovided bybyage thethe ofwoman KY KY 72by Department months theLead for KY blood Poisoning ifLead not forlead identifiedor to Passport? be Assessment.high risk?YES previously tested. See PHPR Lead Classification Chart for protocols onKYPublic case CLPPP management,Health and the Targeted healthChildhood education Lead Screening Poisoning and PoisoningmedicalPrevention Prevention referrals. PreventionGuide Program Program.test: Program YESNO Kentucky Healthy Homes and Lead Poisoning Prevention Program (KHHLPPP)
GUIDELINES FOR BLOOD LEAD LEVELS (BLL) AND FOLLOW-UP d a BLOOD LEAD LEVEL ASSESSMENT INTERVENTIONS FOLLOW-UP e L d Annual blood lead test o o l Less than 10 µg/dL Not considered lead Continue to review risk assessment questions at once a positive risk factor is B 0-9.9µg/dL poisoning each preventive health visit up to 6 years of age identified. (No amount of lead in the Complete routine blood lead testing for at-risk Retest at next periodicity body is normal. Even low patients (Medicaid, Targeted Zip Code areas, and “+” visit if risk factor changes blood lead levels can cause or “don’t know” verbal lead risk assessment Medicaid recipients or adverse neurological responses) Assure blood lead testing at 12 and children who reside in a effects such as loss of IQ 24 months on all Medicaid recipients/ and at-risk targeted screening area: points and learning children who live in a targeted screening area or 1. Routine blood lead level disabilities. It is very have positive risk factors. obtained at 12 and 24 important that education Parent education pamphlets months of age. on ways to prevent lead Refer for WIC services 2. Blood lead level obtained poisoning begin at this Contact State HHLPPP NCI if you have questions on all children 25 level) months–6 years of age who have never been screened.
10–14.9 µg/dL Level of concern Parent education pamphlets Repeat blood lead level in 12 Send completed report form form if 2nd level in the weeks of the initial, if BLL is 1st specimen at this level 12 weeks is >10µg/dL to HHLPPP NCI still in this range repeat every Refer for WIC services 12 weeks until blood lead Home Visits: level is < 10 µg/dL. If 1st specimen at this level a home visit and visual Establish a tracking system investigation may be made that assures retesting. *If 2nd BLL remains at this level a home visit and Case management. visual investigation must be made within 30 days of 2nd EBLL result. Contact State HHLPPP NCI if you have questions
Page 2 of 18 Kentucky Public Health Practice Reference Section: Lead January 31, 2012 Kentucky Healthy Homes and Lead Poisoning Prevention Program (KHHLPPP)
GUIDELINES FOR BLOOD LEAD LEVELS AND FOLLOW-UP
* SEE PRENATAL LEAD SCREENING GUIDELINES IN PRENATAL SECTION FOR PRENATAL PATIENTS
BLOOD LEAD LEVEL ASSESSMENT INTERVENTIONS FOLLOW-UP
Lead Poisoning Parent education pamphlets 1. Submit confirmation (see 15–29.9µg/dL >15µg/dL Contact state HHLPPP NCI if guidance needed assessment criteria) specimen within one week Venous Specimens are Once Lead Poisoning is Confirmed: 2. Repeat blood lead levels at uncontaminated, preferred Refer for Medical Nutrition Therapy and WIC 1–2 month intervals until: and considered confirmation services. a. Blood lead level is less Refer to a primary care provider (PCP) for than 10µg/dL for 6 months First capillary specimen at medical evaluation. Provide PCP with b. or as s ordered by the this level will need to be letter/information on lead specialist consult. physician confirmed. Initial home visit to be made within 1 week. 3. Establish a tracking system nd 2 Capillary is acceptable; Visual investigation to be made within 1 week of that assures retesting and however, special care is LHD receiving confirmed EBLL results case management nd needed when using a 2 Refer to a *Certified Risk Assessor to perform a 4. For medical case closure see capillary specimen as a lead risk assessment within 2 weeks of LHD case closure section confirmation for lead receiving confirmed EBLL results. *Contact KY 5. Environmental: Lead hazards poisoning. HHLPPP if your HD does not have a Certified have been addressed. Risk Assessor Environmental: Lead Risk Assessment to be 30-44.9µg/dL Lead Poisoning completed within 30 days of Risk Assessor Same as above >15µg/dL receiving referral from LHD, ‘Contact HHLPPP for A VENOUS Environmental Management for EBLL’s guidance, specimen is Mail or fax report to HHLPPP NCI needed to confirm a diagnosis of lead poisoning at this level.
Page 3 of 18 Kentucky Public Health Practice Reference Section: Lead January 31, 2012 Kentucky Healthy Homes and Lead Poisoning Prevention Program (KHHLPPP)
GUIDELINES FOR BLOOD LEAD LEVELS AND FOLLOW-UP
SEE PRENATAL LEAD SCREENING GUIDELINES IN PRENATAL SECTION FOR PRENATAL PATIENTS BLOOD LEAD LEVEL ASSESSMENT INTERVENTIONS FOLLOW-UP
Submit venous confirmation specimen 45–69.9 µg/dL Lead Poisoning BLL> 15 Same as listed above except refer to within 48 hours µg/dL PCP for medical evaluation. Provide During and post chelation therapy, retest A VENOUS specimen is PCP with letter/information on lead monthly until: needed to confirm a specialist consult within 48 hours. Blood lead level is less than 10µg/dL for 6 diagnosis of lead months (capillary specimens are acceptable) poisoning at this level. or as s ordered by the physician Establish a tracking system that assures retesting and case management For medical case closure see case closure section Environmental: Lead hazards have been addressed
Lead Poisoning BLL> 15 Submit venous specimen within 24 hours 70µg/dL and above µg/dL Same as listed above except refer to During and post chelation therapy, retest PCP for medical evaluation. Provide monthly until: MEDICAL EMERGENCY PCP with letter/information with lead Blood lead level is less than 10µg/dL for 6 A VENOUS specimen is specialist consult within 24 hours. months (capillary specimens are acceptable) needed to confirm a or as s ordered by the physician diagnosis of lead Establish a tracking system that assures poisoning at this level. retesting and case management For medical case closure see case closure section Environmental: Lead hazards have been addressed
* Contact KY HHLPPP for Lead Specialist contact information
Page 4 of 18 Kentucky Public Health Practice Reference Section: Lead January 31, 2012 Kentucky Healthy Homes and Lead Poisoning Prevention Program (KHHLPPP) LEAD POISONING PREVENTION AND MANAGEMENT
▪Case Management:
Environmental lead exposure continues to cause harm, particularly to young children and pregnant women. This section of the PHPR offers guidance on the provision of lead screening and follow-up services for children 6 months – 6 years of age. Lead screening and follow-up guidelines for pregnant women are included in the Prenatal Section of the PHPR.
According to the Centers for Disease Control and Prevention (CDC), case management of children and pregnant women with elevated blood lead levels involves the coordination, provision and oversight of services required to reduce lead levels to below a level of concern. A hallmark of effective case management is ongoing communication with the caregivers and other service providers, and a cooperative approach to solving any problems that may arise during efforts to decrease a patient’s elevated blood lead level, and eliminate lead hazards in the patient’s environment.
Case management is much more than a simple referral to other service providers. There are 8 components, which should be under the purview of a registered nurse:
Client identification and outreach Individual assessment and diagnosis Service planning and resource identification The linking of clients to needed services Service implementation and coordination The monitoring of service delivery Advocacy Evaluation*
Case management should occur for every child with a 2nd blood lead level of 10ug/dL or greater and for every pregnant woman with a venous level of 5ug/dL or greater. Children and pregnant women with elevated blood lead levels become “health department patients” when their cases are brought to the attention of staff, even if they are or have been receiving direct clinical services elsewhere. They will remain a health department patient until patient case closure.
The report forms are used to coordinate communication between the LHD lead case managers and the state HHLPPP NCI in an effort to assure that all children with an EBLL receive appropriate and timely care. The KHHLPPP NCI monitors incoming lab data and compares this with identified EBLL children reports sent from the LHD. A HHLPPP Initial Report Form includes demographics including *zip code, contact information, social security and a Medicaid number if relevant, actions/interventions marked for appropriate BLL’s, dated, and initialed where appropriate, as soon as the health department case manager becomes aware of a child with a BLL of 10µg/dL or greater. *A zip code must be included to enter the data into the system.
The KHHLPPP initial report form must be filled out for all children with a 2nd blood lead level of 10 -14µg/dL or confirmed BLL of 15 µg/dL or greater and for every pregnant woman with a venous BLL of 5µg/dL or greater. The original report is to be placed in the patient’s chart and a copy of this form may be faxed or mailed to the KHHLPPP NCI.
After the completed Initial Report Form has been sent to KHHLPPP, updates can be entered on the HHLPPP Monthly Report Form. This form should be kept in in patient’s chart and updated as appropriate with follow-up
Page 5 of 18 Kentucky Public Health Practice Reference Section: Lead January 31, 2012 Kentucky Healthy Homes and Lead Poisoning Prevention Program (KHHLPPP)
BLL’s and necessary interventions noted. Copies of the monthly report form will need to be faxed to the KHHLPPP NCI when new entries are made.
If the patient’s BLL increases, thus changing needed interventions please send updated information with appropriate interventions noted to the KHHLPPP NCI.
▪VERBAL RISK ASSESSMENT FOR LEAD POISONING
Review each of these questions at every preventive service for all children ages 6 months–6 years. American Academy of Pediatric (AAP) recommends verbal lead risk assessment to be performed at ages 6, 9, 12, 18, and 24 months, and ages 3, 4, 5, and at 6 years with appropriate action to follow if blood lead level is positive. AAP recommends and Medicaid requires blood lead testing at ages 12 and 24 months. These questions are also included on the Health Risk Assessments (ACH 25, 90 and ACH 91).
Pregnant Women Review each of these questions at the positive pregnancy test visit or initial prenatal visit to determine if patient is at-risk.
A copy of the Verbal Lead Risk Assessment Questionnaire can be found in the Forms and Teaching Sheets/Teaching Sheets Section under Lead/ACH 25 section of the PHPR. The questionnaire reviews potential patient risks such as:
1. Does the patient live in or visit a building built before 1978 with peeling/chipping paint or undergone recent or ongoing remodeling (dust)? 2. Does the patient or any other members of the household (child’s playmate/ brother/sister/ patient’s spouse) have a history of elevated blood lead levels or who has had lead poisoning? 3. Does the patient or someone who visits or in the household work in an occupation known or suspected to involve lead? Common industries using lead include but are not limited to: Auto mechanics/bodywork Plumbing Farm/Migrant Farm Work Blowing Glass Jewelry Making/Repair Furniture Refinishing Gardening Metal Sculpting Renovation Work Painting Stained Glass Painting Roads Printing Car/Boat repair Metal Work/Welding Casting Aluminum Firing Ranges Plastics manufacturing Ceramic Making Firearms/Firing Range Radiator Repair Battery Recycling/Smelting/Recycling Making Bullets/Sinkers/lead toys High Construction Area Electronic soldering Home Repairs/Remodeling Bridge Repair/Painting Smelting Metals/ Scrap yards
4. Does the patient use any folk remedies that may contain lead or use pottery or ceramic ware for cooking, eating, or drinking or participate in hobbies that may involve lead such as ceramic pottery, jewelry making, gardening or stained glass? IMPORTED COSMETICS: ▪ Middle East, India, Pakistan, Africa ▪ Kohl, Surma, Al Koh: a powder used both as a cosmetic eye make-up and applied to skin infections and the navel of a newborn child. And can be ingested when on hands ▪ Kajal: eye cosmetic when used can be ingested if on hands. ▪ Sindoor: a powder applied to face or scalp during ceremonies, mistakenly used as food FOODS: ▪ Middle East: ▪ Lozeena: a bright orange powder used by Iraqis to color rice and meat▪ Mexico ▪ ▪ Chapulines (dried grasshoppers): can be chocolate coated; grasshoppers eat chilies that are contaminated with lead from soil and area silver mine fallout
Page 6 of 18 Kentucky Public Health Practice Reference Section: Lead January 31, 2012 Kentucky Healthy Homes and Lead Poisoning Prevention Program (KHHLPPP) FOLK REMEDIES: ▪ Hispanic ▪Azarcon aka: Ruedo, Corol, Maria Luiso, Alarcon, Ligo: used for intestinal illness. ▪ Mexico ▪ Greta: a yellow powder used for intestinal illness. ▪ Dominican Republic ▪▪ Litargirio: yellow peach powder used as a deodorant, foot fungicide, treatment for burns and wound healing. ▪ Vietnam/ Hmong Community ▪ Pay-loo-ah- a red powder given for rash or fever. ▪ Asian/ Tibet/ India/Thailand ▪ Ayurvedic
medicine, ▪ Tibetan Herbal Vitamin ▪ China▪ Jin Bu Huan: used to relieve pain, ▪Po Ying Tan: used to treat minor ailments in children, Ba-Baw-San. ▪ India ▪ Ghasard: a brown powder given as an aid to digestion. ▪Thailand▪ Daw Tway is a digestive aid used in Thailand and Myanmar (Burma). ▪ Iran ▪Bint Al Zahab: Rock ground into a powder and mixed with honey and butter given to newborn babies for colic and early passage of meconium after birth. ▪ Saudi Arabia ▪ Traditional Saudi Medicine: Orange powder prescribed by a traditional medicine practitioner for teething; also has an antidiarrheal effect, ▪Santrinj: An amorphous red powder containing 98% lead oxide used principally as a primer for paint for metallic surfaces, but also as a home remedy for "gum boils" and "teething."▪ Bint Dahab: A yellow lead oxide used by local jewelers and as a home remedy, ▪ Kuwait ▪ Bokhoor: A traditional practice of burning wood and lead sulphide to produce pleasant fumes to calm infants. Other: ▪Bala Goli: a round, flat, black bean dissolved in ‘gripe water’ and used for stomach ache. ▪Kandu: a red powder used to treat stomach ache.
5. Does the patient live near a busy road/ highway? Soil around the home could be contaminated by the leaded gasoline fallout, on the soil or in water (cisterns/wells) for many years following contamination and can get on a child’s hands. Lead can also be absorbed from the soil in fast growing plants such as Kale, spinach, and other garden vegetables from the soil and then consumed by animals and humans and can lead to increase in blood lead levels.
Document in the medical record when assessment was completed, any positive response(s) and action(s) taken:
If the verbal risk assessment is negative at each visit, a blood lead level test should be routinely done for all Medicaid children and children who reside in a **targeted zip code area at 12 and 24 months of age. A “Yes” or “don’t know” answer to any question on the risk assessment will warrant a blood test for lead poisoning at that time, regardless of the child’s payer source or zip code area. Any child with a positive risk factor should be tested at least annually, until 6 years of age, as long as any risk factor exists.
A “Yes” or “don’t know” answer to any question on the risk assessment questionnaire will warrant a blood test for lead poisoning or a referral to the PCP.
See also the Prenatal section of the PHPR for Lead Screening Guidelines and Follow Up. Document in the medical record at the initial prenatal visit and anytime that the assessment was done, any positive response(s), and action taken according to the class chart guidelines located in the Prenatal section of the PHPR.
▪ BLOOD LEAD TESTING
Children and pregnant women regardless of payer source must have a blood test if they have a “Yes” or “don’t know” answer to any question on the risk assessment. For Medicaid enrolled pregnant women, Medicaid will pay for a blood lead screening, all others will need to pay per sliding fee scale or private insurance.
Children who receive Medicaid benefits or reside in a **targeted zip code area must have a blood lead test at 12 and 24 months of age.
All children between 2 and 6 years of age who receive Medicaid benefits or reside in a targeted zip code area must be provided a blood lead test when they present to the health department if they have not previously received a documented blood lead test. Page 7 of 18 Kentucky Public Health Practice Reference Section: Lead January 31, 2012 Kentucky Healthy Homes and Lead Poisoning Prevention Program (KHHLPPP)
*See Blood Specimen Collection Guidelines in the Lead Section and also the Lab Section
COMPLETION OF LABORATORY SUBMISSION FORMS Please fill out lab requisition forms accurately and completely, including your agency as the provider.
A. SCREENING This should be checked for the: initial capillary sample; first venous sample venous samples should always be taken on pregnant women re-screenings of children with levels equal to or greater than 10ug/dL and any screening test being repeated due to clot, insufficient quantity, or any other reason the sample could not be analyzed. B. CONFIRMATORY This should be checked for: the second capillary sample when the first capillary sample was equal to or greater than 15 micrograms per deciliter (lead poisoning). venous samples submitted as confirmatory samples after a first capillary sample was equal to or greater than 15 micrograms per deciliter and confirmatory tests being repeated due to clot, insufficient quantity, or any other reason the sample could not be analyzed. C. MEDICAL FOLLOW-UP This should be checked for: follow-up tests of ALL children who have been previously confirmed to be lead poisoned and medical follow-up tests being repeated due to clot, insufficient quantity, or any other reason the sample could not be analyzed.
NOTE: Venipunctures are confirmed specimens and if the results are greater than or equal to 15 micrograms per deciliter (µg/dL), this is to be considered a confirmed case of lead poisoning. Follow the recommended actions for levels greater than or equal to 15ug/dL as indicated in the “Guidelines for Blood Lead Levels and Follow-Up.”
NOTE: See Administrative Reference for payment procedures.
▪ HOME VISITS AND ENVIRONMENTAL MANAGEMENT FOR PATIENTS WITH ELEVATED BLOOD LEAD LEVELS (EBLL)
According to KRS 211.905, an inspection of the property where an EBLL child routinely spends more than six (6) hours per week should be completed to determine the existence of lead-based hazards.
Priority should be given to the child’s primary place of residence. The environmental investigations may include the visual as well as the comprehensive lead risk assessment to determine the existence of lead based hazards.
Environmental Management through home visits is one component of an on-going process related to the elimination of lead poisoning as a public health problem. Home visits and visual investigations help to: Identify areas in the home that could potentially be a source for lead exposure;
Provide suggestions and educational materials to the family in an effort to make the home lead-safe;
Page 8 of 18 Kentucky Public Health Practice Reference Section: Lead January 31, 2012 Kentucky Healthy Homes and Lead Poisoning Prevention Program (KHHLPPP) Reduce the patient’s current BLL to less than 10µg/dL by reducing or eliminating the amount of lead exposure;
Assure that patient’s with an EBLL receive timely and appropriate care.
Collaboration of the environmentalist and the lead case manager assures appropriate and timely environmental home visits and investigations for patients who are identified with EBLL’s. Interventions during investigations include: Informing the patient/parent/guardian/care giver of child’s blood lead level; review level of understanding; monitoring of blood lead levels, Reviewing what lead poisoning is and common sources of lead, provide educational materials; Reviewing health education and preventive lead poisoning strategies, provide suggestions in an effort to make home lead safe and to reduce the amount of lead exposure; Reviewing lead poisoning prevention diet, Reviewing patient’s physical status, including behavior problems/changes, nutritional status and specific habits such as placing fingers in mouth or eating dirt or paint chips; Establishing who is providing patients primary and acute health care; Visualize the patient’s home environment and child play areas to identify potential sources of lead; is the home pre-1978 and have chipping, peeling paint or dust throughout home and discuss emergency measures to reduce the patient’s lead hazard exposure; Assure the well-being of the child by referring to appropriate agencies; services may include social services for emergency or temporary housing agencies.
Home visits by a nurse or allied health professional as defined in the Home Visiting Section of the PHPR, are to be conducted for all children referred into or already receiving services in a health department clinic with a second blood lead level remaining at 10–14µg/dL or a confirmed blood lead level of 15µg/dL micrograms per deciliter or above and for pregnant women with a BLL of 10ug/dL or greater.
Upon receipt of EBLL results, the lead case manager is responsible for collaboration and referrals to the environmentalist or risk assessor for appropriate environmental investigations. For children identified as having BLL’s of:
2nd BLL of 10µg/dL or greater, a home visit and visual investigation are to be completed at the children and pregnant women’s primary residence to identify potential sources of lead. Confirmed BLL of 15µg/dL or greater (lead poisoning), in addition to the home visit/visual investigation, a referral for a lead risk assessment must be completed to a a certified risk assessor.
If your health department or district does not employ a certified risk assessor, please contact the KHHLPPP• 502-564-2154•275 East Main Street •Frankfort • KY •40621 If a lead poisoned child is referred to the health department and no environmental risk assessment has been completed on their current home, referrals for a lead risk assessment may need to be completed for those patients living in at-risk conditions.
Investigation of the Primary Address: The initial home visit should be initiated by the LHD lead case manager or home visiting nurse following time frames listed below (See Table 1). The visual investigation is generally completed by the environmentalist however can also be completed at the time of a home visit by a trained home visiting RN. Investigations should be conducted within the appropriate timeframes according to CDC’s recommendations. (See Table 1) However, KHHLPPP recommends timeframe of two (2) weeks for BLL’s 10-14ug/dL to visualize potential sources of lead and to review preventive education with the parent/guardian/.care giver and to prevent further elevation of the BLL.
Page 9 of 18 Kentucky Public Health Practice Reference Section: Lead January 31, 2012 Kentucky Healthy Homes and Lead Poisoning Prevention Program (KHHLPPP)
Table 1: Home Visit and Visual Investigation Blood Lead Level Time Frame for Assessment 2nd BLL 10-14ug/dL 4 weeks of 2nd BLL in this range 15-19.9 µg/dL 2 weeks; refer for comprehensive lead risk assessment 20-44.9 µg/dL 1 weeks; refer for comprehensive lead risk assessment 45-69.9 µg/dL 48 hours; refer for comprehensive lead risk assessment >70 µg/dL 24 hours; refer for comprehensive lead risk assessment
At the time of the assessment, preventive education should be reviewed with the parents/guardians/care giver. Preventive education includes discussing the child’s potential source of lead-based hazards and how to prevent further exposure to those sources, increase child’s hand washing with soap and water, house cleaning techniques such as damp dusting, wet mopping, and daily vacuuming of the home. Temporary measures to reduce further exposure are not required within a specific timeframe, however it is recommended to keep the child away from the potential sources. If the child’s BLL should increase to lead poisoning (BLL >15ug/dL), it is required per KRS 211.905 to correct any identified lead hazards within sixty (60) days. Temporary measures may include but are not limited to:
Blocking child from potential hazardous area with a barrier, (i.e. door, child gate); Using furniture to block child’s access to the hazard (i.e. furniture in front of a chipping window sill); Use of duct or masking tape and plastic or cardboard to cover an area of chipping/peeling surface until permanent work can be conducted; Daily damp dust, wet mop and vacuum with a hepa vac especially in the child’s play area; Wipe child’s toys clean, keep toys in clean dry tote, and placing tote in clean play area and limiting the child’s play to this area; (especially if child is crawling and/or in hand-to-mouth exploration stage); Keep child’s hands washed with soap and water, (germ gel does not remove lead), wash hands before snacks and meals and before any nap or bedtime (especially if child is crawling and/or in hand-to-mouth exploration stage); Exploring the possibility to relocate child(ren) and pregnant women from the home while renovation/remediation work is in progress.
A thorough visual investigation of the child’s home identifies possible sources of lead. The investigation should visualize both the interior and exterior environment of the child with attention given to child accessible painted surfaces, dust and soil. Other potential sources of lead should be considered during the assessment i.e., water, family occupation, hobbies, etc.
If the BLL remains elevated or at a level of lead poisoning and is not decreasing in 8-12 weeks, an environmental investigation may need to be conducted at another property where the child routinely spends more than six (6) hours a week.
The home visit/visual investigation form should include any pertinent information from the child's parent/guardian/care giver that is not already supplied on the referral form. This should include the following: How long the child has lived at this address Supplemental address information Number and names of children that live or visit here Owners name, address and phone number Child’s play areas, sleep areas, habits Parents occupations, hobbies, other possible sources.
Page 10 of 18 Kentucky Public Health Practice Reference Section: Lead January 31, 2012 Kentucky Healthy Homes and Lead Poisoning Prevention Program (KHHLPPP)
Lead Risk Assessments For children identified with confirmed lead poisoning, a BLL >15µg/dL, a lead risk assessment is required according to KRS 211.905 (1). Comprehensive Lead Risk Assessments referrals are made by the LHD case manager and should be conducted by a certified risk assessor within the appropriate time frames per CDC’s recommendations. (See Table 2)
Table 2: Comprehensive Lead Risk Assessment Blood Lead Level Time Frame for Type of Assessment Assessment >70 µg/dL Within 24 hours Comprehensive Lead Risk Assessment 45-69.9µg/dL Within 48 hours Comprehensive Lead Risk Assessment 20-44.9 µg/dL Within 1 weeks Comprehensive Lead Risk Assessment 15-19.9 µg/dL Within 2 weeks Comprehensive Lead Risk Assessment Persistent BLL at10-14ug/dL Within 4 weeks Comprehensive Lead Risk Assessment
The lead risk assessment report can take up to 30-90 days to process and receive.
The case manager must collaborate with the environmentalist to assure timely and appropriate environmental follow up. When the LHD receives its copy of the lead risk assessment report, both the case manager and the environmentalist should review the report to coordinate appropriate preventive strategies and interventions.
Follow-Up Home Visits Follow-up home visits also assure measures for lead poisoning prevention are continuing. Follow-up home visits are also indicated when:
a. Child fails to return for blood lead monitoring b. blood lead levels remain elevated c. blood lead levels are increasing d. at any other time the case manager feels a home visit would be beneficial
Assessment Interventions Family’s verbal understanding of lead Reinforce previous health education poisoning. and prevention Assess barriers to patients ability to Stress importance of monitoring blood lead levels every 1–2 months or as ordered by keeping appointments, refer as the physician for confirmed lead poisoning cases and every 3 months for 10–14 appropriate micrograms per deciliter. Patient’s physical status. Provide health education and referral, if indicated. Patients blood lead level status. Collect blood and/or schedule a clinic appointment, if indicated. (Coded “Screening” or “Confirmatory” sample. “Medical Follow-up” if child has been confirmed.) Home environment: determine Reinforce previous recommendations. whether temporary measures are Provide education, as indicated. continuing. Determine whether permanent Stress importance of workers using safety precautions and appropriate clean-up measures have occurred/are procedures during abatement. Encourage pregnant women and children to be kept planned. away from work areas. While extensive work is being done, it is preferable to move the family out of the home.
Page 11 of 18 Kentucky Public Health Practice Reference Section: Lead January 31, 2012 Kentucky Healthy Homes and Lead Poisoning Prevention Program (KHHLPPP)
▪Case closure Case closure is determined according to the initial blood lead level and can be closed as follows: •B LL 10-14.9 µg/dL – Case closure is when BLL is less than 10µg/dL, repeat BLL as indicated.
• BLL 15 µg/dL and greater– Case closure is when BLL is less than 10µg/dL for at least 6 months; environmental hazards have been addressed; and there are no new environmental hazards.
When a child is closed to follow-up, according to PHPR guidelines, the date and reason for case closure, and any actions/interventions or comments should be recorded on the case management report in area provided.
For prenatal lead exposure, case closure ends for the pregnant woman at delivery of the infant. If the BLL is >25µg/dL, follow-up will be with the patients PCP. The newborn will need to be tested at delivery. A cord blood sample is to be used for testing at the time of delivery. Protocols for case management will be initiated for newborns with BLL’s >10µg/dL.
A case may also be designated as administrative closure if all directives, as enumerated in the “Follow- up/Internal Tracking/Referral” section of the PHPR, have been completed. The case manager must follow all procedures for closure in a ‘lost to follow up’ case closure.nal (If a case has been closed and at a later date is reopened, send a new Initial Report Form with initial BLL and updated information. Please do not continue on old file and write reopened.)
Forms available @ http://chfs.ky.gov/dph/info/dpqi/PHPR.htm. and then go to Forms and Teaching Sheets and in this section go to Lead/ Report and Home Visit Forms/Onsite Visual Investigation Form.
The home visit, follow-up home visit and visual evaluation forms, when completed, should be filed at the county local health department in the patient’s chart and a copy will be mailed or faxed to the state HHLPPP NCI
Mail to: Healthy Homes and Lead Poisoning Prevention Program Division for Maternal and Child Health 275 East Main Street, HS2GWA Frankfort, Kentucky 40621 Or Fax to: (502) 564- 5766
Resources: “Lead Poisoning: Are Your Children at Risk?” “Preventing Lead Exposure in Young Children” “Lead Poisoning and Your Children” www.epa.gov/lead “Protect Your Children from Lead in Your Home” www.cdc.gov/niosh “Fight Lead Poisoning with a Healthy Diet” www.putthelidonlead.org “Lead Paint Safety” “Prevent Lead Poisoning, Eat Healthy” Manuals: 1. Screening Young Children for Lead Poisoning: Guidance for State and Local Public Health Officials. (CDC, 1997) 2. Managing Elevated Blood Lead Levels Among Young Children: Recommendations from the Advisory Committee on Childhood Lead Poisoning Prevention. (CDC, 2002)
Page 12 of 18 Kentucky Public Health Practice Reference Section: Lead January 31, 2012 Kentucky Healthy Homes and Lead Poisoning Prevention Program (KHHLPPP)
BLOOD LEAD SPECIMEN COLLECTION GUIDELINES
When collecting blood lead specimens, please refer to the laboratory used by your local health department and follow their correct collection guidelines. CDC Guidelines for collecting and handling blood lead samples: http://www.cdc.gov/nceh/lead/training/blood_lead_samples.htm.
Medtox website for Guideline for collecting and handling blood lead samples video: www.Medtox.com, go to Medical testing, go to Filter paper testing, go to view collection video.
Attention: Steps performed before, during, and after collection are of paramount importance.
Lead is everywhere in the environment. Therefore, great care must be taken to remove lead from the hands of the patient and collector prior to collection. It will also prevent contamination of your collection site and work environment. Prepare your worksite in a sterile fashion prior to washing patients and your own hands for the specimen blood draw.
It is recommended for screening children who are younger than one (1) year of age to use the heel of the infant as a puncture site. Guidelines for this procedure can be found at the National Committee on Clinical Laboratory Standards. NOTE: The finger stick collection technique is more prone to environmental contamination than the venous and will affect specimen results. Special precautions are needed to prevent contamination.
CDC recommends confirmation on all lead poisoned results with a venous specimen.
Contamination errors are common in trace metal analysis, so precautions must be taken to eliminate or reduce them. Lead can be picked up by accident from work surfaces, from printed materials or from the hands of the collector. It can also come from the hands and the clothes of the child you are screening. The key to effective lead screening is to collect specimens that have not been contaminated.
To reduce the odds of contaminating your sample: Take special care when preparing your test area and supplies, use sterile fashion.
As much as possible, use only supplies that have been certified as lead free.
Label the liquid soap bottle that will be used for lead testing, “Use for Lead Testing Only”.
Handle all equipment with powder-free gloves. Powdered gloves may contaminate your sample.
Keep all screening supplies—which include your lancet, gauze pads, band aids, tissues, alcohol pads, and micro- collection vials—in a clean plastic box with a snap lid for storage.
When using bulk-packaged micro-collection vials, carefully pour the vials into a re-sealable plastic bag and close to store. Individually packaged kits or a full box of micro-collection vials can be stored as they are. All micro-collection containers from open packages should be stored in a covered plastic container.
There are many types of micro-collection vials you can use to collect samples, but all must be prescreened or certified as lead-free.
Page 13 of 18 Kentucky Public Health Practice Reference Section: Lead January 31, 2012 Kentucky Healthy Homes and Lead Poisoning Prevention Program (KHHLPPP) For Capillary tubes, most vials contain 200 to 300 micrograms per deciliter of blood, EDTA or Heparin tubes are required.
For Capillary Scoop micro-collection vials, these should be used with extreme caution because they have a high potential for contributing to lead and tissue contamination.
Choose a lancet with the appropriate depth to collect the proper amount of blood for the micro-collection vial you are using. Also, use retractable lancets that cannot be used more than once to avoid sticking a child unnecessarily Practice universal precautions and wear protective equipment.
Specimen Collection Technique Preparing the Collection Area: Before you begin, fill out your laboratory request form completely and write the child's name on the vial label or front of filter paper collection Card by applying bar-coded sticker from requisition into box on card, or writing name and patient ID number on card. NOTE: Information must match the requisition and cards without label or identifying information will NOT be tested. Information required for lab reporting and should be placed on lab requisitions include: First Name, Last Name, Middle Initial, Date of Birth, Patient address, City, State, Zip code, Social Security #/ Medicaid/Passport #, Child/Prenatal/Adult, and collection date. Prepare your collection area with a clean, disposable pad in a sterile fashion as to keep area contamination free and always have the following on hand: o Two gauze pads o Liquid soap o Two alcohol pads o Bandages o A self sheathing lancet o Biohazard bag o A micro collection vial or filter paper o Accessible sharps container o Specimen identification label
It's important that the technician/ nurse responsible for obtaining the blood sample is familiar with the techniques for obtaining a high quality blood lead sample, see CDC video at http://www.cdc.gov/nceh/lead/training/blood_lead_samples.htm Capillary/Finger Stick Technique 1. The nurse should help the child thoroughly wash their hands (or foot) with soap and water, as the collector is also washing their hands, paying special attention to the fingertips and under the finger nails and on nail beds, (absolutely do not use gel type sanitizers). If the child will not let the nurse wash their hands, the parents should thoroughly wash their own hands and then the child’s hands, again paying attention to area of the nails.
2. Rinse hands thoroughly.
3. Since recycled and colored towels may have traces of lead, it's best to let hands air dry or use white, lead free towels.
4. To avoid contamination do not let the child's fingers touch any surface, you may need to hold the child’s hand in a gauze or paper towel until you get to your work area.
Page 14 of 18 Kentucky Public Health Practice Reference Section: Lead January 31, 2012 Kentucky Healthy Homes and Lead Poisoning Prevention Program (KHHLPPP) 5. Although you can draw a sample from any finger, we suggest working with the ring finger. The ring finger is less calloused and somewhat less sensitive. Plus, it’s easy to palpitate above the puncture to produce and increase blood flow.
6. Massaging the child’s hand and the lower part of the finger before you make your puncture will calm the child and stimulate blood flow.
7. Clean the finger that you will puncture with an alcohol pad. If you see dirt on the pad, use a new alcohol pad until clean.
8. Allow finger to air dry or wipe dry with sterile gauze. NOTE: If alcohol remains on the finger, it will prevent the blood from forming a well-rounded drop and will contaminate the sample. Wiping will also prevent alcohol from getting into the cut and stinging. Remember to keep the finger isolated from the rest of the hand.
9. When you are ready for blood collection, hold the child's finger in a downward position.
10. Use the appropriate blade and lance the palm side of the finger. Do not lance the side or the tip.
a. Correct finger stick Puncture across grooves of fingerprint; a round drop of blood will form b. Incorrect finger stick: Puncture parallel to grooves of fingerprint; blood runs down finger; will not form into a drop. This enables the blood to form as a drop on the fingertip. If the puncture is parallel to the lines of the fingerprint, the blood will not form as a drop but will run down the finger making correct collection impossible.
11. Promptly blot the first drop of blood on a gauze pad and discard in the appropriate container. The first drop of blood is likely to contain excessive tissue fluid that can alter test results.
12. To collect a droplet of blood, keep the child's finger in a downward position and gently massage it to maintain blood flow. If blood flow is inadequate, gently massage the child's finger to stimulate more flow, but don't squeeze the finger because tissue fluid may dilute the sample. Avoid strong, repetitive pressure and do not scrape the finger during collection.
Capillary Tubes/Vial Collection
Hold the micro-collection tube at a 10 degree angle below the collection line. Touch the tapered end of the tube into the droplet of blood and not directly on the skin. Capillary action will cause the blood to fill the tube. As the blood starts entering the capillary tube, be careful not to allow air bubbles to enter. You will need to collect your sample within two minutes to avoid clotting.
Also avoid collecting smeared blood or blood that has run into the cuticle or nail area.
Depending on the micro-collection vial you use, the amount of blood you collect will vary. Fill tube to the appropriate line in order to have both the correct anticoagulant-to-blood ratio and to supply a sufficient amount of blood to the lab for testing.
Seal the micro-collection vial and gently invert the container 7 to 10 times to prevent clot formation. Clots can render the specimen unsuitable for testing. Page 15 of 18 Kentucky Public Health Practice Reference Section: Lead January 31, 2012 Kentucky Healthy Homes and Lead Poisoning Prevention Program (KHHLPPP) Carefully place the child’s identification label on the micro-collection vial vertically. If the label is not fixed vertically, the laboratory will not be able to read it. Filter Paper Collection Lead testing requires that a SINGLE large drop of blood FREELY falls and is absorbed uniformly by the filter paper. Do not scrape, smear, smudge, wipe or touch finger or blood to the filter paper, these specimens will be rejected.
Collect at least two large, separate blood drops that:
Evenly saturate the filter paper, i.e., the spot will appear the same on front and back of the paper (see examples, p. 2 on Medtox Guideline examples). Evaluate the sample collection. Examine the back side of the filter paper to ensure that the blood has soaked evenly through to the paper. If NOT acceptable, repeat finger stick and recollect sample on a new sample card. Are about the size of the black circles (½ inch diameter). NOTE: Blood spots do NOT have to be within the black circles but must be large enough for testing (2 spots with minimum 3/8 inch diameter). If drops are free falling, the drop will be large enough to read, do not touch blood or finger to paper. NEVER put a 2nd drop of blood on top of a spot of blood already on the paper (i.e., multiple drops), which makes the collection unacceptable for testing and will be cancelled as a smear, non-homogeneous, or unsuitable (see examples, p. 2 on Medtox examples). If a hemoglobin test is also requested, a 3rd acceptable free falling blood spot is required. A “HGB” circle is provided as a guide on the white Pediatric Lead/Hemoglobin blood sample card, however can be anywhere in the collection area as long as it does not overlap another blood drop. Dry collection Card: Allow the opened collection Card to air dry for at least 2 – 5 minutes. Place the dry card into a plastic bag and seal. NOTE: Samples received wet CANNOT be tested—occurs when cards are immediately placed into plastic bag or when filter paper is saturated with too much blood. Please let these cards dry. 13. Ship specimen promptly per protocol of the laboratory.
When the child's blood level results are received from the laboratory, consult PHPR Lead section for intervention guidelines according to blood lead results.
Page 16 of 18 Kentucky Public Health Practice Reference Section: Lead January 31, 2012 Kentucky Healthy Homes and Lead Poisoning Prevention Program (KHHLPPP)
Targeted Zip Codes
Adair Breckinridge Edmonson Graves Henry 42715 40170 42275 42040 40007 42742 42285 42061 40058 42761 Calloway 42076 Elliott Grayson Hopkins Allen 41171 42762 42408 42153 Campbell 42410 41071 Estill Green Ballard 41073 40336 42743 Jackson 42060 41074 40472 40447 41085 Greenup 40486 Barren Fayette 41174 42160 Carlisle 40508 Jefferson 42021 Hardin 40202 Bath 42023 Fleming 40155 40203 40374 41049 40177 40204 Carter 40205 Bell 41146 Floyd Harlan 40206 40845 41605 40801 40208 40902 Casey 41606 40807 40209 40958 42528 41607 40810 40210 40977 42539 41612 40815 40211 40988 41615 40819 40212 Christian 41619 40820 40213 Bourbon 42266 41630 40823 40215 40348 42254 41635 40828 40217 40361 41636 40830 Clay 41640 40831 Johnson Boyd 40914 41649 40843 41216 41101 40941 41650 40854 41219 40972 41651 40855 41222 Bracken 40983 41653 40863 41228 41002 41660 40870 41238 41004 Clinton 41666 40873 41240 42602 41669 41254 Breathitt Hart 41255 41317 Crittenden Fulton 42722 41257 41339 42064 42041 42729 41260 41385 42050 42749 41263 Cumberland 41265 42759 Garrard Hickman 41268 Kenton 40461 42031 41274 41011 Lee Magoffin Muhlenberg Pike 41014 41311 41426 42374 41514 Page 17 of 18 Kentucky Public Health Practice Reference Section: Lead January 31, 2012 Kentucky Healthy Homes and Lead Poisoning Prevention Program (KHHLPPP)
41015 41397 41464 42321 41524 41016 41465 42332 41543 Letcher 41632 42339 41546 Knott 40826 41549 41740 40862 Martin Ohio 41553 41822 41537 41203 42333 41555 41843 41819 41224 42338 41563 41844 41825 41250 42343 41564 41759 41826 41262 42369 41567 41772 41833 41267 41569 41817 41835 Owen 41834 41855 Mason 40355 Todd 41839 41810 41055 42204 41859 41840 41056 Owsley 41845 41314 Warren Knox 41849 Meade 41364 42170 40734 40104 41386 40771 Lewis 40176 Wayne 40903 41135 Pulaski 42633 40906 41170 Menifee 42501 42632 40935 41179 40322 42544 40953 40346 42553 Webster 40982 Lincoln 40387 42450 40995 40448 Wayne 42463 40997 Mercer 42633 42403 Livingston 40310 42632 Lawrence 42047 Whitley 41124 Metcalf Perry 40759 41159 Logan 42129 41367 40763 41230 42265 42154 41701 40769 41712 Leslie McCreary Monroe 41723 Wolfe 40827 42647 42167 41778 41301 40858 42653 42157 41735 41332 40874 42638 42140 41751 41365 41714 Morgan 41773 41730 McLean 41408 41762 42371 41421 Robertson 41775 41425 41064 41776 Marion 40009 Nelson Rowan 40328 40008 40313
Page 18 of 18 Kentucky Public Health Practice Reference Section: Lead January 31, 2012