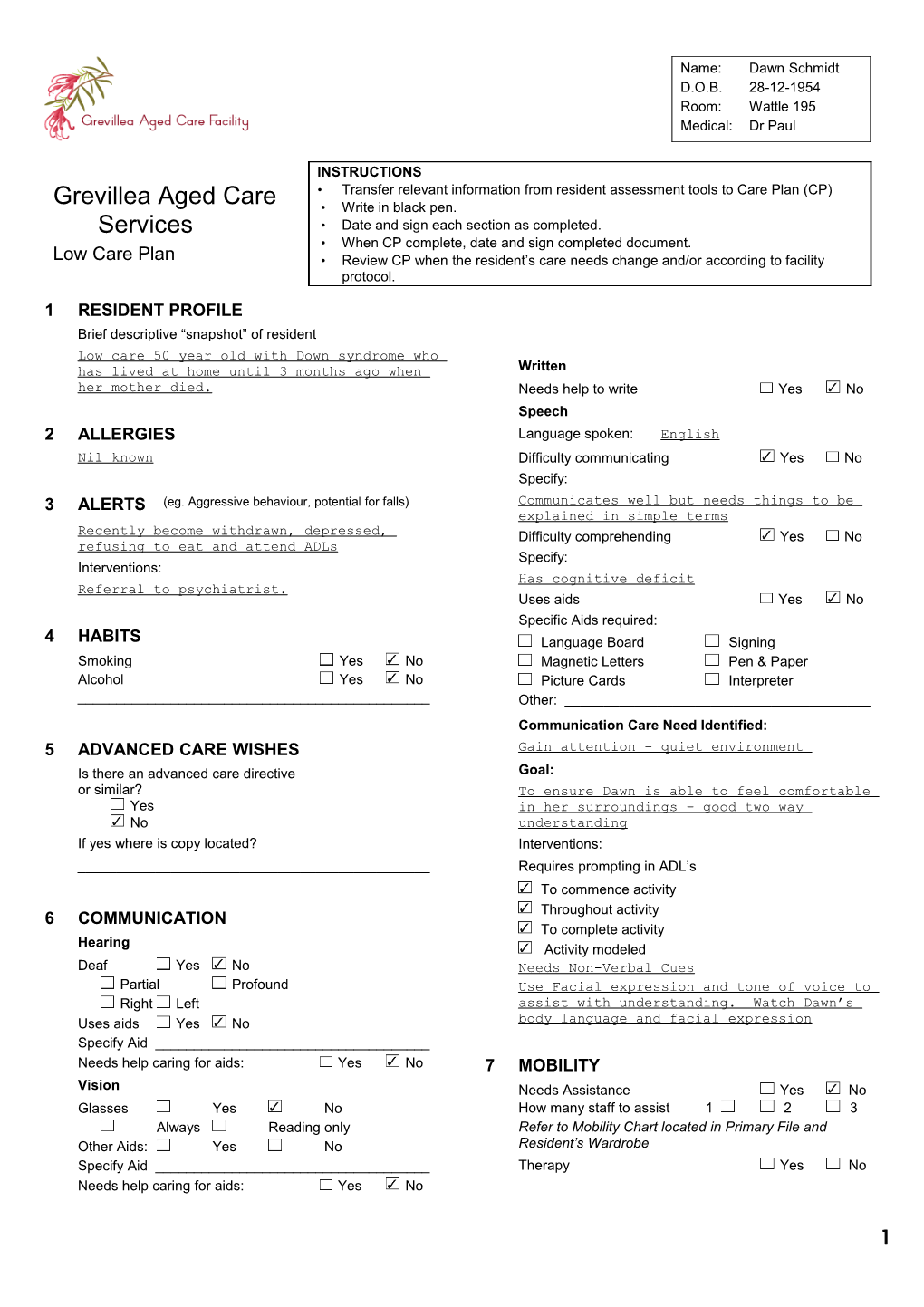
Name: Dawn Schmidt D.O.B. 28-12-1954 Room: Wattle 195 Medical: Dr Paul
INSTRUCTIONS • Transfer relevant information from resident assessment tools to Care Plan (CP) Grevillea Aged Care • Write in black pen. Services • Date and sign each section as completed. • When CP complete, date and sign completed document. Low Care Plan • Review CP when the resident’s care needs change and/or according to facility protocol.
1 RESIDENT PROFILE Brief descriptive “snapshot” of resident Low care 50 year old with Down syndrome who has lived at home until 3 months ago when Written her mother died. Needs help to write Yes No Speech 2 ALLERGIES Language spoken: English Nil known Difficulty communicating Yes No Specify: 3 ALERTS (eg. Aggressive behaviour, potential for falls) Communicates well but needs things to be explained in simple terms Recently become withdrawn, depressed, Difficulty comprehending Yes No refusing to eat and attend ADLs Specify: Interventions: Has cognitive deficit Referral to psychiatrist. Uses aids Yes No Specific Aids required: 4 HABITS Language Board Signing Smoking Yes No Magnetic Letters Pen & Paper Alcohol Yes No Picture Cards Interpreter ______Other: ______Communication Care Need Identified: 5 ADVANCED CARE WISHES Gain attention – quiet environment Is there an advanced care directive Goal: or similar? To ensure Dawn is able to feel comfortable Yes in her surroundings – good two way No understanding If yes where is copy located? Interventions: ______Requires prompting in ADL’s To commence activity Throughout activity 6 COMMUNICATION To complete activity Hearing Activity modeled Deaf Yes No Needs Non-Verbal Cues Partial Profound Use Facial expression and tone of voice to Right Left assist with understanding. Watch Dawn’s Uses aids Yes No body language and facial expression Specify Aid ______Needs help caring for aids: Yes No 7 MOBILITY Vision Needs Assistance Yes No Glasses Yes No How many staff to assist 1 2 3 Always Reading only Refer to Mobility Chart located in Primary File and Other Aids: Yes No Resident’s Wardrobe Specify Aid ______Therapy Yes No Needs help caring for aids: Yes No
1 Name: Dawn Schmidt D.O.B. 28-12-1954 Room: Wattle 195 Medical: Dr Paul
R.N./E.N. to attend Yes No Date 3/4/05 Signature: P Rogers Review Date: Signature: Date Signature: Review Date: Signature:
Grevillea Hostel
Goal/s To ensure that Dawn gets some activity each Care need identified: day. Dawn can cut her own nails, care worker to Passive Exercises Yes No check weekly. Active Exercises Yes No Oral/Dental Hygiene Active/Assisted Exercises Yes No Dentist public private Walking Program Yes No Dentist name:______Phone:______Other: NA Refer to Physiotherapy Mobilisation Plan in primary file and Dental Appointments: resident’s wardrobe Own teeth Upper Lower Falls Denture Upper Lower Potential for falls Yes No Denture Labelled Upper Lower Hip protectors to be worn Yes No Assistance needed Yes No Goal: Best time to clean teeth: Refer App: 108a Restrain Order, App: 108b/c Record of Physical Restraint and App: 108d Review of Restraint Prompt Dawn to clean her teeth after meals. Order. Alerts: Interventions: Forgets to do oral hygiene NA Won’t open mouth Does not understand Can’t rinse and spit 8 PERSONAL CARE and ROUTINES Bites toothbrush/staff Resident’s preferred routine and needs in personal hygiene, Aggressive nail and oral care. Constantly grinding and chewing Shower daily 2nd daily weekly Head bent forward/face in downward position Spa daily 2nd daily weekly Personal Care Goals: Trolley daily 2nd daily weekly To ensure mouth is kept clean – promote Sponge daily 2nd daily weekly healthy gums. Interventions in addition to those recorded am pm above. Other: (eg soap moisturiser) Nutrition and Hydration Ensure that Dawn has a shower each day Goal/s nd Hair wash: daily 2 daily weekly + PRN To ensure Dawn is well nourished and How many staff to assist 1 2 3 hydrated – to assist in reducing current excess in weight. Grooming and Dressing Diet Help with dressing/undressing Yes No Supervise Assit Feed Modelling Specify: Modelling Ensure that Dawn changes her clothes on a Type of Assistance Required: regular basis. Ensure that Dawn is eating each meal. Record How many staff to assist 1 2 3 and report the results. Other (eg shaving, makeup hairdressing etc) N.B.M. Pureed Nail Care Soft Cut up Full Podiatrist required Yes No
2 Name: Dawn Schmidt D.O.B. 28-12-1954 Room: Wattle 195 Medical: Dr Paul
Pressure ulcer “at risk” Yes No Rash “at risk” Yes No Excoriation “at risk” Yes No Date 3/4/05 Signature: P Rogers Other: NA Review Date: Signature: Date Signature: Review Date: Signature:
Grevillea Hostel
Meal times, aids and location Ensure Dawn comes to the dining room for each meal. Fluids N.B.M. Nectar/Soup Goal for skin care: NA As desired Yoghurt Gel If yes above, refer to related App: 231 Wound Assessment Supervise Assist Feed and Management Chart for this resident Modelling Specify resident’s skin care routine: NA Aids required: Sleep and Rest 10. MEDICATION ADMINISTRATION Goal/s: Self administration Yes No To ensure adequate rest and relaxation. Goals: Usual retiring time: 2100 hrs To ensure medications are taken, as Initiated by Resident Staff prescribed by GP. Usual time asleep: 2200 hrs Interventions Usual time awakening: 0800 hrs Ensure Dawn takes any medications as Describe any sleep inducing interventions used, eg warm prescribed. milk drink, analgesia, relaxation music, massage, and the effect: 11 HEALTH STATUS MONITORING NA Vital signs to be recorded Yes No Medications related to sleep/rest. Please tick relevant observations and indicate frequency Does the resident currently require sedatives? Yes No Observation Freq. Observation Freq. Assessed rest pattern needs: Pulse Weight 1/12 Morning Nap: Nil am/pm Temperature BMI Usual duration: Respirations Urinalysis 30 min 1 hr 1.5 hrs 2 hrs BP Fluid Chart Risk alerts during rest/sleep periods: BGL Other NA Refer to App.32 Sleep Assessment 12 CONTINENCE AND TOILETING 9 SKIN CARE NEEDS a. Urinary Continence – competent Skin Integrity Assessed Yes No ______App: 174 Skin Integrity Assessment ______Dates attended/reviewed. 1. On Admission App: NA Continence and Monitoring Assessment 2. ______Yes No Assessment Outcomes Date attended: ______Skin tear /dry skin Yes No Review date: ______Wound Yes No Continent of urine Yes No
3 Name: Dawn Schmidt D.O.B. 28-12-1954 Room: Wattle 195 Medical: Dr Paul
Goal: c. Toileting Treatment and Management Plan Summary – Needs assistance with toileting Yes No Increase fluid intake Goal/s Strategies to improve mobility Locating toilet Introduce toileting program Transport to/from toilet Timed/scheduled toileting program Getting on and off toilet Prompted toileting program Managing toilet paper/wiping Bladder retraining program Performing post toilet hygiene Date 3/4/05 Signature: Prompt and instruct step by step P Rogers Model desire action Review Date: Signature: Staff complete entire procedure Date Signature: Returning to activity/room Review Date: Signature:
Grevillea Hostel
Highlight times as per assessed needs (24 hr clock) Toilet Risk Management strategies: 1 2 3 4 5 6 7 8 9 10 11 12 Supervise in bathroom Yes No Shower Chair Yes No 13 14 15 16 17 18 19 20 21 22 23 24 Arm rails Yes No Pelvic floor exercise program Other: NA Use of incontinence product/aids (specify below) Referral medical or nursing specialist NA 13. TECHNICAL AND/OR COMPLEX NEEDS b. Faecal Continence Specify in terms of goals and interventions eg pain App: 4 bowel Management, Assessment and management, palliative care, tracheostomy, oxygen therapy etc. and strategies. Evaluation attended Yes No NA Date attended: 3/5/05 Review Date: ______Continent of faeces Yes No Constipation Yes No 14. COGNITIVE AND MENTAL HEALTH Goal: a. Cognitive – assessment attended To increase fluids, diet and mobility to SMMSE with the Yes No overcome constipation. MMSE assistance Yes No Increase fluid intake Score: 1 Increase exercise/mobility Goal: Increase dietary fibre Introduce toileting program To promote feelings of contentment and security in her environment. Timed/scheduled toileting program Prompted toileting program Interventions: Planned evacuation program Explain all procedures before commencing; Highlight days and times as per assessed needs allow time for her to process information. Promote self-esteem by involving Dawn by allowing her to make choices about her self care. 1 2 3 4 5 6 7 9 10 11 12 b. Depression – assessment attended 13 14 15 16 17 18 19 21 22 23 24 Initial Depression Check Yes No Introduce laxative therapy Non-Verbal Depression Scale Yes No Evacuation products/aids (specify below) Score: ______To have Aperient if bowels not opened after Yesavage Depression Scale Yes No 2 days. To have Microlax enema if BNO after 3 days. Score: 48 Needs case conference Referral medical or nursing specialist Goal: Other: May need regular aperients
4 Name: Dawn Schmidt D.O.B. 28-12-1954 Room: Wattle 195 Medical: Dr Paul
To reduce feelings of depression to give Self Esteem Building e.g. beauty care, art, craft. Dawn a feeling of well-being and Hair care, daily clothing choice, contentment. hairdresser – 2 monthly Interventions: Social Group e.g. sing-a-long, Bingo, movies, cards. Encourage family visits. Encourage Dawn to Special theme days have control over her daily routine. Encourage Dawn to do her own washing and Sing-a-long ironing. Plan a supported holiday Social Individual (one-on-one) e.g. reading, reminiscence, paired board games such as backgammon Date 3/4/05 Signature: P Rogers Going to movies once a fortnight, encourage Review Date: Signature: Dawn to read weekly magazines as she did Date Signature: with her mother. Physical/Tactile e.g. hand massage, balloon game, quoites, Review Date: Signature: carpet bowls. Exercises to music – weekly
Grevillea Hostel 16. CULTURAL c. Behavioural – assessment attended Cultural needs identified Yes No Creighton Yes No Goal: Score: 38 (critical) Interventions eg pets, diet, music, special days, numbers or C.A.S. Behaviour Assessment Yes No animals of significance, environmental considerations such Specific Behaviour Monitor Yes No as bed positioning. D.B.S.R.S. Yes No (Dementia Behaviour Severity Rating Scale) 17. SPIRITUAL Score: NA Spiritual needs identified Yes No Management Chart in place Yes No Goals Refer to Management Chart for each behaviour separately To provide for Dawn’s spiritual needs within eg aggression, verbal disruption etc. her new environment. Behaviours identified Interventions eg preferred services of worship, clergy, Difficult – Resistive to carers prayer times, icons, medals, position of bible/spiritual Aggression literature and special days. Demanding Chapel services every Sunday. At risk of absconding Grief and Loss Goal: 15. INTEREST AND ACTIVITIES Encourage Dawn to verbalise her feelings of Goals: loss. Provide meaningful activity to assist in Interventions eg. enablements of coping such as building self-esteem. counselling, company, comforting and time alone Encourage involvement in activities. Prevent Counselling with psychiatrist and time with Social Isolation. family and friends. Interventions Emotionally Calming eg validation, doll, water, music 18. SOCIAL AND FAMILY therapies. Family visits Yes No Encourage Dawn to do her own washing, Specify (who frequency, special considerations) ironing etc nd Involve Dawn in social outings and exercise Brother x 2 weekly classes Encourage visits from friends Mental Stimulation/Cognitive eg quizzes newspaper, jigsaw, Carer input, needs and role and cards. Encourage participation in Dawn’s care. Photos of her family/friends – talk about places they went to.
5 Name: Dawn Schmidt D.O.B. 28-12-1954 Room: Wattle 195 Medical: Dr Paul
Date 3/4/05 Signature: P Rogers Review Date: Signature:
6