Time-dependent changes of hyperdense artery sign morphology and structure in acute stroke, study on 270 patients
Slaven Pikija, MD*a; Jozef Magdic, MDb; Peter Unterkreuter, MDc; J. Sebastian Mutzenbach,
MDa; Friedrich Weymayr, MDd; Johann Sellner, MDa aDepartment of Neurology, Christian Doppler Medical Centre, Paracelsus Medical University
Salzburg, Salzburg, Austria bDepartment of Neurology, Univerzitentni Klinicni Center Maribor, Maribor, Slovenia cDepartment of Neurology, Bezirkkrankehaus Lienz, Lienz, Austria dDivision of Neuroradiology, Christian Doppler Medical Centre, Paracelsus Medical
University Salzburg, Salzburg, Austria
Address for correspondence: Slaven Pikija, MD
Christian Doppler Klinik, Paracelsus Medical University,
Salzburg, Austria
Phone: +43-662-4483-3001
Fax: +43 662 4483 3004
e-mail: [email protected]
Total word count (text, references, tables): 2743
Tables: 3
Figures: 2
Disclosure: Authors have nothing to disclose
Key words: ischemic stroke, hyperdense artery, computed tomography
1 Abstract
Background and Purpose
We assessed the hypothesis that intracranial embolic material undergoes time-dependent changes short after stroke onset.
Methods
This is a retrospective study of consecutive acute stroke patients with sign of hyperdense artery (HA) as seen on non-enhanced CT (NECT) admitted to three stroke centers. Patient’s demographics, stroke severity according to national institute of health stroke scale (NIHSS), time to NECT after symptom onset, blood parameters on admission and stroke etiology according to TOAST criteria were collected. Occlusion site, density of HA expressed in
Hounsfield units (HU) and density of contralateral non-affected artery, area and length of HA was measured by two blinded stroke neurologist on the NECT images. Correlation of relative density (rHU) (average HU of HA/average HU of non-affected artery), length and area of HA were collated with time elapsed since symptom onset as well with stroke etiology and various blood parameters.
Results
Total of 2.562 NECT were visually inspected for the presence of HA. The total of 270
(10.5%) patients exhibited HA. Twenty (7.4%) of patients had no known time of onset. Mean time to CT were 197±205 minutes. In the first 4.5 hours, medial cerebral artery proximal
(ACM-M1) rHU was negatively correlated with time. Clot length and area was positively correlated with time and large artery atherosclerotic strokes had the largest HAs.
Conclusions
2 In this three-center retrospective study consecutive acute stroke patients intraarterial clots have showed time-dependent changes in means of altered clot density, length and area. Our main findings warrants further prospective studies.
3 Introduction
Cerebral arterial occlusion with its dramatic clinical consequence seen as stroke syndrome is usually the final step of complex pathologic disturbance in hemostatic cascade. Physiological response of cerebral acceptor vessel is most likely manifold. Donor material fate in time- dependent manner is poorly understood. Logically, the local secretory and serum dependent anticoagulations mechanisms take place, along with complexly disturbed local hemodynamics making impact on donated clot.
Neuroimaging and histological studies have been successful in deducing composition of embolised material, but the origin of embolised material probably could not be deduced with available techniques, although controversies exists [1-3].
Nevertheless, the clot’s morphological properties and composition are of prognostic value, with reports showing that large and more hypodenser clots – as seen on non-enhanced CT images, are more resistant to intravenous lytic therapy [4, 5].
In order to recruit as many patients as possible we have performed the retrospective study in three stroke centers.
As the availability of intravenous thrombolytic therapy rises worldwide and keeping in mind that CT scan is readily employed in decision tree of acute management of stroke patients we have pursued to further elucidate morphological and composition properties of cerebral embolic material with emphasis of time-dependent evolution.
4 Subjects and methods
We retrospectively reviewed the consecutive stroke patients non-enhanced CTs (NECT) images from three stroke centers, the Christian-Doppler-Klinik Salzburg, Austria (CDK) , the department of Neurology, University Clinical Center Maribor, Slovenia (MB) and
Department of Neurology, Bezirkkrankenhaus Lienz, Lienz (LZ).
Inclusion criteria for our study were: age≥18 years and NECT available for inspection on acute stroke presentation. Exclusion criteria were: acute brain hemorrhage, brain tumor or other non-stroke related pathology seen on NECT.
Usual demographic data were collected; additionally to usual blood profile we have recorded
HgbA1c and acute fibrinogen values. Stroke subtypes were assessed by investigators using
Trial of Org 10172 in Acute Treatment criteria [6].
Visual inspection was performed by two experienced stroke physicians, SP and JM who were blinded of clinical data. When in doubt of presence of hyperdense vessel sign, consensus was made.
CT scan parameters in CDK were:
CT scans were performed in multidetector CT scanner Somatom Definition AS plus
( 64 row) from Siemens, Erlangen.
Acquisition 40 x 0,6 mm, pitch of 0,55 mm .The CT scans were reconstructed into 4- mm
thick adjacent slices through the whole brain with the specifications of 120 kV, 250 mAs
( mean value , using automatic exposure control) and matrix size of 512x 512. The mean
equivalent dose was 1,5 mSV.
… differed across centers. Maribor and Lienz had 3 mm slice-thickness available.
5 Hyperdense artery sign was recognized as the area of hyperattenuating artery on NECT.
Hyperdense area was manually delineated in IMPAX software, the vessel and the side of affected vessel was recorded. Further measures were recorded: average Hounsfield unit (HU) density as reported by software in delineated area, area in mm2 of manually circumscribed hyperdensity, length in mm. Length was measured only when judged meaningful, i.e. it was not measured when only “dot sign” in M2 section of cerebral medial artery was seen.
In order to correct for hematocrit values, the density of the vessel contralateral to affected one was measured, in the case of basilar artery hyperdensity the measurement was in posterior cerebral artery.
From measured densities relative value HU ratio (rHU) (average HU of affected artery divided by average HU of contralateral/appropriate non-affected artery) was derived.
Statistical analysis…
6 Results
After screening of 2.562 NECT images total of 270 patients with acute ischemic stroke and visible hyperdense artery sign in non-contrast computed tomography of the head (NECT) were retrospectively collected from the consecutive patient pool of 3 stroke centers. The
CDK, MB and LZ contributed with 173 (64.1%), 58 (21.5%) and 39 (14.4%) patients, respectively. Of 270 patients, 20 (7.4%) were of unknown time of onset which left 250 patients for time-dependent analysis.
Within first 4.5 hours after symptom onset total of 202 (74.8%) patients had had NECT.
Patient’s demographics are given in Table 1.
Measurements of hyperdense artery sign as seen on NECT are given in Table 2 and further subdivided by each affected artery in Table 3.
Overall NIHSS value at admission is significantly correlated with the area of arterial hyperdensity, p=0.002 (N=258, rho=0.1921).
As expected NIHSS scale is significantly higher in ACM M1 occlusion than in other arteries, p<0.001 (Kruskall-Wallis test, chi2=11.008, df=1). Overall, these patients tend to be significantly older than those with other occlusion sites, p=0.036 (75.0 vs. 71.5 years of age), tend to have significantly less rHU (i.e. less denser embolic material), p<0.001 (rHU - 1.27 vs. 1.40). Furthermore, these patients had significantly lower HgbA1C and Triglycerides compared with other arteries, p<0.001 (5.54% vs. 6.10%) and p=0.037 (108.5 vs 126.6 mg/dl) for HgbA1C and triglycerides respectively, although higher fibrinogen levels, p=0.012 (396.2 vs. 356.7 mg/dl).
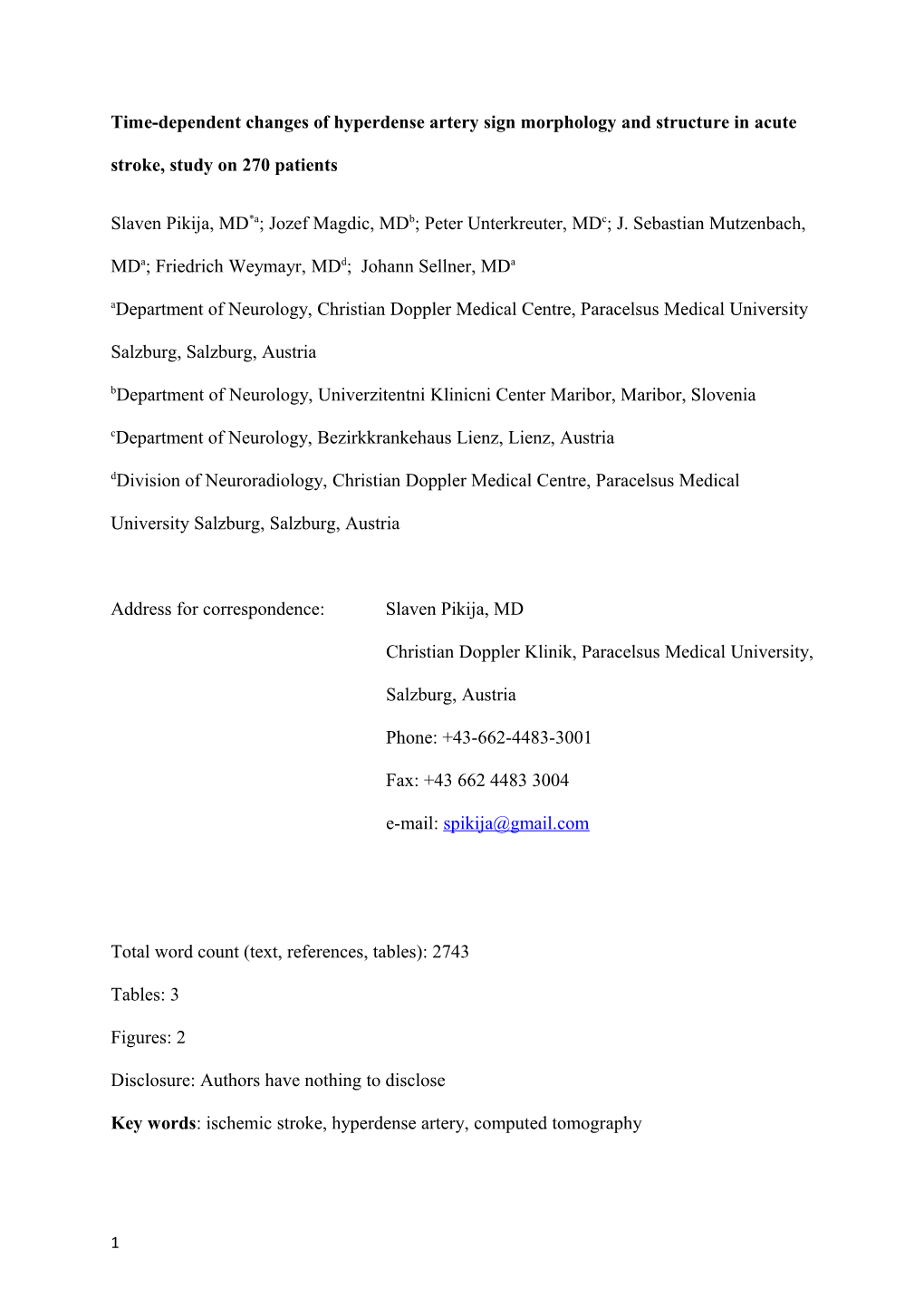
When looking in patients presenting in first 4.5 hours it seems that with passed time the MCA
M1 is less dense, and this correlation is significant at p=0.017 (N=81, F=5.96), Figure 1.
7 However it seems that after 4.5 hours density of the clot stabilizes, although data is available only for 28 patients.
Overall and especially in ACM M1 occlusion the embolic material seems to grow over time as relationship between CT scan time and measured area and length of embolic material is positively correlated and significant at p=0.03 (N=240) and p<0.001 (N=197), and p=0.001
(N=109) and p=0.001 (N=102) respectively.
Previous usage of anticoagulant (in 12 patients) is weakly associated with less denser material in MCA M1, p=0.060 (1.26 vs. 1.36).
MCA M2 embolic material contained the densest material of all examined vessels (not taking into account single ACA hyperdensity).
Overall, in first 4.5 hours fibrinogen levels are negatively associated with embolic material area and length p=0.016 (N=180, F=5.96) and p=0.017 (N=150, F=5.81) respectively, meaning that embolic material tends to be larger in patients with lower fibrinogen level.
Although the stroke etiology was not correlated with rHU, the clot’s length (N=164, F=4.81, p=0.001) and area (N=192, F=3.17, p=0.015) in the first 4.5 hours differ significantly between stroke etiologies, the largest and biggest clots been in LAA etiology group, Figure 2.
Site of occlusion was not different across stroke etiologies.
8 Discussion
Density of thrombus as seen on NECT is showed to predict composition of retrieved clots [3], predict revascularization efficacy [4] and is possibly not associated with stroke etiology [1, 2,
7]. It was also shown that clot length predicts outcome after intravenous thrombolysis, i.e. larger thrombi are less susceptible to lysis [5]. Accordingly, the characteristics of intraarterial embolic material in acute stroke is of potentially great interest for stroke physicians. The anatomical site, composition and spread of clot in various arteries could be used in decision making process for further treatment of the patient.
NECT is the fast, widely available and readily used method in acute stroke management and aside serving as “tool of exclusion” for thrombolysis/intervention, it could provide additional useful information regarding clot susceptibility to lysis.
Traditionally, the clots composed of red cell material are considered to be fresh, less compact and hyperdenser than fibrin-rich clots. It is assumed that red blood cells, at least after local plaque rupture in coronary vessels, build proximal and distal of fibrin-thrombocyte rich nidus
(Jang 1988). The similar mechanism could be in place in embolized clots with one study indicating interspersed formations of fibrin-platelet rich depostits with linear collections of nucleated cells and erythrocyte regions (Marder 2006) possibly revealing complex local hemodynamics around clot material.
It could be reasonably assumed that initial clot material changes its composition and morphology over time. Acceptor vessel probably undergoes multitude of hemodynamic and secretory changes in local milieu (REFSSSS). Proximal and distal apposition of new embolic material, endolytic processes take place in course of the time, possibly dissolving less compact thrombus material and leaving place for fibrin meshwork.
9 We have found indirect evidence of clot metamorphosis in acute stroke patients. According to our results ACM M1 clots tends to lose its density in the first 4.5 hours, however this effect stabilizes after this time point possibly achieving equilibrium point. Loss of density is attributed to build up of fibrin-platelet rich layers. Clot expansion and loss of density i.e. build up of fibrin-platelet rich layers could be responsible for negative correlation of fibrinogen levels with thrombus length and area. Changes in clot density over time was previously showed by Topcuoglu et al. [7], in their sample the densities of clot tend to drop in absolute
HU values as seen on control CT imaging. Density of clot as seen on NECT correlates directly to percentage of clots RBCs. Loss of density after embolism in ACM M1 occlusion is probably multifactorial and we could hypothesise that relatively larger vessel diameter is responsible to better wash-out of clots degradations products or better availability of endolytic enzymes.
According to our results, distal thrombi were more hyperdense. We could speculate that initial clot material provide fertile ground for immediate RBC build up possibly on the distal surface were is expected that flow is slower. What happened next with clot layering is open to discussion, however our indirect evidence showing that clot expands and along usage of fibrinogen point that clots are predominantly growing in fibrin-platelet rich layers.
Shobha et al [5] have found that longer clots persist even after intravenous thrombolysis.
Clots independent from artery location in our sample tend to grow in length and area over time. Also the length and area of clot according to our data could point to stroke etiology, the largest and longest thrombi been in LAA group and the smallest and shortest clots found in
UNK group, the findings contradictory of previous reports (Cho KH Stroke 2005) in which
CE clots are bigger. Clots originally derived from LAA pathologies are traditionally considered as fibrin-thrombocyte rich thrombi, i.e. white thrombi that could provide fertile local milieu for further thrombus build-up.
10 The group of patients without known stroke mechanism had the smallest clots, the reason of which is open to speculations.
Limitations of our joint study are many. Our patient cohort is retrospective, various scan parameters and various slice thicknesses were used in patients workup. Additionally, presumption that time dependent changes could be approximated from various patients is subjected to biases. Ideally each patient should be prospectively followed with NECT on fixed time points. However such approach is flawed with nowadays availability of thrombolysis/intervention procedures thus making such observations of natural clot evolution virtually impossible.
In conclusion, our three-center retrospective study on moderate-sized cohort of consecutive acute stroke patients had showed that metamorphosis in composition and morphology of donated embolic material do occur in acceptor artery and it is most likely time-dependent, possibly reflecting ongoing local (pato)physiological processes.
Larger, prospective studies are needed to confirm our findings and to make correlations with radiological and patients outcomes.
11 N=270 ACM M1 first 4.5 hours (N=) Age 75 (65-84) Gender (Female) 151 (55.9) Time to CT from symptom onset (min)Ω 197±205 Prior Stroke/TIA 34 (12.6) PAVK 21 (7.8) Atrial fib. 131 (48.7) Diabetes 44 (16.3) Carotid Stenosis (>50%) 34 (12.6) Cardial failure 39 (14.5) Antithrombotic th. 90 (33.3) Antikoagulant 26 (9.6) Novel Antikoagulant 2 (0.7) Thrombolysis 162 (60.0) Intervention 71 (26.3) Thrombolysis+Intervention 58 (21.5) NIHSS* 16 (10-20) TOAST etiology Cardioembolic 137 (50.7) Unknown/Other 71 (26.3) Large artery atheroscl. 37 (13.7) Dissection 13 (4.8) Undetermined 12 (4.4) Blood Sugar§ 131.4±42.6 HgbA1C† 5.75±0.88 Cholesterol‡ 180.3±43.3 Triglycerides£ 118.5±66.5 HDL¥ 51.4±16.2 LDL¥ 110.9±37.0 Fibrinogen€ 374.8±123.2 Data are mean±standard deviation, number(percentiles) or median(interquartile range, 25%-
75%).
Ω Onset time not known in 20 (7.4%) patients; *NIHSS missing for 2 (0.7%) patients;
§Blood sugar data missing for 1 (0.4%) patient; †HgbA1C missing for 111 (41%) patients;
‡Cholesterol data missing for 35 (12.9%) patients; £Triglycerides data missing for 33 (12.2%) patients; ¥HDL and LDL data missing for 37 (12.4%) patients; €Fibrinogen data missing for
23 (8.5%) patients
12 Table 1. Characteristics of 270 acute ischemic stroke patients with intracranial artery hyperdense sign on non-contrast computed tomography of the head.
13 N=270 Vessel affected Middle cerebral artery (MCA) 188 (88.9) MCA - M1 segment 118 (62.7) MCA - M2 segment 70 (37.2) Posterior cerebral artery (PCA) 5 (2.4) Anterior cerebral artery (ACA) 1 (0.5) Basilar artery 10 (4.7) Vertebral artery (VA) 7 (3.3) Other arteries 1 (0.5) Vessel Side – Right (ACM, ACP, ACA and VA) 99 (50.51) HU Average (Clot density in Hounsfield Units) 46.8±5.1 HU Ratio affected/non-affected side 1.34±0.25 Length of hyperdensity in mm* 16.3±11.1 Area of hyperdensity in mm2† 38.9±33.9 Data are mean±standard deviation, number(percentiles) or median(interquartile range, 25%-
75%).
*Length were not calculated in 57 (21%) of patients; †Hyperdense artery area measurement were not available in 10(3.7%) of patients.
HU- Hounsfield units
Table 2. Measurements of intracranial artery hyperdense sign on non-contrast computed tomography of the head in 270 consecutive patients with acute ischemic stroke.
14 MCA M1 MCA M2 ACP ACA BA VA (N=118) (N=70) (N=5) (N=1) (N=10) (N=7) HU Average 47.1±4.5 45.7±4.7 44.2±7.6 52.0±0 52.8±4.4 53.2±3.6 HU Ratio 1.27±0.18 1.32±0.22 1.28±0.11 1.35±0 1.31±0.19 1.31±0.24 Length of 17.9±13.4 14.8±8.8 12.2±8.6 10.0±0 - 7.7±0 hyperdensity in mm* Area of 46.2±37.7 31.1±34.8 11.2±10.2 25.3±0 20.9±8.7 40.1±31.1 hyperdensity in mm2† *Length not reported in 8, 28, 3, 10, 6 for MCA M1, MCA M2, PCA, BA and VA respectively
MCA – middle cerebral artery, M1 – first segment of MCA, M2 – second segment of MCA,
ACA – anterior cerebral artery, PCA – posterior cerebra artery, BA – basilar artery. HU –
Hounsfield units.
Table 3. Measurements of hyperdensities in varios cerebral vessels in 270 acute stroke patients.
15 16 p=0.017, N=81. symptom <= time4.5Hours, from material, segment onset M1 embolic artery cerebral of middle with fromonsetdensity oftimepassed symptom to CT Figure 1.Correlation Time to NECT in minutes
50 100 150 200 250 1 HU Ratio(HU AffectedArtery / HU Non-Affected Artery) 1.2 1.4 1.6 1.8 References:
1. Marder, V.J., et al., Analysis of thrombi retrieved from cerebral arteries of patients with acute ischemic stroke. Stroke, 2006. 37(8): p. 2086-93. 2. Niesten, J.M., et al., Relationship between thrombus attenuation and different stroke subtypes. Neuroradiology, 2013. 55(9): p. 1071-9. 3. Liebeskind, D.S., et al., CT and MRI early vessel signs reflect clot composition in acute stroke. Stroke, 2011. 42(5): p. 1237-43. 4. Moftakhar, P., et al., Density of thrombus on admission CT predicts revascularization efficacy in large vessel occlusion acute ischemic stroke. Stroke, 2013. 44(1): p. 243-5. 5. Shobha, N., et al., Measurement of length of hyperdense MCA sign in acute ischemic stroke predicts disappearance after IV tPA. J Neuroimaging, 2014. 24(1): p. 7-10. 6. Kolominsky-Rabas, P.L., et al., Epidemiology of ischemic stroke subtypes according to TOAST criteria: incidence, recurrence, and long-term survival in ischemic stroke subtypes: a population-based study. Stroke, 2001. 32(12): p. 2735-40. 7. Topcuoglu, M.A., E.M. Arsava, and E. Akpinar, Clot Characteristics on Computed Tomography and Response to Thrombolysis in Acute Middle Cerebral Artery Stroke. J Stroke Cerebrovasc Dis, 2015.
17