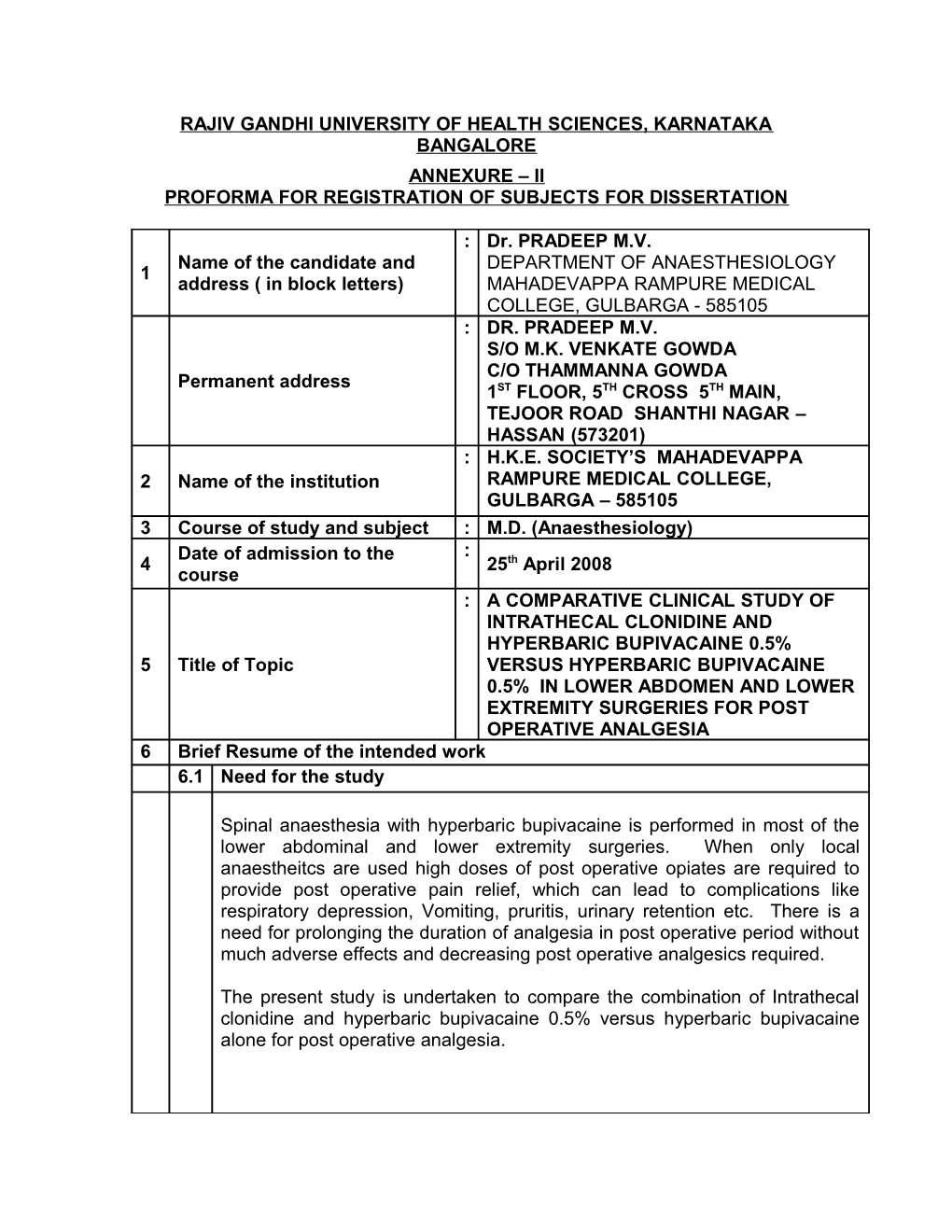
RAJIV GANDHI UNIVERSITY OF HEALTH SCIENCES, KARNATAKA BANGALORE ANNEXURE – II PROFORMA FOR REGISTRATION OF SUBJECTS FOR DISSERTATION
: Dr. PRADEEP M.V. Name of the candidate and DEPARTMENT OF ANAESTHESIOLOGY 1 address ( in block letters) MAHADEVAPPA RAMPURE MEDICAL COLLEGE, GULBARGA - 585105 : DR. PRADEEP M.V. S/O M.K. VENKATE GOWDA C/O THAMMANNA GOWDA Permanent address 1ST FLOOR, 5TH CROSS 5TH MAIN, TEJOOR ROAD SHANTHI NAGAR – HASSAN (573201) : H.K.E. SOCIETY’S MAHADEVAPPA 2 Name of the institution RAMPURE MEDICAL COLLEGE, GULBARGA – 585105 3 Course of study and subject : M.D. (Anaesthesiology) Date of admission to the : 4 25th April 2008 course : A COMPARATIVE CLINICAL STUDY OF INTRATHECAL CLONIDINE AND HYPERBARIC BUPIVACAINE 0.5% 5 Title of Topic VERSUS HYPERBARIC BUPIVACAINE 0.5% IN LOWER ABDOMEN AND LOWER EXTREMITY SURGERIES FOR POST OPERATIVE ANALGESIA 6 Brief Resume of the intended work 6.1 Need for the study
Spinal anaesthesia with hyperbaric bupivacaine is performed in most of the lower abdominal and lower extremity surgeries. When only local anaestheitcs are used high doses of post operative opiates are required to provide post operative pain relief, which can lead to complications like respiratory depression, Vomiting, pruritis, urinary retention etc. There is a need for prolonging the duration of analgesia in post operative period without much adverse effects and decreasing post operative analgesics required.
The present study is undertaken to compare the combination of Intrathecal clonidine and hyperbaric bupivacaine 0.5% versus hyperbaric bupivacaine alone for post operative analgesia. 6.2 Review of Literature
Grace D, Bunting H, Milligan KR, Fee JPH (1995). Conducted a randomized study for post operative analgesia on 90 patients, undergoing total hip replacement under bupivacaine spinal anesthesia. Group B -30 patients (isobaric bupivacaine 0.5%. (2.75ml) + 0.9 sodium chloride (1ml) Group-BM 30 patients (isobaric bupivacaine 0.5% (2.75ml) and morphine 0.5mg + 0.9% sodium chloride (0.75ml) and Group BMC – 30 patients (Isobaric bupivacaine 0.5% (2.75ml) + morphine 0.5mg (0.25ml) + clonidine 75gm (0.5ml) + 0.9% sodium chloride (0.25ml). They concluded that patient controlled morphine requirement were significantly reduced in post operation by group BMC although the incidence of MAP was significantly low in group-BMC. The incidence of emesis similar in group BMC and group-BM as was significantly more than group-B1.
Dobrydnjov, Axelsson K, Samarutel J, Holmstron B (2002). Conducted a double –blind, Randomized study on 45 ASA-I-III orthopaedic patients scheduled for osteosynthsis of a traumatic femur fracture. They were randomized into 3 groups, one group (15 patients) received 15mg plain bupivacaine intrathecally (Group-B), or an Intrathecal mixture of plain bupivacaine 15mg and clonidine 150gm (Group-CIT). In group CPO oral clonidine 150mg was administered 60 minutes before intrathecal injection of bupivacaine 15mg. They concluded that addition of Intrathecal clonidine prolonged analgesia and decreased morphine consumption post operatively more than oral clonidine, Hypotension was more pronounced after oral than intrathecal clonidine2.
Brian D, Sites, et al (2003). Conducted study on 81 ASA physical status I-III patients, undergoing either a single or bilateral total knee orthoplasty and were randomized into 4 groups with the following 2ml solutions added to 15mg of hyperbaric bupivacaine: (1) Sterile saline, (2) Morphine (250 gm), (3) Morphine (250gm) with clonidine (25gm) and (4) Morphine (250gm) with clonidine (75gm). At 1,2,4,6,12, and 24 hours post operatively, measured the VAS, cumulative intravenous morphine consumption, Haemodynamics, nausea, ancillary drugs and side effects. They concluded that the co-administration of Intrathecal clonidine and morphine decreases the 24 hrs IV morphine consumption and improves the 24 hours VAS score when compared with Intrathecal morphine alone3.
Baker, Amir et al (2004). Conducted study on 30 elderly patients for post operative analgesia after surgical repair of traumatic hip fracture. Patients were randomized into two groups. Group ISO (15 patients) received clonidine 150 gm + 1ml of 0.9% normal saline and Group HYPER (15 patients) received clonidine 150 gm + 1ml of 10% glucose. Yielding a 5% HYPER solution. The drug was administered in recovery room via IT catheter when patients complained of pain after the operation. They concluded that the analgesic effect over time was more pronounced in the ISO group than in HYPER group4.
Van Tuijl I, Van klei W.A van der werff, D.B.M; Kalkman, C.J. (2006). Conducted a randomized controlled double blind trial on 106 women patients were randomly allocated to receive spinal anaesthesia using either bupivacaine 0.5% (2.2ml) heavy with 0.5ml normal saline 0.9% (total 2.7 ml) - Group B, or bupivacaine 0.5% (2.2ml) heavy with clonidine (75gm) in 0.5ml normal saline 0.9% (total 2.7ml) – group BC,. They concluded that the addition of clonidine to hyperbaric bupivacaine prolongs spinal anaesthesia after caesarean section and improves early analgesia. No clinical relevant maternal or neonatal side effects were detected5.
Lavand’Homme, Patricia M et al (2008). Conducted study on 96 parturients undergoing elective cesarean section were randomly received Intrathecal bupivacaine – sufentanyl (BS group). Bupivacaine sufentanyl-clonidine 75gm (BSC group) or Bupivacaine – clonidine 150gm (BC group). The post operative analgesic effect of clonidine was assessed by clinical pain score (VAS) and rescue analgesics used post operatively. They concluded that the use of rescue analgesics was significantly delayed in BSC group compared to other groups6.
6.3 Objectives of the study
1. To evaluate the post operative analgesic effect of Intrathecal clonidine and hyperbaric bupivacaine 0.5%. 2. To know the incidence of adverse effects and complications of adding clonidine to hyperbaric bupivacaine for Intrathecal administration. 7 Materials and methods 7.1 Source of data
Patients undergoing elective and emergency procedures at Basaveshwar Teaching and General Hospital, Sangameshwar Hospital, Gulbarga attached to Mahadevappa Rampure Medical College, Gulbarga
7.2 Methods of collection of data ( including sampling procedure, if any)
Inclusion criteria All patients belonging to age group 18-60 years with ASA grade I and grade II undergoing elective and emergency operative procedure for lower abdomen and lower extremity. Exclusion criteria 1. Patients with history of bleeding disorders or patients on anticoagulant therapy 2. Patient’s refusal 3. Any contraindication to spinal anesthesia 4. Patients with mental illness 5. Patients with severe systemic disease, metabolic disorders, congenital or cardiovascular disorders
Mode of selection of cases: Random
Allocation to different groups
Group B: Patients receiving 2.5ml of hyperbaric bupivacaine 0.5% along with 0.5ml of normal saline (total volume of 3ml)
Group BC: Patients receiving 2.5ml hyperbaric bupivacaine 0.5% with clonidine 75gm, (Total volume of 3ml) Number of cases belonging to each group - 50 Parameters of comparison: Intraoperative: Time of onset of analgesia (Sensory – time taken from injection of drug to onset of analgesia at T10 level by pinprick method) Maximum level of analgesia achieved Time taken for onset of motor blockade (Time taken from injection of drug to onset of grade-I motor block on bromage scale). Total duration of surgery
Heart Rate, Blood pressure, Respiratory Rate, SPO2 Postoperative:
Heart Rate, Blood pressure, Respiratory Rate, SPO2 Total duration of analgesia (Time taken from the onset of analgesia to the point where the patient complained of pain in the operated site requiring rescue analgesics (VAS > 5) Visual analog scale, sedation score. Rescue analgesics. Nausea vomiting and other side effects
In this study the data analysis is done by – large sample “Z” test and “Chi square test” Does the study require any investigation or intervention to be 7.3 conducted on patients or other humans or animals? if so please describe briefly Yes. The study requires the following investigations CBC, Blood grouping Urine routine (for albumin, sugar and microscopy) ESR Bleeding time, Clotting time RBS, Blood urea, serum creatinine Chest X-ray, ECG 7.4 Has ethical clearance been obtained from your institution in case of 7.3 ? Yes. Ethical clearance has been obtained from “Ethical clearance committee” of the institution. 8 List of References 1. Grace D, Bunting H, Milligan K.R, Fee J.P.H. Postoperative analgesia after co-administration of clonidine and morphine by the Intrathecal route in patients undergoing Hip replacement. Anesth Analg 1995; 80: 86-91. 2. Dobrydnjov, Axelsson K, Samarutel J, and Holmstrom B. Postoperative pain relief following Intrathecal bupivacaine combined with Intrathecal or oral clonidine. Acta Anaesthesiologica Scandinavica. 2002; 46 (7): 806-814. 3. Brian D. Sites, Michael Beach, Russell Biggs, Christopher Rohan, Christopher Wiley, Athos Rassias, Janice Gregory. Intrathecal clonidine added to a bupivacaine – morphine spinal anesthetic improves postoperative analgesia for total knee arthroplasty. Anesth Analg 2003; 96:1083-1088. 4. Baker, Amir, Klimscha, Walter, Eisenach, James C, Xin-Hui, Wilding, Eckart et al. Intrathecal clonidine for postoperative analgesia in elderly patients: The influence of Baricity on Hemodynamic and analgesic effects. Pain Medicine. 2004 July; 99 (1): 128-134. 5. Van Tuijl, l, Van Klei W.A, Van Der Werff D.B.M, Kalkman C.J. The effect of addition of Intrathecal clonidine to hyperbaric bupivacaine on postoperative pain and morphine requirements after caesarean section: a randomized controlled trial. British Journal of Anesthesia. 2006; 97 (3): 365-370. 6. lavand’homme, Patricia M, Roelants, Fabienne,Waterloos, Hilde RN, Collet, Valerie, De Kock Marc F. An evaluation of the postoperative antihyperalgesic and analgesic effects of Intrathecal clonidine administered during elective cesarean delivery. Obstetric Anesthesiology. 2008; 107(3): 948-955. 9 Signature of Candidate
This study is undertaken to evaluate the efficacy 10 Remarks of guide of clonidine in prolonging the analgesia after subarachnoid block with bupivacaine
11 11.1 Name and designation of the
Guide Dr. K.SRI RAMAMURTHY M.D. PROFESSOR DEPARTMENT OF ANAESTHESIOLOGY, M.R. MEDICAL COLLEGE, GULBARGA
11.2 Signature
11.3 Co- guide (if any)
11.4 Signature
Dr. BASAVARAJ V. MODI 11.5 Head of the M.D. Department PROFESSOR AND HOD DEPARTMENT OF ANAESTHESIOLOGY M.R.MEDICAL COLLEGE, GULBARGA
11.6 Signature
12 12.1 Remarks of the Chairman and Principal
12.2 Signature