0666d73c299e1a1df1b16f7db322595f.doc Page 1 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
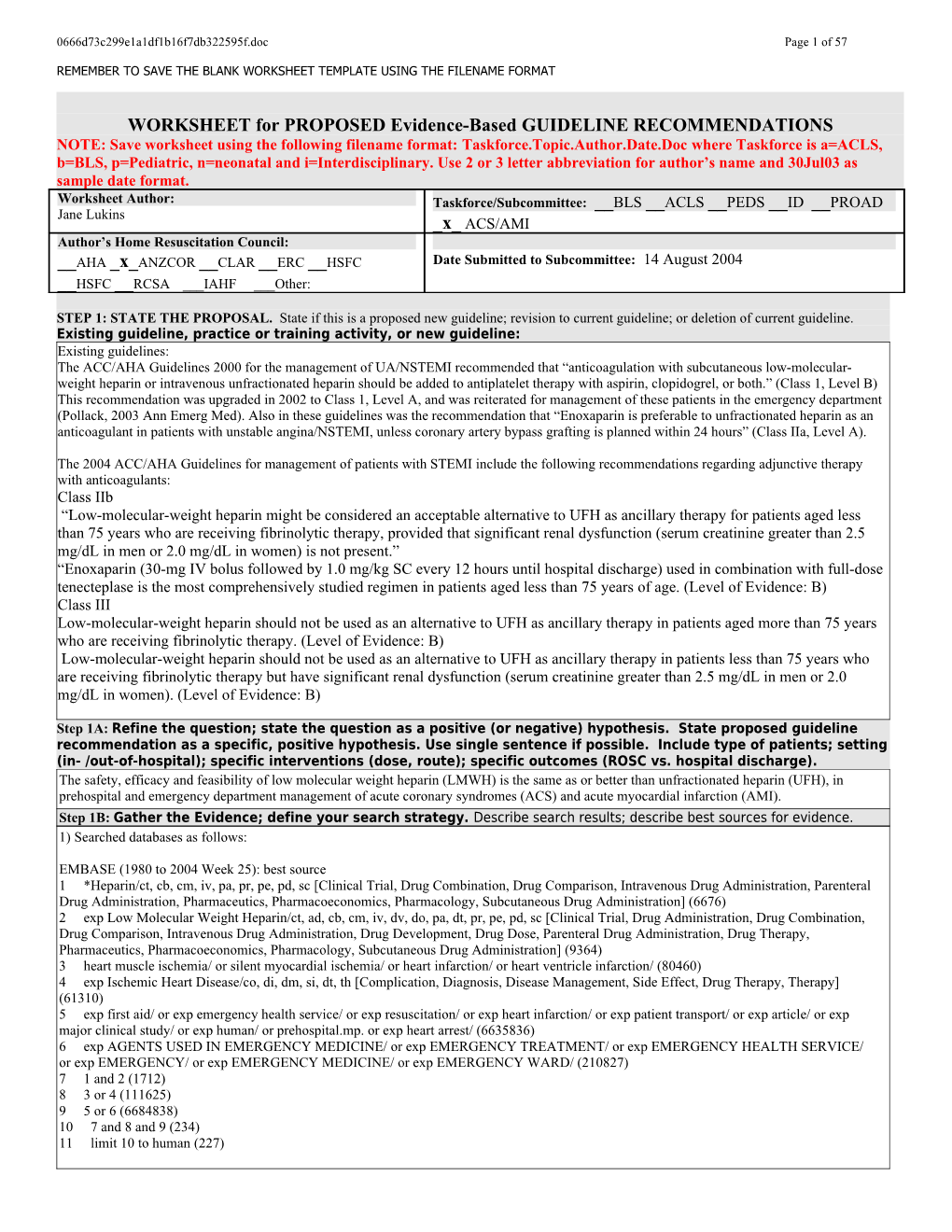
WORKSHEET for PROPOSED Evidence-Based GUIDELINE RECOMMENDATIONS NOTE: Save worksheet using the following filename format: Taskforce.Topic.Author.Date.Doc where Taskforce is a=ACLS, b=BLS, p=Pediatric, n=neonatal and i=Interdisciplinary. Use 2 or 3 letter abbreviation for author’s name and 30Jul03 as sample date format. Worksheet Author: Taskforce/Subcommittee: __BLS __ACLS __PEDS __ID __PROAD Jane Lukins _x_ ACS/AMI Author’s Home Resuscitation Council: __AHA _x_ANZCOR __CLAR __ERC __HSFC Date Submitted to Subcommittee: 14 August 2004 __HSFC __RCSA ___IAHF ___Other:
STEP 1: STATE THE PROPOSAL. State if this is a proposed new guideline; revision to current guideline; or deletion of current guideline. Existing guideline, practice or training activity, or new guideline: Existing guidelines: The ACC/AHA Guidelines 2000 for the management of UA/NSTEMI recommended that “anticoagulation with subcutaneous low-molecular- weight heparin or intravenous unfractionated heparin should be added to antiplatelet therapy with aspirin, clopidogrel, or both.” (Class 1, Level B) This recommendation was upgraded in 2002 to Class 1, Level A, and was reiterated for management of these patients in the emergency department (Pollack, 2003 Ann Emerg Med). Also in these guidelines was the recommendation that “Enoxaparin is preferable to unfractionated heparin as an anticoagulant in patients with unstable angina/NSTEMI, unless coronary artery bypass grafting is planned within 24 hours” (Class IIa, Level A).
The 2004 ACC/AHA Guidelines for management of patients with STEMI include the following recommendations regarding adjunctive therapy with anticoagulants: Class IIb “Low-molecular-weight heparin might be considered an acceptable alternative to UFH as ancillary therapy for patients aged less than 75 years who are receiving fibrinolytic therapy, provided that significant renal dysfunction (serum creatinine greater than 2.5 mg/dL in men or 2.0 mg/dL in women) is not present.” “Enoxaparin (30-mg IV bolus followed by 1.0 mg/kg SC every 12 hours until hospital discharge) used in combination with full-dose tenecteplase is the most comprehensively studied regimen in patients aged less than 75 years of age. (Level of Evidence: B) Class III Low-molecular-weight heparin should not be used as an alternative to UFH as ancillary therapy in patients aged more than 75 years who are receiving fibrinolytic therapy. (Level of Evidence: B) Low-molecular-weight heparin should not be used as an alternative to UFH as ancillary therapy in patients less than 75 years who are receiving fibrinolytic therapy but have significant renal dysfunction (serum creatinine greater than 2.5 mg/dL in men or 2.0 mg/dL in women). (Level of Evidence: B)
Step 1A: Refine the question; state the question as a positive (or negative) hypothesis. State proposed guideline recommendation as a specific, positive hypothesis. Use single sentence if possible. Include type of patients; setting (in- /out-of-hospital); specific interventions (dose, route); specific outcomes (ROSC vs. hospital discharge). The safety, efficacy and feasibility of low molecular weight heparin (LMWH) is the same as or better than unfractionated heparin (UFH), in prehospital and emergency department management of acute coronary syndromes (ACS) and acute myocardial infarction (AMI). Step 1B: Gather the Evidence; define your search strategy. Describe search results; describe best sources for evidence. 1) Searched databases as follows:
EMBASE (1980 to 2004 Week 25): best source 1 *Heparin/ct, cb, cm, iv, pa, pr, pe, pd, sc [Clinical Trial, Drug Combination, Drug Comparison, Intravenous Drug Administration, Parenteral Drug Administration, Pharmaceutics, Pharmacoeconomics, Pharmacology, Subcutaneous Drug Administration] (6676) 2 exp Low Molecular Weight Heparin/ct, ad, cb, cm, iv, dv, do, pa, dt, pr, pe, pd, sc [Clinical Trial, Drug Administration, Drug Combination, Drug Comparison, Intravenous Drug Administration, Drug Development, Drug Dose, Parenteral Drug Administration, Drug Therapy, Pharmaceutics, Pharmacoeconomics, Pharmacology, Subcutaneous Drug Administration] (9364) 3 heart muscle ischemia/ or silent myocardial ischemia/ or heart infarction/ or heart ventricle infarction/ (80460) 4 exp Ischemic Heart Disease/co, di, dm, si, dt, th [Complication, Diagnosis, Disease Management, Side Effect, Drug Therapy, Therapy] (61310) 5 exp first aid/ or exp emergency health service/ or exp resuscitation/ or exp heart infarction/ or exp patient transport/ or exp article/ or exp major clinical study/ or exp human/ or prehospital.mp. or exp heart arrest/ (6635836) 6 exp AGENTS USED IN EMERGENCY MEDICINE/ or exp EMERGENCY TREATMENT/ or exp EMERGENCY HEALTH SERVICE/ or exp EMERGENCY/ or exp EMERGENCY MEDICINE/ or exp EMERGENCY WARD/ (210827) 7 1 and 2 (1712) 8 3 or 4 (111625) 9 5 or 6 (6684838) 10 7 and 8 and 9 (234) 11 limit 10 to human (227)
0666d73c299e1a1df1b16f7db322595f.doc Page 2 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
MEDLINE (1966 – June week 3 2004): 1 heparin/ and exp heparin, low-molecular-weight/ (1555) 2 myocardial ischemia/ or coronary disease/ or exp angina pectoris/ or exp myocardial infarction/ (212837) 3 1 and 2 (170) 4 limit 3 to human (169) Note: If also tried to combine with Emergency Medicine or Prehospital terms, no articles were found
Cochrane database (CDSR, ACP Journal Club, DARE, CCTR) 1 heparin/ and exp heparin, low-molecular-weight/ (290) 2 myocardial ischemia/ or coronary disease/ or exp angina pectoris/ or exp myocardial infarction/ (10371) 3 1 and 2 (50)
AHA Endnote 7 Master Library 1 searched all fields that contain acute coronary syndrome or myocardial infarction or myocardial ischemia or angina (1453) 2 searched within 1 all fields that contain heparin or low molecular weight heparin or enoxaparin or fraxaparin or dalteparin (150) 3 searched within 2, all fields that contain emergency or prehospital (17)
2) Combined the end results of the above database searches in my own Endnote library where I deleted duplicates. 3) Reviewed titles electronically and deleted those clearly unrelated to question 4) Identified 236 articles. Reviewed abstracts electronically excluded 126 using criteria below. 5) Of 110 articles obtained, 50 were suitable for critical appraisal and inclusion in worksheet. 6) 4 additional articles obtained after initial worksheet completion, 3 were suitable for inclusion in worksheet. Total 53.
List electronic databases searched (at least AHA EndNote 7 Master library [http://ecc.heart.org/], Cochrane database for systematic reviews and Central Register of Controlled Trials [http://www.cochrane.org/], MEDLINE [http://www.ncbi.nlm.nih.gov/PubMed/ ], and Embase), and hand searches of journals, review articles, and books. Embase 1980 to 2004 Week 25 Medline 1966 to June Week 3 2004 Cochrane database (reviews and trials) AHA Endnote 7 Master Library Reference lists of articles hand searched to obtain other relevant clinical trials. • State major criteria you used to limit your search; state inclusion or exclusion criteria (e.g., only human studies with control group? no animal studies? N subjects > minimal number? type of methodology? peer-reviewed manuscripts only? no abstract-only studies?)
The searches were limited to human studies, peer and non-peer reviewed manuscripts cited in the world’s literature. Articles excluded were abstract only studies, all narrative reviews and published systematic reviews without a meta-analysis and those that had no relevance to emergency department or prehospital settings (Specifically, in-hospital studies more than 72 hours after patient presentation, post percutaneous angiography trials, trials investigating changes in coagulation factors without clinical end points and long-term outpatient care). • Number of articles/sources meeting criteria for further review: Create a citation marker for each study (use the author initials and date or Arabic numeral, e.g., “Cummins-1”). . If possible, please supply file of best references; EndNote 6+ required as reference manager using the ECC reference library.
Searches narrowed after title/ abstract review to 53 articles
STEP 2: ASSESS THE QUALITY OF EACH STUDY Step 2A: Determine the Level of Evidence. For each article/source from step 1, assign a level of evidence—based on study design and methodology. Level of Definitions Evidence (See manuscript for full details) Level 1 Randomized clinical trials or meta-analyses of multiple clinical trials with substantial treatment effects Level 2 Randomized clinical trials with smaller or less significant treatment effects Level 3 Prospective, controlled, non-randomized, cohort studies Level 4 Historic, non-randomized, cohort or case-control studies Level 5 Case series: patients compiled in serial fashion, lacking a control group Level 6 Animal studies or mechanical model studies Level 7 Extrapolations from existing data collected for other purposes, theoretical analyses Level 8 Rational conjecture (common sense); common practices accepted before evidence-based guidelines 0666d73c299e1a1df1b16f7db322595f.doc Page 3 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Step 2B: Critically assess each article/source in terms of research design and methods. Was the study well executed? Suggested criteria appear in the table below. Assess design and methods and provide an overall rating. Ratings apply within each Level; a Level 1 study can be excellent or poor as a clinical trial, just as a Level 6 study could be excellent or poor as an animal study. Where applicable, please use a superscripted code (shown below) to categorize the primary endpoint of each study. For more detailed explanations please see attached assessment form.
Component of Study and Rating Excellent Good Fair Poor Unsatisfactory Design & Highly appropriate Highly appropriate Adequate, Small or clearly Anecdotal, no sample or model, sample or model, design, but biased population controls, off randomized, proper randomized, proper possibly biased or model target end-points controls controls Methods AND OR OR OR OR Outstanding Outstanding accuracy, Adequate under Weakly defensible Not defensible in accuracy, precision, and data the in its class, limited its class, precision, and data collection in its class circumstances data or measures insufficient data collection in its or measures class
A = Return of spontaneous circulation C = Survival to hospital discharge B = Survival of event D = Intact neurological survival E = Other
Step 2C: Determine the direction of the results and the statistics: supportive? neutral? opposed?
DIRECTION of study by results & statistics: SUPPORT the proposal NEUTRAL OPPOSE the proposal Outcome of proposed guideline Outcome of proposed guideline Outcome of proposed guideline Results superior, to a clinically important no different from current inferior to current approach degree, to current approaches approach
Step 2D: Cross-tabulate assessed studies by a) level, b) quality and c) direction (ie, supporting or neutral/ opposing); combine and summarize. Exclude the Poor and Unsatisfactory studies. Sort the Excellent, Good, and Fair quality studies by both Level and Quality of evidence, and Direction of support in the summary grids below. Use citation marker (e.g. author/ date/source). In the Neutral or Opposing grid use bold font for Opposing studies to distinguish them from merely neutral studies. Where applicable, please use a superscripted code (shown below) to categorize the primary endpoint of each study. Supporting Evidence for UA/NSTEMI
The safety, efficacy and feasibility of low molecular weight heparin (LMWH) is the same as or better than unfractionated heparin (UFH), in prehospital and emergency department management of acute coronary syndromes (ACS) and acute myocardial infarction (AMI).
Magee(04)# k,l,s,t Excellent Petersen(04)# e,t,f,s Antman(99; 1)e Antman(99; 2)# e,g,s,t Antman(02)# e Cohen(97) e,t 0666d73c299e1a1df1b16f7db322595f.doc Page 4 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT e c
n Goodman(00; 2) e
d Good e,t Klein(03) f,k,p,s,t
i Campos(02)n,s,t O'Brien(00)i,u, v Goodman(03)
E f,g,e,s,t,v
f o Goodman(00; 1) y t
i e,t Bozovich(00)e,f,g l
a Fair Gurfinkel(95) Brosa(02)i,t u j,g,s,t Detournay(00)i,u
Q Malhotra (01; 1) Mark(98) i,u e,f,g,i,s,t,u Spinler(03)e,t Mattioli(99)e,j,t 1 2 3 4 5 6 7 8 Level of Evidence A = Return of spontaneous circulation B = Survival of event C = Survival to hospital discharge D = Intact neurological survival E = Composite (Death/MI±recurrent angina)F = Major hemorrhage G = Minor hemorrhage H = Bleeding post intervention/surgery I = Cost J = Recurrent ischaemia K = Myocardial Infarction L = Revascularisation M = Thrombotic marker difference N = Composite E + F (incl ICH) O = TIMI flow P = Mortality S = Safety T = Efficacy U = Feasibility V = +G2b3a inhibitor X = STEMI, no reperfusion Y = STEMI + Fibrinolytic therapy Z = STEMI + PCI Citations in italic = studies not performed in ED/Prehospital settings or intervention not initiated within 24 hours of qualifying symptom. * = Trial done in prehospital setting # = Meta-analysis Neutral or Opposing Evidence for UA/NSTEMI The safety, efficacy and feasibility of low molecular weight heparin (LMWH) is the same as or better than unfractionated heparin (UFH), in prehospital and emergency department management of acute coronary syndromes (ACS) and acute myocardial infarction (AMI). e c
n Eikelboom(00)#
e e,f,s,t
d Excellent Berkowitz(01)f i FRAIS
v Ferguson (04) Investigators(99)
E e,t,m,s e,f,s,t f
o Le Nguyen(01)#
y e,f,s,t t i l a u Good Blazing(04)e,f,s, Q Kovar(02)e,f,s,t,v t,v
Cohen(99)v Cohen(02)v,f,g Fair Gurfinkel(99)e,k Klein(97)e,f,g,s, Malhotra(01; Brieger(02)h,s Jones(02)h, t 2)# e,f,g,s,t Clark(00)h,s s Montalescot(03) e,f,g,m,s,t Suvarna(97)j,k,l, t 1 2 3 4 5 6 7 8 Level of Evidence A = Return of spontaneous circulation B = Survival of event C = Survival to hospital discharge D = Intact neurological survival E = Composite (Death/MI±recurrent angina)F = Major hemorrhage 0666d73c299e1a1df1b16f7db322595f.doc Page 5 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
G = minor hemorrhage H = Bleeding post intervention/surgery I = Cost J = Recurrent ischaemia K = Myocardial Infarction (outcome) L = Revascularisation M = Thrombotic marker difference N = Composite E + F (incl ICH) P = Mortality S = Safety T = Efficacy U = Feasibility V = +G2b3a inhibitor X = STEMI, no reperfusion Y = STEMI + Fibrinolytic therapy Z = STEMI + PCI Citations in italic = studies not performed in ED/Prehospital settings or intervention not initiated within 24 hours of qualifying symptom. * = Trial done in prehospital setting # = Meta-analysis
Supporting Evidence for STEMI
The safety, efficacy and feasibility of low molecular weight heparin (LMWH) is the same as or better than unfractionated heparin (UFH), in prehospital and emergency department management of acute coronary syndromes (ACS) and acute myocardial infarction (AMI). e c n e
d Excellent Theroux(03)# Wallentin(03; 2)* i e,j,k,t,f,g,s,y e,t,u,y,s v E
f o
y t i
l Baird(02)*e,y
a Good Van deWerf Wallentin(03; 1) Klein(03) u (01)e,j,k,l,n,s,t, k,o,s,t,y f,p,s,t Q y
Fair Cohen(00)e,t,x
1 2 3 4 5 6 7 8 Level of Evidence A = Return of spontaneous circulation B = Survival of event C = Survival to hospital discharge D = Intact neurological survival E = Composite (Death/MI±recurrent angina)F = Major hemorrhage G = minor hemorrhage H = Bleeding post intervention/surgery I = Cost J = Recurrent ischaemia K = Myocardial Infarction (outcome) L = Revascularisation M = Thrombotic marker difference N = Composite E + F (incl ICH) O = TIMI flow P = Mortality S = Safety T = Efficacy U = Feasibility V = +G2b3a inhibitor X = STEMI, no reperfusion Y = STEMI + Fibrinolytic therapy Z = STEMI + PCI Citations in italic = studies not performed in ED/Prehospital settings or intervention not initiated within 6 hours of STEMI onset. * = Trial done in prehospital setting # = Meta-analysis Neutral or Opposing Evidence for STEMI The safety, efficacy and feasibility of low molecular weight heparin (LMWH) is the same as or better than unfractionated heparin (UFH), in prehospital and emergency department management of acute coronary syndromes (ACS) and acute myocardial infarction (AMI). 0666d73c299e1a1df1b16f7db322595f.doc Page 6 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT e c n e
d Excellent Cohen(03)e,s,x i v E
f o
y t i l
a Good Kovar(02)e,f,s,t,
u Ross(01)s,t,y v Q
Fair Peters(01)f,s,y Dubois(03)s,t,y,z
1 2 3 4 5 6 7 8 Level of Evidence A = Return of spontaneous circulation B = Survival of event C = Survival to hospital discharge D = Intact neurological survival E = Composite (Death/MI±recurrent angina)F = Major hemorrhage G = minor hemorrhage H = Bleeding post intervention/surgery I = Cost J = Recurrent ischaemia K = Myocardial Infarction (outcome) L = Revascularisation M = Thrombotic marker difference N = Composite E + F (incl ICH) P = Mortality S = Safety T = Efficacy U = Feasibility V = +G2b3a inhibitor X = STEMI, no reperfusion Y = STEMI + Fibrinolytic therapy Z = STEMI + PCI Citations in italic = studies not performed in ED/Prehospital settings or intervention not initiated within 6 hours of STEMI onset. * = Trial done in prehospital setting # = Meta-analysis
STEP 3. DETERMINE THE CLASS OF RECOMMENDATION. Select from these summary definitions. CLASS CLINICAL DEFINITION REQUIRED LEVEL OF EVIDENCE Class I • Always acceptable, safe • One or more Level 1 studies are present (with rare Definitely recommended. Definitive, • Definitely useful exceptions) excellent evidence provides support. • Proven in both efficacy & effectiveness • Study results consistently positive and compelling • Must be used in the intended manner for proper clinical indications. Class II: • Safe, acceptable • Most evidence is positive Acceptable and useful • Clinically useful • Level 1 studies are absent, or inconsistent, or lack • Not yet confirmed definitively power • No evidence of harm • Class IIa : Acceptable and useful • Safe, acceptable • Generally higher levels of evidence Good evidence provides support • Clinically useful • Results are consistently positive • Considered treatments of choice • Class IIb: Acceptable and useful • Safe, acceptable • Generally lower or intermediate levels of evidence Fair evidence provides support • Clinically useful • Generally, but not consistently, positive results • Considered optional or alternative treatments Class III: • Unacceptable • No positive high level data Not acceptable, not useful, may be • Not useful clinically • Some studies suggest or confirm harm. harmful • May be harmful. • Research just getting started. • Minimal evidence is available Indeterminate • Continuing area of research • Higher studies in progress • No recommendations until • Results inconsistent, contradictory further research • Results not compelling 0666d73c299e1a1df1b16f7db322595f.doc Page 7 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
STEP 3: DETERMINE THE CLASS OF RECOMMENDATION. State a Class of Recommendation for the Guideline Proposal. State either a) the intervention, and then the conditions under which the intervention is either Class I, Class IIA, IIB, etc.; or b) the condition, and then whether the intervention is Class I, Class IIA, IIB, etc. Indicate if this is a __Condition or _x_Intervention The safety, efficacy and feasibility of low molecular weight heparin (LMWH) is the same as or better than unfractionated heparin (UFH), in prehospital and emergency department management of acute coronary syndromes (ACS) and acute myocardial infarction (AMI). Final Class of recommendation: __Class I-Definitely Recommended __Class IIa-Acceptable & Useful; good evidence __Class IIb-Acceptable & Useful; fair evidence __Class III – Not Useful; may be harmful __Indeterminate-minimal evidence or inconsistent
Treatment Recommendations DRAFT FOR DISCUSSION WITH THE TASK FORCE DALLAS 2005:
UFH versus LMWH in UA/NSTEMI Emergency department administration of LMWH compared to UFH for patients with UA/NSTEMI may be helpful in addition to antiplatelet therapy with aspirin, however it is unknown at what time period after the onset of symptoms it is optimal and if it should be standard practice for ED physicians to provide this medical intervention in the ED based on the current science. There is currently no evidence to suggest that treatment with LMWH in UA/NSTEMI is time critical so use in the prehospital setting is not recommended.
UFH versus LMWH in STEMI In the prehospital and early emergency department settings, administration of LMWH for patients with STEMI might be considered an acceptable alternative to UFH as ancillary therapy for patients aged less than 75 years who are receiving fibrinolytic therapy, provided that significant renal dysfunction (serum creatinine greater than 2.5 mg/dL in men or 2.0 mg/dL in women) is not present. UFH is recommended for patients aged 75 years or older as ancillary therapy to fibrinolysis in this setting. In patients with STEMI who are not receiving fibrinolysis, LMWH (specifically enoxaparin) might be considered an acceptable alternative to UFH in the emergency department setting.
REVIEWER’S PERSPECTIVE AND POTENTIAL CONFLICTS OF INTEREST: Briefly summarize your professional background, clinical specialty, research training, AHA experience, or other relevant personal background that define your perspective on the guideline proposal. List any potential conflicts of interest involving consulting, compensation, or equity positions related to drugs, devices, or entities impacted by the guideline proposal. Disclose any research funding from involved companies or interest groups. State any relevant philosophical, religious, or cultural beliefs or longstanding disagreements with an individual. Dr. Jane Lukins is credentialed in Emergency Medicine by the Australasian College of Emergency Medicine. She completed an Emergency Medical Services fellowship at University of Toronto, Canada. Dr. Lukins has no financial conflicts of interest involving consulting, compensation or equity positions related to drugs, devices, or entities impacted by the guideline process, or any research funding from involved companies or interest groups. She does not have any relevant intellectual biases. She does not have any relevant philosophical, religious, or cultural beliefs or longstanding disagreements with an individual.
REVIEWER’S FINAL COMMENTS AND ASSESSMENT OF BENEFIT / RISK: Summarize your final evidence integration and the rationale for the class of recommendation. Describe any mismatches between the evidence and your final Class of Recommendation. “Mismatches” refer to selection of a class of recommendation that is heavily influenced by other factors than just the evidence. For example, the evidence is strong, but implementation is difficult or expensive; evidence weak, but future definitive evidence is unlikely to be obtained. Comment on contribution of animal or mechanical model studies to your final recommendation. Are results within animal studies homogeneous? Are animal results consistent with results from human studies? What is the frequency of adverse events? What is the possibility of harm? Describe any value or utility judgments you may have made, separate from the evidence. For example, you believe evidence-supported interventions should be limited to in-hospital use because you think proper use is too difficult for pre-hospital providers. Please include relevant key figures or tables to support your assessment. 0666d73c299e1a1df1b16f7db322595f.doc Page 8 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
UFH versus LMWH in UA/NSTEMI Consensus on Science Extrapolation from 7 in-hospital RCTs (LOE 1 and 2) and additional studies (including 7 meta-analyses) which document similar or improved composite outcomes after administration of LMWH, compared with UFH, to patients with UA/NSTEMI within the first 48 hours after symptom onset suggests (LOE 7) that earlier administration of LMWH to patients in the ED may improve outcomes. Extrapolation to the prehospital setting is difficult as often the diagnosis of UA/NSTEMI is not yet clear.
Efficacy There are two excellent in-hospital LOE 1 trials that have shown superiority of the LMWH Enoxaparin, over UFH, in terms of efficacy, TIMI 11B and ESSENCE (Antman 1999; 1 and Cohen 1997), both show a reduction in the composite of death, MI and urgent revascularisation occurring in the acute phase (8 to 14 days) and continuing to the longer term (30 to 43 days). 1 year follow up shows this reduction is sustained. A meta-analysis of the results of these two trials (Antman 1999; 2) and another meta- analysis of the one-year follow up data from the 2 trials (Antman 2002) have also confirmed that enoxaparin significantly reduces the triple composite outcome of death, MI, and recurrent ischaemia needing urgent revascularisation to one year. However, in the largest trial, SYNERGY (Ferguson 2004), which included an early invasive strategy, there was no difference in efficacy between the LMWH Enoxaparin and UFH.
Large trials comparing other LMWHs to UFH have shown no difference in terms of efficacy, between the two anticoagulants, no trials have shown LMWH to be inferior to UFH in terms of efficacy. Three meta-analyses have been done comparing trials of different LMWHs and UFH (Eikelbloom 2000, Le Nguyen 2001 and Magee 2004). Eiklebloom and Le Nguyen found no statistically significant difference in efficacy between LMWH and UFH, although there was a 12% and 14% reduction respectively for the composite outcome of death and MI with LMWH. While Magee also found no difference in overall mortality between LMWH and UFH (OR = 1.0), there was a significant reduction in the occurrence of MI and need for revascularisation procedures (OR = 0.83 and 0.88 respectively).
Safety In the SYNERGY trial (Ferguson 2004) there was modest excess of major bleeding found in the LMWH Enoxaparin group compared to the UFH group. Other trials, however, have not found major bleeding events to be significantly different with LMWH compared to UFH,but have consistently shown an increase in minor bleeding, usually reported as ecchymoses at injection sites, with the use of LMWH.
A Mexican trial (Campos 2002) showed a superior safety profile using a lower dose of enoxaparin (0.8mg/kg/dose) when compared to UFH, while retaining the therapeutic effect and efficacy benefit of the LMWH.
With regard to safety of LMWH compared to UFH in the setting of angiography; Breiger (2002) concluded that omission of LMWH (enoxaparin) on the morning of angiography resulted in vascular complication rates comparable to that of UFH. One trial studying patients undergoing CABGs found a significant increase in post-operative bleeding complications in patients given LMWH (fragmin) within 12 hours of surgery, compared to those who received LMWH more than 12 hours prior to surgery or those being treated with UFH (Clark 2000), and another trial found there was an increased rate of re-exploration for post-op bleeding in patients who had received LMWH (Enoxaparin) within 48 hours of cardiac surgery (Jones 2002).
Feasibility It is well recognised that the twice daily subcutaneous dosing of LMWH is superior in terms of ease of administration in comparison to the intravenous infusion and APTT monitoring required with UFH. The authors of the SYNERGY trial (Ferguson 2004) concluded that “the advantages of convenience should be balanced with the modest excess of major bleeding”.
There have also been several cost analysis studies comparing the anticoagulants in different countries (done as subsets of the ESSENCE and TIMI 11B trials). All have shown an overall cost benefit to health systems in favour of LMWH, mainly due to a decrease in the need for revascularisation procedures. (O’Brien 2000, Brosa 2002, Detournay 2000, Mark 1998).
With regard to the timing of treatment with anticoagulation in patients with UA/NSTEMI there has been no time dependant caveat reported in the literature and although common sense would suggest treatment begin as soon as the condition is recognised, this requires ECG interpretation capability. For this reason it may not be feasible to use UFH or LMWH in the prehospital setting unless long out-of hospital times are expected and ECG capability is present. This could be an area that requires dedicated trials.
Crossover of anti-thrombin therapy Two recent trials comparing the LMWH, Enoxaparin, to UFH (Blazing 2004, Ferguson 2004) have included patients who received anti-thrombin therapy prior to randomization, meaning some patients had a crossover of anti-thrombin therapy. Both of these trials demonstrated neutral efficacy and one documented opposing safety for Enoxaparin compared to UFH. The meta-analysis by 0666d73c299e1a1df1b16f7db322595f.doc Page 9 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Petersen 2004 (LOE 1) documented an increased benefit for the combined efficacy outcome in those patients treated with Enoxaparin compared to UFH who did not receive pre-randomisation therapy (number needed to treat = 72). This was compared to the total study population, including patients receiving crossover therapy, where the number needed to treat was 107. The authors theorise that crossover of anti-thrombin therapy may attenuate a benefit of Enoxaparin if anti-thrombin effects fall during crossover, or may increase the risk of bleeding, if anti-thrombin effects rise. Therefore, crossover of antithrombin therapy is not recommended.
In combination with G2b3a Inhibitors Five trials have compared UFH and LMWH in patients with NSTEMI who were treated with a G2b3a inhibitor (Blazing 2004, Goodman 2003, Cohen 2002, Kovar 2002, Cohen 1999). In terms of efficacy, LMWHs compared favourably or were non inferior to UFH, and in terms of safety, there were similar or less frequent major bleeding events with LMWH, but again an increased frequency of minor bleeding complications defined as cutaneous (ecchymoses at injection or catheterization sites) or oropharyngeal (mostly epistaxis).
In the Emergency Department setting There are no trials specifically done in the prehospital or very early ED setting (first 4 hours from presentation in the ED). However, as many patients with UA/NSTEMI may call 911 or present to the Emergency Department up to 24 hours after the onset of symptoms, it is reasonable to draw efficacy conclusions from trials that have been conducted in other settings (eg inpatient/cardiology) if the time from qualifying symptoms to initiation of intervention is within 24 hours. The TIMI 11B trial (LOE 1, Antman 99; 1) reported a median time of 11 hours from qualifying symptom to first dose of study medication, which places it in a time frame relevant to ED. Unfortunately, this time interval is rarely reported in the literature and in its place, the time to randomisation from qualifying symptom is more commonly reported. This time interval can be used as a surrogate recognising that delays from randomisation to time of treatment can occur. Thus, this surrogate interval will underestimate the actual time to treatment. In the trial by Gurfinkel (1995) there was a mean time of 6 hours from qualifying symptoms to randomisation, FRAXIS (FRAIS investigators 1999) reported that 53% of patients were randomised within 6 hours of symptoms, SYNERGY (LOE 2, Ferguson 2004) had a median time of 14.7 hours from symptom onset to enrollment and the trial by Survana (1997) randomised patients within 24 hours of symptoms. Of these trials, TIMI 11B (LOE 1, Antman 1999; 1) and Gurfinkel 1995 (LOE 2) are supportive of LMWH compared to UFH in terms of efficacy, the others are neutral.
It should be noted that although the ESSENCE trial (LOE 1, Cohen 1997) randomised patients within 24 hours of the qualifying symptom, it was reported that 96% received the study medication within 12 hours of randomisation (which could mean up to 36 hours from symptom onset). There were four other trials that randomised patients within 48 to 72 hours of qualifying symptoms (Montalescot 2003, Mattoli 1999, Klein 1997 and Malhotra 2001; 1). These trials are therefore less relevant, and the evidence that they provide must be extrapolated to the ED setting.
Given this, it can be recommended that high risk patients with UA/NSTEMI (those with a clear history of unstable angina, a known significant past history of coronary artery disease or ischaemic ECG changes, or those with a cardiac enzyme rise) should be treated with LMWH (Enoxaparin) in preference to UFH as soon as the condition is realised, as long as CABG surgery is not planned within 24 hours. (Class 11b)
It is also recommended that future trials should attempt to define whether there is a time critical benefit to anticoagulation therapy in UA/NSTEMI and that it should be standard to measure and report the time interval from qualifying symptom to intervention.
In the Prehospital setting There are no trials comparing UFH and LMWH in the prehospital setting for UA/NSTEMI. There is also no evidence to suggest that treatment with an anticoagulant in UA/NSTEMI is time critical (such has been established with reperfusion in STEMI). Therefore, the use of an anticoagulant in most prehospital settings for UA/NSTEMI is not recommended. (Class Indeterminate)
UFH versus LMWH in STEMI Consensus on Science Evidence from 3 RCTs (LOE 1 and 2) and additional studies (LOE 1 to 7, including one meta-analysis) document improvement in overall TIMI flow and ischaemic outcomes when LMWH (specifically enoxaparin), compared to UFH, is administered to patients with STEMI in the early hospital setting (within 6 hours of symptom onset).
In the prehospital setting, 2 RCTs (LOE 1 and 2) document improvement in composite outcomes when LMWH (specifically enoxaparin), compared to UFH, is administered as to patients with STEMI as adjunctive therapy to fibrinolysis.
In the Emergency Department setting 0666d73c299e1a1df1b16f7db322595f.doc Page 10 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
STEMI is a time critical medical condition and trials that have been conducted in the hospital setting have randomised patients within the first 6 hours of symptom onset, this makes them relevant to the ED setting. In-hospital trials in patients with STEMI have compared UFH and LMWH as ancillary treatment with fibrinolysis, during PCI and also in the case where revascularisation is not an option. In combination with Fibrinolytic agents, in terms of efficacy the LMWHs, have been found to be superior to, or as good as UFH in terms of overall TIMI flow (Wallentin 2003; 1, Ross 2001) and also in reducing the frequency of ischaemic complications (Van de Werf 2001), with a trend to a 14% reduction in mortality in a meta-analysis (Theroux 2003). In terms of safety, trials have conflicting results. Some trials have shown no difference (Wallentin 2003; 1 and Ross 2001), ASSENT-3 found the combined efficacy and safety outcome to be in favour of enoxaparin (Van de Werf 2001), but the meta-analysis showed significantly more bleeding complications (major and minor) with Enoxaparin compared to UFH (Theroux 2003). When revascularization is not an option (eg: late presentation, contraindication) one LOE 1 trial showed a similar safety and efficacy profile of LMWH (enoxaparin) to UFH (Cohen 2003).
Therefore, in the early ED setting it is recommended that LMWH (specifically enoxaparin) might be considered an acceptable alternative to UFH as ancillary therapy for patients aged less than 75 years who are receiving fibrinolytic therapy, provided that significant renal dysfunction (serum creatinine greater than 2.5 mg/dL in men or 2.0 mg/dL in women) is not present. (Class IIb) In patients with STEMI who are not receiving fibrinolysis, LMWH (specifically enoxaparin) might be considered an acceptable alternative to UFH. (Class Indeterminate)
In the Prehospital setting Two trials comparing UFH to LMWH as ancillary treatment with fibrinolysis have been conducted in the prehospital setting (Baird 2002 and Wallentin 2003; 2). In the trial by Baird 43% of patients were treated in the prehospital setting by physicians, in ASSENT-3 Plus (Wallentin 2003; 2) all patients were treated in the prehospital setting by physicians, or by nurses or paramedics with on-line medical control.
Both trials used Enoxaparin as the LMWH and showed superiority in terms of efficacy compared to UFH.
In terms of safety, the Baird trial showed no difference in major bleeding complications, however there was a concerning increase in intracranial hemorrhage in patients > 75 years receiving Enoxaparin in ASSENT–3 Plus. This serious adverse event led to the conclusion in the ASSENT-3 Plus trial that (at least with tenecteplase) UFH is recommended for the prehospital setting. The results of trials investigating a decreased dose of enoxaparin in those older than 75 years are needed to help define the safety profile of Enoxaparin before it can be recommended in this age group.
In terms of feasibility, a cost analysis showed treatment with LMWH to be cheaper in the acute phase (Baird 2002) and in ASSENT-3 Plus patients received reperfusion therapy 47 minutes faster than compared with the in-hospital parallel trial (Van Der Werf 2002) and more patients had received the full dose of enoxaparin compared to UFH by the time they reached the hospital.
Therefore, in the Prehospital environment LMWH (specifically enoxaparin) might be considered an acceptable alternative to UFH as ancillary therapy for patients aged less than 75 years who are receiving fibrinolytic therapy, provided that significant renal dysfunction (serum creatinine greater than 2.5 mg/dL in men or 2.0 mg/dL in women) is not present. (Class Indeterminate) UFH is recommended for patients aged 75 years or older as ancillary therapy to fibrinolysis in this setting. (Class I)
Preliminary draft/outline/bullet points of Guidelines revision: Include points you think are important for inclusion by the person assigned to write this section. Use extra pages if necessary. UFH versus LMWH in UA/NSTEMI Previous Recommendations From the previous ACC/AHA Guidelines 2000 for the management of UA/NSTEMI it was recommended that “anticoagulation with subcutaneous low-molecular-weight heparin or intravenous unfractionated heparin should be added to antiplatelet therapy with aspirin, clopidogrel, or both.” (Class 1, Level B) This recommendation was upgraded in 2002 to Class 1, Level A, and was reiterated for management of these patients in the emergency department (Pollack, 2003 Ann Emerg Med). Also in these guidelines was the recommendation that “Enoxaparin is preferable to unfractionated heparin as an anticoagulant in patients with unstable angina/NSTEMI, unless coronary artery bypass grafting is planned within 24 hours” (Class IIa, Level A).
CoSTR Statement DRAFT FOR DISCUSSION WITH THE TASK FORCE DALLAS 2005: Consensus on Science Extrapolation from 7 in-hospital RCTs (LOE 1 and 2) and additional studies (including 7 meta-analyses) which document similar or improved composite outcomes after administration of LMWH, compared with UFH, to patients with UA/NSTEMI within the 0666d73c299e1a1df1b16f7db322595f.doc Page 11 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
first 48 hours after symptom onset suggests (LOE 7) that earlier administration of LMWH to patients in the ED may improve outcomes. Extrapolation to the prehospital setting is difficult as often the diagnosis of UA/NSTEMI is not yet clear.
Treatment Recommendation Therefore, emergency department administration of LMWH compared to UFH for patients with UA/NSTEMI may be helpful in addition to antiplatelet therapy with aspirin, however it is unknown at what time period after the onset of symptoms it is optimal and if it should be standard practice for ED physicians to provide this medical intervention in the ED based on the current science. There is currently no evidence to suggest that treatment with LMWH in UA/NSTEMI is time critical so use in the prehospital setting is not recommended.
UFH versus LMWH in STEMI Recent Guidelines The 2004 ACC/AHA Guidelines for management of patients with STEMI include the following recommendations regarding adjunctive therapy with anticoagulants: Class IIb “Low-molecular-weight heparin might be considered an acceptable alternative to UFH as ancillary therapy for patients aged less than 75 years who are receiving fibrinolytic therapy, provided that significant renal dysfunction (serum creatinine greater than 2.5 mg/dL in men or 2.0 mg/dL in women) is not present.” “Enoxaparin (30-mg IV bolus followed by 1.0 mg/kg SC every 12 hours until hospital discharge) used in combination with full- dose tenecteplase is the most comprehensively studied regimen in patients aged less than 75 years of age. (Level of Evidence: B) Class III Low-molecular-weight heparin should not be used as an alternative to UFH as ancillary therapy in patients aged more than 75 years who are receiving fibrinolytic therapy. (Level of Evidence: B) Low-molecular-weight heparin should not be used as an alternative to UFH as ancillary therapy in patients less than 75 years who are receiving fibrinolytic therapy but have significant renal dysfunction (serum creatinine greater than 2.5 mg/dL in men or 2.0 mg/dL in women). (Level of Evidence: B)
CoSTR Statement DRAFT FOR DISCUSSION WITH THE TASK FORCE DALLAS 2005: Consensus on Science Evidence from 3 RCTs (LOE 1 and 2) and additional studies (LOE 1 to 7, including one meta-analysis) document improvement in overall TIMI flow and ischaemic outcomes when LMWH (specifically enoxaparin), compared to UFH, is administered to patients with STEMI in the early hospital setting (within 6 hours of symptom onset).
In the prehospital setting, 2 RCTs (LOE 1 and 2) document improvement in composite outcomes when LMWH (specifically enoxaparin), compared to UFH, is administered to patients with STEMI as adjunctive therapy to fibrinolysis. This however, must be balanced against the risk of serious adverse events, specifically of an increase in intracranial hemorrhage in patients > 75 years receiving LMWH (Enoxaparin) documented in one of these RCTs (LOE 2).
Treatment Recommendation Therefore, in the prehospital and early emergency department settings, administration of LMWH for patients with STEMI might be considered an acceptable alternative to UFH as ancillary therapy for patients aged less than 75 years who are receiving fibrinolytic therapy, provided that significant renal dysfunction (serum creatinine greater than 2.5 mg/dL in men or 2.0 mg/dL in women) is not present. UFH is recommended for patients aged 75 years or older as ancillary therapy to fibrinolysis in this setting. In patients with STEMI who are not receiving fibrinolysis, LMWH (specifically enoxaparin) might be considered an acceptable alternative to UFH in the emergency department setting.
Publication: Chapter: Pages:
Topic and subheadings:
UFH versus LMWH in UA/NSTEMI Safety 0666d73c299e1a1df1b16f7db322595f.doc Page 12 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Efficacy Feasibility Crossover of antithrombin therapy In combination with G2b3a Inhibitors In the Emergency Department setting In the Prehospital setting
UFH versus LMWH in STEMI In the Prehospital setting: Safety, efficacy, and feasibility In the Emergency Department setting In combination with Fibrinolytic agents In combination with diagnostic angiography and PCI When revascularization is not an option (eg: late presentation, contraindication)
Attachments: . Bibliography in electronic form using the Endnote Master Library. It is recommended that the bibliography be provided in annotated format. This will include the article abstract (if available) and any notes you would like to make providing specific comments on the quality, methodology and/or conclusions of the study. 0666d73c299e1a1df1b16f7db322595f.doc Page 13 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT Citation List
Citation Marker Full Citation* Antman 1999; 1 Antman, E. M., C. H. McCabe, et al. (1999). "Enoxaparin prevents death and cardiac ischemic events in unstable angina/non-Q-wave myocardial infarction. Results of the thrombolysis in myocardial infarction (TIMI) 11B trial." Circulation 100(15): 1593-1601. BACKGROUND: Low-molecular-weight heparins are attractive alternatives to unfractionated heparin (UFH) for management of unstable angina/non-Q-wave myocardial infarction (UA/NQMI). METHODS AND RESULTS: Patients (n=3910) with UA/NQMI were randomized to intravenous UFH for >/=3 days followed by subcutaneous placebo injections or uninterrupted antithrombin therapy with enoxaparin during both the acute phase (initial 30 mg intravenous bolus followed by injections of 1.0 mg/kg every 12 hours) and outpatient phase (injections every 12 hours of 40 mg for patients weighing <65 kg and 60 mg for those weighing >/=65 kg). The primary end point (death, myocardial infarction, or urgent revascularization) occurred by 8 days in 14.5% of patients in the UFH group and 12.4% of patients in the enoxaparin group (OR 0.83; 95% CI 0.69 to 1.00; P=0. 048) and by 43 days in 19.7% of the UFH group and 17.3% of the enoxaparin group (OR 0.85; 95% CI 0.72 to 1.00; P=0.048). During the first 72 hours and also throughout the entire initial hospitalization, there was no difference in the rate of major hemorrhage in the treatment groups. During the outpatient phase, major hemorrhage occurred in 1.5% of the group treated with placebo and 2.9% of the group treated with enoxaparin (P=0.021). CONCLUSIONS: Enoxaparin is superior to UFH for reducing a composite of death and serious cardiac ischemic events during the acute management of UA/NQMI patients without causing a significant increase in the rate of major hemorrhage. No further relative decrease in events occurred with outpatient enoxaparin treatment, but there was an increase in the rate of major hemorrhage.
TIMI 11B Trial. Multicentre, double blind, randomised controlled trial Hypothesis: to test if LMWH (Enoxaparin) was superior to UFH in patients with unstable angina/Non-STEMI. Enoxaparin given as initial 30mg IV bolus, them 1mg/kg subcutaneously) in the acute phase (first 8 days) and if an extended outpatient course (to 43 days) provided benefit. Primary end points: For efficacy were a composite of all cause mortality, recurrent MI, or urgent revascularisation. For safety, major hemorrhage. Secondary end points: Looked at subgroup outcomes and minor hemorrhage. Outcomes at 48hrs and 14 days also looked at. N=3910 pts, groups were similar. Time from qualifying symptom (>5 mins ischaemic discomfort at rest) to first dose of study medication: median 11 hours (5.8, 18.9). Enoxaparin found to be superior in acute phase, max benefit at 48 hrs, with no increase in major hemorrhage, but an increase in incidence of minor hemorrhage (injection site or sheath site hematoma). No continued benefit in outpatient phase but an increased incidence of major hemorrhage. Drug company sponsored the trial (declared).
Level of Evidence: 1 Quality of Evidence: Excellent in design and methodology, Excellent in terms of appropriateness to ED setting. Direction of Evidence: Supportive of LMWH (enoxaparin) over UFH in terms of efficacy and neutral for safety in the acute phase. (Commencing treatment within 24 hours symptom onset)
Antman 1999; 2 Antman, E. M., M. Cohen, et al. (1602). "Assessment of the treatment effect of enoxaparin for unstable angina/non-Q-wave myocardial infarction: TIMI 11B-essence meta-analysis." Circulation 100(15): 1602-1608. Background - Two phase III trials of enoxaparin for unstable angina/non- Q-wave myocardial infarction have shown it to be superior to unfractionated heparin for preventing a composite of death and cardiac ischemic events. A prospectively planned meta-analysis was performed to provide a more precise estimate of the effects of enoxaparin on multiple end points. Methods and Results - Event rates for death, the composite end points of death/nonfatal myocardial infarction and death/nonfatal myocardial infarction/urgent revascularization, and major hemorrhage were extracted from the TIMI 11B and ESSENCE databases. Treatment effects at days 2, 8, 14, and 43 were expressed as the OR (and 95% CI) for enoxaparin versus unfractionated heparin. All heterogeneity tests for 0666d73c299e1a1df1b16f7db322595f.doc Page 14 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
efficacy end points were negative, which suggests comparability of the findings in TIMI 11B and ESSENCE. Enoxaparin was associated with a 20% reduction in death and serious cardiac ischemic events that appeared within the first few days of treatment, and this benefit was sustained through 43 days. Enoxaparin's treatment benefit was not associated with an increase in major hemorrhage during the acute phase of therapy, but there was an increase in the rate of minor hemorrhage (OR 2.38; 95% CI 1.98 to 2.85; p<0.0001). Conclusions - The accumulated evidence, coupled with the simplicity of subcutaneous administration and elimination of the need for anticoagulation monitoring, indicates that enoxaparin should be considered as a replacement for unfractionated heparin as the antithrombin for the acute phase of management of patients with high-risk unstable angina/non-Q-wave myocardial infarction.
Meta-analysis of ESSENCE and TIMI 11B trials. Trials selected for intervention with enoxaparin as the LMWH intervention group. Minor hemorrhage was not defined in this trial. Level of Evidence: 1 Quality of Evidence: Excellent Direction of Evidence: Supportive for efficacy of LMWH (Enoxaparin) v UFH, with treatment effect occurring within 48 hours and persisting out to day 43. Opposing for safety with minor hemorrhage only increased significantly with LMWH. Antman 2002 Antman, E. M., M. Cohen, et al. (2002). "Enoxaparin is superior to unfractionated heparin for preventing clinical events at 1-year follow-up of TIMI 11B and ESSENCE." European Heart Journal 23(4): 308-314. Background: Enoxaparin treatment is associated with a 20% reduction in clinical events during the acute phase of management of patients with unstable angina/non ST elevation myocardial infarction. Interest in the use of enoxaparin would be enhanced further if evidence of a durable treatment benefit over the long term could be provided. Methods: Event rates at 1 year for the composite end-point of death/non-fatal myocardial infarction/urgent revascularization and its individual components were ascertained from the TIMI 11B and ESSENCE databases. Results: There was no evidence of heterogeneity between TIMI 11B and ESSENCE in tests for interactions between treatment and trial. A significant treatment benefit of enoxaparin on the rate of death/non-fatal myocardial infarction/urgent revascularization was observed at 1 year (hazard ratio 0.88, P=0.008). The event rate was 25.8% in the unfractionated heparin group and 23.3% in the enoxaparin group, an absolute difference of 2.5%. A progressively greater treatment benefit of enoxaparin was observed as the level of patient risk at baseline increased. Treatment effects for the individual end-point elements ranged from 9-14%, favouring enoxaparin. Conclusions: The stable absolute difference in event rates of 2.5% seen at 8 days and again at 1 year favouring enoxaparin may be due to more effective control of the thrombotic process surrounding the index event. Once the pharmacological effect of enoxaparin had dissipated there was no rebound increase in events. Thus, those patients who had received enoxaparin acutely were protected from experiencing a deterioration of the original therapeutic benefit. These findings regarding enoxaparin add to the data to be considered by clinicians when selecting an antithrombin for the acute phase of management of unstable angina/non-ST elevation myocardial infarction. (C) 2001 The European Society of Cardiology.
Prospective meta-analysis of 1 year follow up data of TIMI 11B and ESSENCE trials. Hypothesis: Treatment effect of enoxaparin given in the acute phase for unstable angina/Non- STEMI would be sustained at 1 year. N=6646 available for follow up of 7081 originally enrolled in the 2 trials (94%). Outcomes: Individual events of death, MI, urgent revascularisation, and composite of death and MI, and triple composite. Patients with 0–2 risk factors were combined into a low risk stratum (32%), those with 3–4 risk factors into an intermediate risk stratum (56%), and 5–7 risk factors into a high risk stratum (12%), based on the following TIMI Risk Factors • Age >65 y • Documented prior coronary artery stenosis >50% • Three or more conventional cardiac risk factors (eg, age, sex, family history, hyperlipidemia, diabetes, smoking, hypertension, obesity) • Use of aspirin in the preceding 7 d • Two or more anginal events in the preceding 24 h • ST-segment deviation (transient elevation or persistent depression) 0666d73c299e1a1df1b16f7db322595f.doc Page 15 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
• Increased cardiac biomarkers The 8 day benefit of enoxaparin was sustained at 1 year for the triple composite outcome and increased as the baseline risk for heart disease increased. A statistically significant treatment benefit of enoxaparin was observed in the intermediate (hazard ratio 0·87; 95% CI 0·77, 0·99; P=0·04) and high risk (hazard ratio 0·80; 95% CI 0·65, 0·98; P=0·03) groups.
Level of Evidence: 1 Quality of Evidence: Excellent design and methodology, appropriateness to ED setting is Good. Direction of Evidence: Supportive of LMWH over UFH in terms of efficacy for intermediate and high risk UA/NSTEMI.
Baird 2002 Baird Sh, M. I. B. M. S. J. T. T. G. W. C. (2002). "Randomized comparison of enoxaparin with unfractionated heparin following fibrinolytic therapy for acute myocardial infarction. [comment]." European Heart Journal 23(8): 627-32. AIMS: To compare the efficacy and safety of low molecular weight heparin with unfractionated heparin following fibrinolytic therapy for acute myocardial infarction. METHODS AND RESULTS: Three-hundred patients receiving fibrinolytic therapy following acute myocardial infarction were randomly assigned to low molecular weight heparin as enoxaparin (40 mg intravenous bolus, then 40 mg subcutaneously every 8 h, n=149) or unfractionated heparin (5000 U intravenous bolus, then 30 000 U. 24 h(-1), adjusted to an activated partial thromboplastin time 2-2.5x normal, n=151) for 4 days in conjunction with routine therapy. Clinical and therapeutic variables were analysed, in addition to use of enoxaparin or unfractionated heparin, to determine independent predictors of the 90-day composite triple end-point (death, non-fatal reinfarction, or readmission with unstable angina). The triple end-point occurred more frequently in patients receiving unfractionated heparin rather than enoxaparin (36% vs. 26%; P=0.04). Logistic regression modeling of baseline and clinical variables identified the only independent risk factors for recurrent events as left ventricular failure, hypertension, and use of unfractionated heparin rather than enoxaparin. There was no difference in major haemorrhage between those receiving enoxaparin (3%) and unfractionated heparin (4%). CONCLUSION: Use of enoxaparin compared with unfractionated heparin in patients receiving fibrinolytic therapy for acute myocardial infarction was associated with fewer recurrent cardiac events at 90 days. This benefit was independent of other important clinical and therapeutic factors. Copyright 2002 The European Society of Cardiology.
Prospective, randomised controlled trial. Hypothesis: To determine if there is a benefit of LMWH (enoxaparin) over UFH following fibrinolytic therapy in patients with AMI for reduction of adverse events at 90 days. Primary end point: composite of death, reinfarction, or readmission with unstable angina. N=300, equal groups. Treatment given in prehospital (MD staffed) in 43% of cases or ED setting. There was a 30% relative risk reduction of composite endpoints with LMWH. No increased incidence of clinically significant hemorrhage. Cost comparison also done. LMWH cheaper over 4 day trial.
Level of Evidence: 1 Quality of Evidence: Good design and methodology, moderate sample size and non-blinded. Relevant to prehospital and ED setting. Direction of Evidence: Supportive of LMWH (enoxaparin) over UFH for STEMI post lytics.
Berkowitz 2001 Berkowitz, S. D., S. Stinnett, et al. (2001). "Prospective comparison of hemorrhagic complications after treatment with enoxaparin versus unfractionated heparin for unstable angina pectoris or non-ST-segment elevation acute myocardial infarction." American Journal of Cardiology 88(11): 1230-4. Patients with unstable angina pectoris (UAP) or non-ST-segment elevation acute myocardial infarction (AMI) are at risk of death or recurrent ischemic events, despite receiving aspirin and unfractionated heparin (UFH). This study investigates the effect of the low molecular weight heparin, enoxaparin, on the incidence of hemorrhage and thrombocytopenia in relation to baseline characteristics and subsequent invasive procedures. Rates of hemorrhage and thrombocytopenia were analyzed for UAP or non- ST-segment elevation AMI in patients included in the prospective, randomized, double- blind Efficacy and Safety of Subcutaneous Enoxaparin in Non-Q-wave Coronary Events 0666d73c299e1a1df1b16f7db322595f.doc Page 16 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
(ESSENCE) study. Patients received either enoxaparin or UFH, plus aspirin, for 2 to 8 days. The overall rate of major hemorrhage (at 30 days) was comparable between the 2 groups (6.5% for enoxaparin vs. 7.0% for UFH, p = 0.6). The rate of major hemorrhage while on treatment was slightly higher in the enoxaparin group, but this was not significant (1.1% vs 0.7% for UFH, p = 0.204), as was the rate of major hemorrhage within 48 hours of coronary artery bypass grafting performed within 12 hours of treatment. However, the rate of minor hemorrhage was significantly higher in the enoxaparin group, with the majority being injection-site ecchymoses or hematomas (11.9% vs. 7.2% with UFH, p <0.001). Thrombocytopenia (platelet count <100,000 per mm(3)) occurred mainly in association with coronary bypass surgery, with a similar rate in both groups. Thus, enoxaparin is a well-tolerated alternative to UFH in the management of UAP or non-ST- segment elevation AMI. Despite the more effective antithrombotic effect, which results in fewer ischemic events, enoxaparin is not associated with an increase in the rate of major hemorrhagic complications, and is not significantly associated with thrombocytopenia, but is associated with an increase in minor injection site ecchymosis.
Subset of ESSENCE study, looking at hemorrhagic complications after treatment with LMWH (Enoxaparin) or UFH for unstable angina/NonSTEMI. Prospective, randomised, double-blinded controlled study. Concludes that enoxaparin is at least as safe as UFH with regard to major hemorrhage in this setting with no statistical difference between the two groups (although there was a non-statistical trend to increased rate of major hemorrhage while on treatment) With regard to minor hemorrhage there was an increased incidence injection site hematoma associated with LMWH).
Level of Evidence: 2 Quality of Evidence: Excellent design and methods, appropriate to ED/Prehospital setting as addresses safety concerns. Direction of Evidence: Neutral for major hemorrhagic complications, opposing for minor hemorrhagic complications defined as increased rates of injection site hematoma.
Blazing 2004 Blazing, M. A., J. A. de Lemos, et al. (2004). "Safety and efficacy of enoxaparin vs unfractionated heparin in patients with non-ST-segment elevation acute coronary syndromes who receive tirofiban and aspirin: a randomized controlled trial.[see comment] [erratum appears in JAMA. 2004 Sep 8;292(10):1178 Note: Correction of dosage error in text]." 55-64, 2004 Jul 7. CONTEXT: Enoxaparin or the combination of glycoprotein IIb/IIIa inhibitor tirofiban with unfractionated heparin independently have shown superior efficacy over unfractionated heparin alone in patients with non-ST-elevation acute coronary syndromes (ACS). It is not clear if combining enoxaparin with glycoprotein IIb/IIIa inhibitors is as safe or as effective as the current standard combination of unfractionated heparin with glycoprotein IIb/IIIa inhibitors. OBJECTIVE: To assess efficacy and safety of the combination of enoxaparin and tirofiban compared with unfractionated heparin and tirofiban in patients with non-ST-elevation ACS. DESIGN, SETTING, AND PARTICIPANTS: A prospective, international, open-label, randomized, noninferiority trial of 1 mg/kg of enoxaparin every 12 hours (n = 2026) compared with weight-adjusted intravenous unfractionated heparin (n = 1961) in patients with non-ST-elevation ACS receiving tirofiban and aspirin. Phase A of the A to Z trial was conducted between December 1999 and May 2002. MAIN OUTCOME MEASURES: Death, recurrent myocardial infarction, or refractory ischemia at 7 days in the intent-to-treat population with boundaries set for superiority and noninferiority. Safety based on measures of bleeding using the Thrombolysis in Myocardial Infarction (TIMI) classification system. RESULTS: A total of 169 (8.4%) of 2018 patients randomized to enoxaparin experienced death, myocardial infarction, or refractory ischemia at 7 days compared with 184 (9.4%) of 1952 patients randomized to unfractionated heparin (hazard ratio [HR], 0.88; 95% confidence interval [CI], 0.71-1.08). This met the prespecified criterion for noninferiority. All components of the composite primary and secondary end points favored enoxaparin except death, which occurred in only 1% of patients (23 for enoxaparin and 17 for unfractionated heparin). Rates for any TIMI grade bleeding were low (3.0% for enoxaparin and 2.2% for unfractionated heparin; P =.13). Using a worst-case approach that combined 2 independent bleeding evaluations, use of enoxaparin was associated with 1 additional 0666d73c299e1a1df1b16f7db322595f.doc Page 17 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
TIMI major bleeding episode for each 200 patients treated. CONCLUSIONS: In patients receiving tirofiban and aspirin, enoxaparin is a suitable alternative to unfractionated heparin for treatment of non-ST-elevation ACS. The 12% relative and 1% absolute reductions in the primary end point in favor of enoxaparin met criterion for noninferiority and are consistent with prior trials performed without the use of glycoprotein IIb/IIIa inhibitors.
A to Z Trial (A phase). Prospective, randomized trial of patients with NSTEMI receiving aspirin and G2b/3a inhibitor (tirofiban) comparing treatment with LMWH (enoxaparin) or UFH. Patients were randomized within 24 hours of symptom onset. Primary end points: combined outcome of death, recurrent myocardial infarction, or refractory ischemia at 7 days (efficacy) and major bleeding (safety).
Level of Evidence: 1 Quality of Evidence: Good design and methods, moderate sample size, non-blinded. Direction of Evidence: Neutral for efficacy and safety of LMWH (enoxaparin) compared to UFH in the setting of GIIb/IIIa inhibitor (tirofiban) use.
Bozovich 2000 Bozovich, G. E., E. P. Gurfinkel, et al. (2000). "Superiority of enoxaparin versus unfractionated heparin for unstable angina/non-Q-wave myocardial infarction regardless of activated partial thromboplastin time." American Heart Journal 140(4): 637-642. Background: Whether the clinical superiority of enoxaparin versus unfractionated heparin (UFH) depends on a more stable antithrombotic effect or the proportion of patients not reaching the therapeutic level with UFH has not been addressed. Methods: All patients participating in the Thrombolysis In Myocardial Infarction 11B trial who received UFH and had sufficient activated partial thromboplastin time (aPTT) data (n = 1893) were compared with patients who received enoxaparin (n = 1938). Patients receiving UFH were divided into 3 categories depending on mean aPTT values throughout 48 hours: subtherapeutic, for those in whom the average aPTT fell below 55 seconds; therapeutic, between 55 and 85 seconds; and supratherapeutic, longer than 85 seconds. Events and bleeding rates were determined at 48 hours. Results: A small portion of patients (6.7%) had a subtherapeutic average aPTT value (n = 127). Forty-seven percent of patients (n = 891) fell within the therapeutic range, and 46% were in the supratherapeutic level (n = 875). Event rates were 7.0% in the UFH group versus 5.4% with enoxaparin (P = .039). Events rates were higher in every aPTT strata compared with enoxaparin and statistically significant in the supratherapeutic group (odds ratio 0.65; 95% confidence interval, 0.47- 0.89). Major bleeding rates were 0%, 0.6%, and 0.9% for the subtherapeutic, target, and supratherapeutic strata, respectively, and 0.8% with enoxaparin. Minor hemorrhages occurred in 5.1% of patients receiving enoxaparin versus 3.9%, 2%, and 2.3%, respectively, for the UFH subgroups (P < .001 for all UFH groups vs enoxaparin). Conclusions: Enoxaparin showed a better clinical profile compared with every level of anticoagulation with UFH. Potential mechanisms for enoxaparin superiority are stable antithrombotic activity, lack of rebound thrombosis, and intrinsic superiority.
Post hoc analysis from TIMI 11B. Hypothesis: Enoxaparin superiority is due to a more stable antithrombotic effect rather than the proportion of patients not reaching the therapeutic level with UFH. Problems: Original study not powered to look at UFH subgroups, and only a small proportion of patients were in the subtherapeutic aPTT group. Level of Evidence: 7 Quality of Evidence: Fair design and methods Direction of Evidence: Supportive of LMWH in terms of efficacy, Neutral for safety (major hemorrhage) and opposing for minor hemorrhage (the majority were related to instrumentation or surgery.) Brieger 2002 Brieger, D., V. Solanki, et al. (2002). "Optimal strategy for administering enoxaparin to patients undergoing coronary angiography without angioplasty for acute coronary syndromes." American Journal of Cardiology 89(10): 1167-1170. The optimal strategy for administration of low molecular weight heparin in patients with acute coronary syndrome (ACS) undergoing coronary angiography without percutaneous coronary intervention remains unclear. We studied postangiographic vascular complications in 325 consecutive patients (210 men and 115 women, mean age 0666d73c299e1a1df1b16f7db322595f.doc Page 18 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
63 years) with ACS undergoing diagnostic coronary angiography via a femoral approach followed by immediate sheath removal. At the time of angiography, 44 patients were on intravenous unfractionated heparin (UFH), 229 on subcutaneous enoxaparin, and 52 on no heparin. Enoxaparin was withheld on the morning of angiography in 181 of 229 patients: the no A.M. dose group. Vascular complications were audited, including hematoma development at angiographic puncture sites; these complications were considered significant if >25 cm2. Major vascular complications requiring transfusion or surgical interventions were infrequent in all groups. Patients receiving enoxaparin on the morning of angiography had a twofold increase in significant hematoma rate compared with the no A.M. dose group (31% vs 16%; p = 0.015). The no A.M. dose group had hematoma rates similar to UFH (20%; p = NS) and no anticoagulation (13.5%; p = NS). No significant increase in ischemic episodes occurred as a result of withholding enoxaparin in the no A.M. dose group. We conclude that omission of enoxaparin on the morning of cardiac catheterization results in vascular complications rates comparable to that of UFH without precipitating rebound ischemia. This is a practical, safe strategy for patients with ACS undergoing coronary angiography, allowing early mobilization for most patients who do not proceed to immediate percutaneous coronary intervention. (C) 2002 by Excerpta Medica, Inc.
Prospective, non-randomised cohort study of patients with ACS undergoing coronary angiography. N=325. No randomisation, no blinding. Hypothesis: Patients treated with LMWH (Enoxaparin) before diagnostic angiography may have increased risk of vascular complications with post- procedure sheath removal compared to those treated with UFH. Outcome measures: Major vascular complications (Ultrasound documented femoral pseudoaneurysm, retroperitoneal hematoma or requirement for surgical intervention or blood transfusion). Secondary measures: Significant wound hematomas. Attempts to address safety concerns post angiography with sheath removal, but does not define an optimal time post LMWH dose at which angiography with sheath removal is safe. Study recommends either withholding am dose of LMWH, or delaying sheath removal. Level of Evidence: 3 Quality of Evidence: Fair Direction of Evidence: Opposing for safety of LMWH given on the morning of angiography when there is immediate sheath removal. Neutral for safety of LMWH compared to UFH when am dose is omitted prior to angiography with immediate sheath removal. Brosa 2002 Brosa, M., C. Rubio-Terres, et al. (2002). "Cost-effectiveness analysis of enoxaparin versus unfractionated heparin in the secondary prevention of acute coronary syndrome." Pharmacoeconomics 20(14): 979-987. Background: The Efficacy and Safety of Subcutaneous Enoxaparin in Non-Q- Wave Coronary Events (ESSENCE) and Thrombolysis in Myocardial Infarction (TIMI) 11B studies revealed that enoxaparin reduced the incidence of death, myocardial reinfarction and recurrent angina in patients with acute coronary syndrome (ACS) compared with unfractionated heparin (UFH). Objective: To perform a pharmacoeconomic analysis to evaluate the cost effectiveness of treatment with enoxaparin compared with UFH in Spanish patients with ACS. Design and setting: Retrospective cost-effectiveness analysis using data and costs from Spanish sources, conducted from the perspective of the National Health System. Patients, interventions and outcomes measures: The study was based on the results of the ESSENCE and TIMI 11B clinical trials, which included more than 7000 patients with ACS treated with enoxaparin or UFH. The main variables studied were the success rate, expressed as patients with no complications (reinfarction, unstable angina or death), and the decrease in the utilisation of healthcare resources (revascularisation procedures and hospitalisation). Results: The base-case results of the analysis showed superior efficacy and lower total treatment and follow-up costs with enoxaparin compared with UFH. The total savings in direct health costs per patient with enoxaparin ranged between 448 and 659 euros (time horizons of 1 month and 1 year, respectively) [2001 values]. The sensitivity analysis results confirmed the advantage of enoxaparin in all cases, except in one scenario: when simultaneously using all the minimum values of the confidence interval for absolute risk reduction (ARR) in the utilisation of health resources. Conclusions: This study suggests that enoxaparin is a more effective and less expensive treatment option than UFH in secondary prevention of patients with ACS in Spain, confirming the results obtained in other pharmacoeconomic 0666d73c299e1a1df1b16f7db322595f.doc Page 19 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
analyses performed in the UK, USA, France and Canada.
Retrospective extrapolation using the ESSENCE and TIMI 11B studies to conduct a pharmacoeconomic analysis. Possibly biased by fact that population of study was not same population of economic analysis. Level of Evidence: 7. Quality of Evidence: Fair design and methods. Direction of Evidence: Supportive of cost efficiency of LMWH (enoxaparin) being superior (cheaper) in comparison to UFH in Spain. Campos 2002 Victoria Campos, J., U. Juarez Herrera, et al. (2002). "Decreased total bleeding events with reduced doses of Enoxaparin versus unfractionated heparin in high risk unstable angina. [Spanish]." Archivos de Cardiologia de Mexico 72(3): 209-219. In this prospective, randomized and controlled study, we compare complications in 2 groups of patients: group 1, enoxaparin 0.8 mg/kg, subcutaneous every 12 hours during 5 days, and group 2, intravenous unfractionated heparin during 5 days, by infusion treated to activate partial tromboplastin time 1.5-2 the upper limit of normal. Blood samples were obtained at 4, 12, 24 hours and at day 5 of treatment, to measure anti-Xa levels, and also, evaluated end points at 30 days, between groups. Univariate and multivariate logistic regression analyses were performed with clinical and angiographic variables between groups, with p < 0.05. Results: 203 consecutive patients, average age of 60.5 +/- 11.2 years, and 80% men, were included. There were no differences in clinical and angiographic characteristics. All patients with enoxaparin had therapeutic levels of anti-Xa, of 0.5 to 0.67 U/mL. There was increasing risk of total bleeding in group 2 (18.7%) than in group 1 (5.6%), with RR = 1.72 (95% CI 1.29,2.29), p = .003. Also, there was 33.3% of MACE in group 2, and only 17.8% in group 1, with RR = 1.88 (CI 95% 1.29, 2.29), p = .011. Conclusions: 1) Low doses of enoxaparine achieve therapeutic levels, since the first 4 hours of treatment. 2) A significant reduction of total bleeding occurred with the low doses of enoxaparin, with the same efficacy to reduce MACE during follow- up.
Translation from Spanish into English obtained. Prospective randomised controlled trial in Mexican patients with UA/NSTEMI, randomized within 48 hours of qualifying symptom onset. Compares a lower dose of LMWH (enoxaparin 0.8mg/kg/dose) to UFH. N=203. Primary outcome measures: Therapeutic serum levels of anti-Xa and major complications that included death, AMI, emergency coronary revascularization, refractory angina, and total hemorrhages. Level of Evidence: 2 Quality of Evidence: Good Direction of Evidence: Supportive of lower dose LMWH (enoxaparin) in terms of safety and efficacy.
Clark 2000 Clark, S. C., N. Vitale, et al. (2000). "Effect of low molecular weight heparin (Fragmin) on bleeding after cardiac surgery." Annals of Thoracic Surgery 69(3): 762-764. Background. Fragmin (Dalteparin, Pharmacia Ltd, Milton Keynes, UK), a low molecular weight heparin, is now recommended in the treatment of unstable angina. Due to the greater bioavailability and longer half-life of Fragmin compared with conventional heparin we postulated that this may influence postoperative bleeding after cardiac surgery for unstable angina. Methods. We investigated the influence of the agent on postoperative bleeding after cardiac surgery. Patients undergoing first-time coronary artery bypass grafting were prospectively studied in four groups: group A (n = 100) were elective patients; group B (n=60) had unstable angina and received conventional heparin intravenously until operation; group C (n=115) received Fragmin with the last dose administered more than 12 hours before surgery; and group D (n=115) received Fragmin within 12 hours of operation. Results. Patients in group D had significantly greater blood loss (p < 0.001) and increased blood transfusion than groups A, B, and C (p = 0.047). Patients receiving Fragmin more than 12 hours before surgery (group C) had similar rates of blood loss and transfusion to group B (p > 0.05) but greater than in group A (p = 0.021). There were no differences in reopening rate. Conclusions. The risks of bleeding and transfusion must be weighed against the risks of acute ischemic events if Fragmin is stopped more than 12 hours before operation. (C) 2000 by The Society of Thoracic 0666d73c299e1a1df1b16f7db322595f.doc Page 20 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Surgeons.
Prospective, non-randomised, non-blinded, cohort study of patients with ACS and unstable angina, undergoing CABGS. Hypothesis: LMWH (Fragmin) increases bleeding complications post-op compared to UFH treated patients and elective surgery controls (no anticoagulation.) Outcome measures: Blood loss in chest drains, administration of blood and blood products; Secondary outcomes: ACT measurement, resternotomy rate. Groups were equivalent but not all patients were accounted for (results of 342/390 tabulated (87.7%)) and no reason for this was reported. Aspirin treatment in UA patients may have been a confounder. Level of Evidence: 3 Quality of Evidence: Fair design and methodology. Direction of Evidence: Opposing for safety of LMWH (fragmin) given within 12 hours of CABGS. Neutral for LMWH given >12hrs ore-op vs UFH. Cohen 1997 Cohen, M., C. Demers, et al. (1997). "A comparison of low-molecular-weight heparin with unfractionated heparin for unstable coronary artery disease." New England Journal of Medicine 337(7): 447-452. Background. Antithrombotic therapy with heparin plus aspirin reduces the rate of ischemic events in patients with unstable coronary artery disease. Low-molecular-weight heparin has a more predictable anticoagulant effect than standard unfractionated heparin, is easier to administer, and does not require monitoring. Methods. In a double-blind, placebo-controlled study, we randomly assigned 3171 patients with angina at rest or non- Q-wave myocardial infarction to receive either 1 mg of enoxaparin (low-molecular-weight heparin) per kilogram of body weight, administered subcutaneously twice daily, or continuous intravenous unfractionated heparin. Therapy was continued for a minimum of 48 hours to a maximum of 8 days, and we collected data on important coronary end points over a period of 30 days. Results. At 14 days the risk of death, myocardial infarction, or recurrent angina was significantly lower in the patients assigned to enoxaparin than in those assigned to unfractionated heparin (16.6 percent vs. 19.8 percent; P=0:019). At 30 days, the risk of this composite end point remained significantly lower in the enoxaparin group (19.8 percent vs. 23.3 percent, P=0.016). The need for revascularization procedures at 30 days was also significantly less frequent in the patients assigned to enoxaparin (27.0 percent vs. 32.2 percent, P=0.001). The 30-day incidence of major bleeding complications was 6.5 percent in the enoxaparin group and 7.0 percent in the unfractionated- heparin group, but the incidence of bleeding overall was significantly higher in the enoxaparin group (18.4 percent vs. 14.2 percent, P=0.001), primarily because of ecchymoses at injection sites. Conclusions. Antithrombotic therapy with enoxaparin plus aspirin was more effective than unfractionated heparin plus aspirin in reducing the incidence of ischemic events in patients with unstable angina or non-Q-wave myocardial infarction in the early phase. This benefit of enoxaparin was achieved with an increase in minor but not in major bleeding.
ESSENCE Trial. Prospective, double-blinded, randomised, placebo controlled trial of patients with ACS/NSTEMI. N=3171. Hypothesis: To demonstrate the superiority of LMWH (enoxaparin) over UFH with respect to safety and efficacy. Primary outcome measures: Composite of death, MI or recurrent angina at 14 days. Major and minor hemorrhage. Patients were randomised within 24 hours of symptoms (recent onset rest angina lasting >10 minutes) and 96% received the study medication within 12 hours of randomisation (no median reported for time from qualifying symptom to when study drug was given.) Level of Evidence: 1 Quality of Evidence: Excellent design and methods. With respect to appropriateness to ED setting, patients were given the drug up to 36 hours from qualifying symptom. Direction of Evidence: Supportive of LMWH (enoxaparin) over UFH in terms of efficacy at 14 days and 30 days and neutral for safety (major bleeding). (Commencing treatment within 24 hours symptom onset)
Cohen 2000 Cohen, M., E. M. Antman, et al. (2000). "Impact of enoxaparin low molecular weight heparin in patients with Q- wave myocardial infarction." American Journal of Cardiology 86(5): 553-556. [No abstract] 0666d73c299e1a1df1b16f7db322595f.doc Page 21 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Post hoc subgroup meta-analysis of combined ESSENCE and TIMI 11B data on the effect of Enoxaparin on outcomes in patients with a final admission diagnosis of Q-wave MI. N=252. Primary outcomes: composite of death, MI, recurrent angina requiring revascularization. Secondary outcomes: double end point of death/MI. Results: Mean time from symptom onset to initiation of therapy 8.5 hours. Incidence of triple end point event rate was consistently lower in the Enoxaparin group compared to the UFH group and reached statistical significance at day 43 (p=0.04). Incidence of major hemorrhage was low, no difference between groups. Incidence minor hemorrhage higher in the enoxaparin group (11%) compared to the UFH group (3%), mostly injection site ecchymoses. Conclusion: LMWH (Enoxaparin) could be a useful adjunctive therapy in Q-wave MI, where other treatment options are not available.
Level of Evidence: 7 Quality of Evidence: Design and Methods fair, possibly biased as post hoc analysis and sample relatively small. Direction of Evidence: Supportive of LMWH (Enoxaparin) over UFH for patients who present with UA/NSTEMI but end up with a final diagnosis of transmural MI. Cohen 1999 Cohen, M., P. Theroux, et al. (1999). "Combination therapy with tirofiban and enoxaparin in acute coronary syndromes." International Journal of Cardiology 71(3): 273-81. BACKGROUND: Tirofiban, an intravenous glycoprotein IIb/IIIa antagonist, and enoxaparin, a low molecular weight heparin, have each been shown to be effective at reducing cardiac ischemic events compared to unfractionated heparin alone in separate trials of patients with unstable angina and non-Q-wave myocardial infarction. The combination of these agents may offer further therapeutic benefit. MATERIALS AND METHODS: Fifty-five patients with non-Q-wave myocardial infarction were randomized to receive double-blind treatment with tirofiban (0.1 microgram/kg/min i.v.) for 48-108 h coadministered with either enoxaparin (1 mg/kg sc q 12 h) (n=26) or unfractionated heparin (i.v. adjusted to activated partial-thromboplastin time) (n=27) to evaluate pharmacokinetics, pharmacodynamics, and safety. The primary objective of the study was to investigate the effect of unfractionated heparin versus enoxaparin on the plasma clearance of tirofiban. RESULTS: Coadministration of tirofiban and enoxaparin was generally well tolerated. Plasma clearance of tirofiban was 176.7+/-59.8 and 187.5+/-81.8 ml/min, respectively, for enoxaparin and unfractionated heparin-treated patients (P=NS). The mean difference was well within the prespecified criterion for comparability. Administration of tirofiban with enoxaparin vs. unfractionated heparin resulted in lesser variability and a trend towards greater inhibition of platelet aggregation using 5 microM adenosine phosphate agonist. More patients achieved target inhibition of platelet aggregation >70% in the tirofiban and enoxaparin group (84% vs. 65%, P=0.19). Median bleeding time was 21 min for tirofiban and enoxaparin vs. > or =30 min for tirofiban and unfractionated heparin (P=NS). For a given level of inhibition of platelet aggregation, bleeding time was less prolonged with tirofiban and enoxaparin than tirofiban and unfractionated heparin (adjusted mean bleeding time 19.6 vs. 24.9 min, P=0.02). Tirofiban plasma concentration and clearance were comparable whether coadministered with enoxaparin or unfractionated heparin. There were no major or minor bleeding events in either group by the TIMI criteria. INTERPRETATION: The more consistent inhibition of platelet aggregation and lower adjusted bleeding time of tirofiban and enoxaparin vs. tirofiban and unfractionated heparin support the therapeutic potential of combining these two agents. These data from the first clinical report of coadministration of a glycoprotein IIb/IIIa receptor antagonist and a low molecular weight heparin are consistent with prior data which show differential pharmacodynamic effects of enoxaparin and unfractionated heparin on platelet aggregation.
Prospective, randomised, double-blinded trial. N=55.Pilot study. Patients were randomised within 24 hours of symptoms. Level of Evidence: 2 Quality of Evidence: Design and methodology fair, small number of patients adequate power for primary outcome but study not powered for clinical event comparisons. Direction of Evidence: Neutral study in terms of primary outcome (clearance of tirofiban.) Trend towards supportive evidence for safety of LMWH (enoxaparin) over UFH with lower bleeding times, however an increase in minor cutaneous and catheterisation site bleeding was observed in the LMWH group. 0666d73c299e1a1df1b16f7db322595f.doc Page 22 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Cohen 2002 Cohen, M., P. Theroux, et al. (2002). "Randomized double-blind safety study of enoxaparin versus unfractionated heparin in patients with non-ST-segment elevation acute coronary syndromes treated with tirofiban and aspirin: The ACUTE II study." American Heart Journal 144(3): 470-477. Background: In comparison with treatment with unfractionated heparin (UFH) and aspirin (ASA), both tirofiban administered with UFH and ASA, and enoxaparin plus ASA have shown superiority in reducing cardiac ischemic events in patients with unstable angina and non-ST-segment elevation myocardial infarction. Replacing UFH with enoxaparin when tirofiban is administered to patients may offer further therapeutic benefit, but could also increase bleeding. Objective: Our objective was to provide estimates of the frequency of bleeding complications, as defined by means of the Thrombolysis In Myocardial Infarction(TIMI) group, and collect data on clinical efficacy of the combination of tirofiban with enoxaparin plus ASA. Methods: Five hundred twenty-five patients with UA/NSTEMI were treated with tirofiban coadministered with ASA and randomized to receive either UFH (n = 210) or enoxaparin (n = 315). Therapy was administered for 24 to 96 hours. Bleeding incidences were assessed until 24 hours after trial therapy was discontinued; other clinical outcomes were assessed for as long as 30 days. Results: The total bleeding rate (TIMI major + minor + loss-no-site) for the UFH group versus the enoxaparin group was 4.8% vs 3.5% (odds ratio [OR] 1.4, CI 0.6-3.4). The TIMI major and minor bleeding rates for the UFH versus the enoxaparin groups were 1.0% versus 0.3% (OR 3.0, CI 0.3-33.8) and 4.3% versus 2.5% (OR 1.7, CI 0.7-4.6). There was an increase in nuisance cutaneous and oral bleeds (<50 mL of blood loss) in the enoxaparin group. Death or myocardial infarction occurred with similar frequency in the 2 groups (9.0% vs 9.2%). However, refractory ischemia requiring urgent revascularization and rehospitalization because of unstable angina occurred more frequently in the UFH group (4.3% vs 0.6% and 7.1% vs 1.6%, respectively). Conclusions: Combination therapy with tirofiban plus enoxaparin appears safe, relative to therapy with tirofiban plus UFH.
ACUTE II study. Prospective, randomised, double-blinded trial in patients with UA/NSTEMI. N=525. Patients had symptoms of UA within 24 hours of randomisation. Patients were all treated with ASA and a G2b3a inhibitor. Primary outcomes: Incidence of bleeding complications (safety). Level of Evidence: 2 Quality of Evidence: Fair. Direction of Evidence: Neutral for safety from major bleeding events (no difference found as not powered). Opposing with regard to minor cutaneous and oral bleeding events. Supportive evidence for decreased incidence of refractory ischemia requiring PCI and readmission with ACS (although study not adequately powered).
Cohen 2003 Cohen, M., G. F. Gensini, et al. (2003). "The Safety and Efficacy of Subcutaneous Enoxaparin Versus Intravenous Unfractionated Heparin and Tirofiban Versus Placebo in the Treatment of Acute ST-Segment Elevation Myocardial Infarction Patients Ineligible for Reperfusion (TETAMI): A Randomized Trial." Journal of the American College of Cardiology 42(8): 1348-1356. OBJECTIVES: The aims of the Safety and Efficacy of Subcutaneous Enoxaparin Versus Intravenous Unfractionated Heparin and Tirofiban Versus Placebo in the Treatment of Acute ST-Segment Elevation Myocardial Infarction Patients Ineligible for Reperfusion (TETAMI) study were to demonstrate that enoxaparin was superior to unfractionated heparin (UFH) and that tirofiban was better than placebo in patients with acute ST-segment elevation myocardial infarction (STEMI) who do not receive timely reperfusion. BACKGROUND: An optimal treatment strategy has not been identified for the many STEMI patients ineligible for acute reperfusion. METHODS: A total of 1,224 patients were enrolled in 91 centers in 14 countries between July 1999 and July 2002. Patients with STEMI ineligible for reperfusion were randomized to enoxaparin, enoxaparin plus tirofiban, UFH, or UFH plus tirofiban. All patients received oral aspirin. The primary efficacy end point was the 30-day combined incidence of death, reinfarction, or recurrent angina; the primary analysis was the comparison of the pooled enoxaparin and UFH groups. RESULTS: The incidence of the primary efficacy end point was 15.7% enoxaparin versus 17.3% for UFH (odds ratio 0.89 [95% confidence interval {CI} = 0.66 to 1.21]) and 16.6% for tirofiban versus 16.4% for placebo (odds ratio 1.02 [95% CI 0.75 to 1.38]). The Thrombolysis In Myocardial Infarction (TIMI) major hemorrhage rate was 1.5% for 0666d73c299e1a1df1b16f7db322595f.doc Page 23 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
enoxaparin versus 1.3% for UFH (odds ratio 1.16 [95% CI 0.44 to 3.02]) and 1.8% versus 1% for tirofiban versus placebo (odds ratio 1.82 [95% CI 0.67 to 4.95]). CONCLUSIONS: This study did not show that enoxaparin significantly reduced the 30-day incidence of death, reinfarction, and recurrent angina compared with UFH in non-reperfused STEMI patients. However, enoxaparin appears to have a similar safety and efficacy profile to UFH and may be an alternative treatment. Additional therapy with tirofiban did not appear beneficial. (C) 2003 by the American College of Cardiology Foundation.
Prospective, randomised, double-blinded controlled study in patients with late presentation STEMI who were ineligible for reperfusion. Relevant to PH/ED setting. Level of Evidence: 1 Quality of Evidence: Excellent design and methods. Direction of Evidence: Neutral. LMWH (enoxaparin) not found to be superior to UFH in delayed presentation STEMI patients.
Correia 1995 Claudio Correia Lc, N. C. A. A. J. R. F. B. J. C. P. L. T. M. M. M. A. V. S. V. and et al. (1995). "[The role of low-molecular-weight heparin in unstable angina, acute myocardial infarction and post-elective percutaneous transluminal coronary angioplasty].[comment]. [Portuguese]." Arquivos Brasileiros de Cardiologia 65(6): 475-8. PURPOSE: To evaluate the clinical efficacy and safety of subcutaneous (SC) low molecular weight heparin (LMWH) compared to intravenous (IV) non fractioned heparin (NFH) in unstable angina, acute myocardial infarction and post-percutaneous transluminal coronary angioplasty. METHODS: From September/92 to April/94, 314 patients were randomized in two groups. Group I-- 154 patients treated with SC LMWH, using in the 1st phase SC LMWH with a dosage of 160 UaXa IC/kg/day (group IA--92 patients), and in the 2nd, a dosage of 320 UaXa IC/kg/day (group IB--62 patients). Group II--160 patients treated with IV NFH 100UI/kg (bolus), followed by 1000UI/h with adjusted dosage by activated partial thromboplastin time. RESULTS: There was not a statistically significant difference among the three groups in relation to cardiac events, hemorrhagic complications and deaths. CONCLUSION: The clinical efficacy and safety of SC LMWH in patients with unstable angina, acute myocardial infarction and post-percutaneous transluminal coronary angioplasty were similar to IV NFH with the dosages used in this study.
Full text unavailable electronically or from the AHA. Randomised single-blinded trial in patients with ACS. Level of Evidence: 2 Quality of Evidence: Unable to determine from abstract. Direction of Evidence: Neutral
Detournay 2000 Detournay, B., X. Huet, et al. (2000). "Economic evaluation of enoxaparin sodium versus heparin in unstable angina. A French sub-study of the ESSENCE trial." Pharmacoeconomics 18(1): 83-9. OBJECTIVES: To perform an evaluation from the societal perspective of the cost of treatment with enoxaparin sodium versus unfractionated heparin (UFH) in patients with unstable angina and non-Q wave myocardial infarction in France. DESIGN: Four complementary cost-minimisation analyses based on the results of the Efficacy and Safety of Subcutaneous Enoxaparin in Non-Q wave Coronary Events (ESSENCE) international trial were conducted. We assessed differences in medical resource consumption and in duration of hospital stay in the whole study population (n = 3171) and for the French patients (n = 133). RESULTS: Results were consistent for the study group as a whole and for the French subgroup. Among patients treated with enoxaparin sodium, there was a statistically significant reduction in the use of angiography and percutaneous transluminal coronary angioplasty (whole group study: p = 0.024 and 0.006, respectively) and a trend towards shorter lengths of hospital stay. The differences in angiography and angioplasty rates led to estimated average net cost savings with enoxaparin sodium of French Francs (FF)1555 per treated patient (whole study population) and FF9993 (French subgroup) [1996 values]. The analyses based on the duration of hospital stay resulted in estimated net cost savings with enoxaparin sodium of between FF1014 per treated patient (whole 0666d73c299e1a1df1b16f7db322595f.doc Page 24 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
study population) and FF2804 (French subgroup). CONCLUSION: Our study confirmed earlier results which show that enoxaparin sodium is cost saving in the treatment of unstable angina.
French sub-study of ESSENCE trial, a cost minimisation study. Hypothesis: that the net direct cost associated with all medical resources used could be considered to adequately reflect the costs of the treatment itself. N=133.Unable to confirm whether analysis is prospective or retrospective. Results consistent with US and UK ESSENCE economic sub-studies, ie LMWH (enoxaparin) is cost saving compared to UFH, mainly due to less coronary angiography and PCIs performed. Level of Evidence: 7 Quality of Evidence: Fair. Small numbers in French sub-study. Direction of Evidence: Supportive of feasibility of LMWH (Enoxaparin) in terms of overall cost benefit to 30 days compared to UFH in France. Dubois 2003 Dubois, C. L., A. Belmans, et al. (2003). "Outcome of urgent and elective percutaneous coronary interventions after pharmacologic reperfusion with tenecteplase combined with unfractionated heparin, enoxaparin, or abciximab.[see comment]." Journal of the American College of Cardiology 42(7): 1178-85. OBJECTIVES: The aim of this study was to evaluate percutaneous coronary intervention (PCI) in the Assessment of the Safety and Efficacy of New Thrombolytic Regimens (ASSENT-3) trial. BACKGROUND: In the ASSENT-3 trial, co-therapy with abciximab (ABC) or enoxaparin (ENOX) reduced ischemic complications after ST- elevation acute myocardial infarction treated with tenecteplase when compared with unfractionated heparin (UFH). The effect of these new co-therapies on the results of PCI is unknown. METHODS: Clinical outcomes in patients who received co-therapy with ABC, ENOX, or UFH and subsequently underwent an elective (n = 1,064) or urgent (n = 716) PCI in the ASSENT-3 trial were compared. RESULTS: No significant differences in clinical end points were observed in patients who underwent an elective PCI. A non-significant trend toward fewer in-hospital myocardial re-infarctions was seen with ABC and ENOX when compared with UFH (0.5% vs. 0.6% vs. 1.5%, respectively). The incidence of bleeding complications was similar in the three treatment arms. Significantly fewer ABC- and ENOX-treated patients needed urgent PCI compared with UFH (9.1% vs. 11.9% vs. 14.3%; p < 0.0001), but outcomes in these patients were in general less favorable (30-day mortality: 8.2% vs. 5.4% vs. 4.5%; 1-year mortality: 11.0% vs. 8.5% vs. 5.6%; in-hospital re-infarction: 3.9% vs. 2.5% vs. 2.7%; major bleeding complications: 8.8% vs. 7.0% vs. 3.4%). In pairwise comparisons with UFH, the higher one-year mortality and major bleeding rates after ABC were statistically significant (p = 0.045 and p = 0.012, respectively). CONCLUSIONS: Clinical outcomes after elective PCI were similar with the three antithrombotic co-therapies studied in ASSENT-3. Although fewer patients needed urgent PCI with ABC and ENOX, clinical outcomes were less favorable in this selected population, especially with ABC.
Post-hoc analysis of ASSENT-3 trial. Relevant to ED setting as used patients who presented within 6 hours of STEMI, received TNK as lytic treatment and were randomised, then underwent PCI sometime in that admission, which was categorised as early, urgent or elective. Results as above. With regard to LMWH (enoxaparin) vs UFH, in terms of efficacy, there was a trend for fewer patients to need urgent PCI, and fewer to have in-hospital reinfarction (not statistically significant); and in terms of safety, there was a modest increase in major non-cerebral bleeds, mainly puncture site related (also not statistically significant). Level of Evidence: 7 Quality of Evidence: Fair Direction of Evidence: Neutral. Eikelboom 2000 Eikelboom, J. W., S. S. Anand, et al. (2000). "Unfractionated heparin and low-molecular- weight heparin in acute coronary syndrome without ST elevation: a meta-analysis.[see comment][erratum appears in Lancet 2000 Aug 12;356(9229):600]." Lancet 355(9219): 1936-42. BACKGROUND: In acute coronary syndrome without ST elevation, the role of unfractionated and low-molecular-weight heparin in aspirin-treated patients remains unclear, and there is conflicting evidence regarding the efficacy and safety of low- molecular-weight heparin (LMWH) relative to unfractionated heparin. We did a systematic overview of the randomised trials to assess the effect of unfractionated heparin and 0666d73c299e1a1df1b16f7db322595f.doc Page 25 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
LMWH on death, myocardial infarction, and major bleeding. METHODS: Randomised trials comparing unfractionated heparin or LMWH with placebo or untreated control, or comparing unfractionated heparin with LMWH, for the short-term and long-term management of patients with acute coronary syndrome without ST elevation, were identified by electronic and manual searches and through contact with experts and industry representatives. Odds ratios for death, myocardial infarction, and major bleeding were calculated for each trial, and results for the individual trials were combined by a modification of the Mantel-Haenszel method. FINDINGS: 12 trials, involving a total of 17157 patients, were included. The summary odds ratio (OR) for myocardial infarction or death during short-term (up to 7 days) unfractionated heparin or LMWH compared with placebo or untreated control was 0.53 (95% CI 0.38-0.73; p=0.0001) or 29 events prevented per 1000 patients treated; during short-term LMWH compared with unfractionated heparin was 0.88 (0.69-1.12; p=0.34); and during long-term LMWH (up to 3 months) compared with placebo or untreated control was 0.98 (0.81-1.17; p=0.80). Long- term LMWH was associated with a significantly increased risk of major bleeding (OR 2.26, [95% CI 1.63-3.14], p<0.0001), which is equivalent to 12 major bleeds per 1000 patients treated. INTERPRETATION: In aspirin-treated patients with acute coronary syndrome without ST elevation, short-term unfractionated heparin or LMWH halves the risk of myocardial infarction or death. There is no convincing difference in efficacy or safety between LMWH and unfractionated heparin. Long-term LMWH has not been proven to confer benefit additional to aspirin and there is no evidence to support its use after the first 7 days.
Meta-analysis of 12 randomised trials comparing UFH to LMWH (or one or the other to placebo) in patients with UA/NSTEMI. Primary outcomes: Composite of death or MI (efficacy), major bleeding (safety); secondary outcomes: recurrent ischemia, need for revascularisation. Level of Evidence: 1 Quality of Evidence: Excellent Direction of Evidence: Neutral for safety and efficacy of LMWH compared to UFH. Ferguson 2004 Ferguson, J. J., R. M. Califf, et al. "Enoxaparin vs unfractionated heparin in high-risk patients with non-ST-segment elevation acute coronary syndromes managed with an intended early invasive strategy: primary results of the SYNERGY randomized trial. 45-54, 2004 Jul 7. CONTEXT: Enoxaparin has demonstrated advantages over unfractionated heparin in low- to moderate-risk patients with non-ST-segment elevation acute coronary syndromes (ACS) treated with a conservative strategy. OBJECTIVES: To compare the outcomes of patients treated with enoxaparin vs unfractionated heparin and to define the role of enoxaparin in patients with non-ST-segment elevation ACS at high risk for ischemic cardiac complications managed with an early invasive approach. DESIGN, SETTING, AND PARTICIPANTS: The Superior Yield of the New Strategy of Enoxaparin, Revascularization and Glycoprotein IIb/IIIa Inhibitors (SYNERGY) trial was a prospective, randomized, open-label, multicenter, international trial conducted between August 2001 and December 2003. A total of 10 027 high-risk patients with non-ST-segment elevation ACS to be treated with an intended early invasive strategy were recruited. INTERVENTIONS: Subcutaneous enoxaparin (n = 4993) or intravenous unfractionated heparin (n = 4985) was to be administered immediately after enrollment and continued until the patient required no further anticoagulation, as judged by the treating physician. MAIN OUTCOME MEASURES: The primary efficacy outcome was the composite clinical end point of all-cause death or nonfatal myocardial infarction during the first 30 days after randomization. The primary safety outcome was major bleeding or stroke. RESULTS: The primary end point occurred in 14.0% (696/4993) of patients assigned to enoxaparin and 14.5% (722/4985) of patients assigned to unfractionated heparin (odds ratio [OR], 0.96; 95% confidence interval [CI], 0.86-1.06). No differences in ischemic events during percutaneous coronary intervention (PCI) were observed between enoxaparin and unfractionated heparin groups, respectively, including similar rates of abrupt closure (31/2321 [1.3%] vs 40/2364 [1.7%]), threatened abrupt closure (25/2321 [1.1%] vs 24/2363 [1.0%]), unsuccessful PCI (81/2281 [3.6%] vs 79/2328 [3.4%]), or emergency coronary artery bypass graft surgery (6/2323 [0.3%] vs 8/2363 [0.3%]). More bleeding was observed with enoxaparin, with a statistically significant increase in TIMI (Thrombolysis in Myocardial Infarction) major bleeding (9.1% vs 7.6%, P =.008) but nonsignificant excess in 0666d73c299e1a1df1b16f7db322595f.doc Page 26 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
GUSTO (Global Utilization of Streptokinase and t-PA for Occluded Arteries) severe bleeding (2.7% vs 2.2%, P =.08) and transfusions (17.0% vs 16.0%, P =.16). CONCLUSIONS: Enoxaparin was not superior to unfractionated heparin but was noninferior for the treatment of high-risk patients with non-ST-segment elevation ACS. Enoxaparin is a safe and effective alternative to unfractionated heparin and the advantages of convenience should be balanced with the modest excess of major bleeding.
SYNERGY trial. Randomised controlled single-blinded trial comparing UFH to LMWH (enoxaparin) in patients with NSTEMI. N=4993. Patients received treatment within 24 hours of symptom onset (median 14 hours) and an early invasive strategy. Level of Evidence: 2 Quality of Evidence: Excellent Direction of Evidence: Neutral in terms of efficacy and opposing in terms of safety. Fox 2002 Fox, K. A. A., E. M. Antman, et al. (2002). "Comparison of Enoxaparin versus unfractionated Heparin in patients with unstable angina pectoris/non-ST-segment elevation acute myocardial infarction having subsequent percutaneous coronary intervention." American Journal of Cardiology 90(5): 477-482. Patients with unstable angina or non-ST-segment elevation myocardial infarction (MI) may undergo invasive revascularization procedures shortly after admission to hospital or after a brief period of stabilization. In the Thrombolysis In Myocardial Infarction (TIMI) 11B trial and Efficacy and Safety of Subcutaneous Enoxaparin in Non-Q-Wave Coronary Events (ESSENCE) trial 1,326 patients underwent percutaneous coronary intervention (PCI). A total of 924 patients underwent PCI during the initial hospitalization period, and of these, 445 patients did so while receiving treatment with unfractionated heparin (UFH) or the low-molecular-weight heparin, enoxaparin. This analysis compared efficacy and clinical events in the enoxaparin and UFH groups in patients who: (1) underwent PCI while on treatment versus those who did not, and (2) underwent PCI in hospital. We also compared those who did not undergo PCI. Treatment with enoxaparin (1 mg/kg given as twice daily subcutaneous injections) was beneficial and well tolerated in patients with unstable angina and non-ST-segment elevation MI who underwent PCI. Compared with UFH, enoxaparin significantly reduced the likelihood of clinical events (death and nonfatal MI after PCI) in patients who underwent PCI after 1 year (p = 0.003 for in-hospital PCI; p = 0.005 for on-treatment PCI), with a trend toward a reduced event rate at 43 days. In addition, patients treated with enoxaparin who did not undergo PCI also showed a reduction in the risk of death, nonfatal MI, and urgent revascularization when compared with those treated with UFH (significant at 43 days, with a trend persisting at 1 year). Study limitations were that PCI was nonrandomized, the analysis was post hoc, and the sample size was relatively small. Nevertheless, in the absence of large clinical trials, this study suggests that treatment with enoxaparin was well tolerated, and exhibited a similar risk of major hemorrhage to UFH in patients who underwent PCI. (C) 2002 by Excerpta Medica, Inc.
Post-hoc analysis of 2 trials (ESSENCE and TIMI 11B), of patients with UA/NSTEMI randomised to UFH or LMWH (enoxapirin) who then had PCI. Outcomes: Composite of death/MI/recurrent angina or Major bleeding. Level of Evidence: 7 Quality of Evidence: Poor, small numbers, study difficult to understand, no clear hypothesis, results seem to duplicate original studies. PCI not randomised. Direction of Evidence: Neutral with regard to safety of major bleeding event for on treatment or in-hospital PCI (no difference found between LMWH and UFH). FRAIS Investigators 1999 FRA.I.S. Investigators (1999). "Comparison of two treatment durations (6 days and 14 days) of a low molecular weight heparin with a 6-day treatment of unfractionated heparin in the initial management of unstable angina or non-Q wave myocardial infarction: FRAX.I.S. (FRAxiparine in Ischaemic Syndrome)." Eur Heart J 20(21): 1553-62. AIM: To assess the benefit of short-term low molecular weight heparin nadroparin compared with unfractionated heparin in unstable angina or non-Q wave myocardial infraction patients and to determine whether a longer, 2-week low molecular weight heparin regimen would offer additional clinical benefit. PATIENTS, METHODS AND RESULTS: This was a multicentre, prospective, randomized, double-blind study in three parallel groups, involving 3468 patients. Patients received one of three treatment 0666d73c299e1a1df1b16f7db322595f.doc Page 27 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
regimens: the unfractionated heparin group received an intravenous bolus of unfractionated heparin 5000 IU, followed by an activated partial thromboplastin time adjusted infusion of unfractionated heparin for 6+/-2 days; the nadroparin 6 group received an intravenous bolus of nadroparin 86 anti-Xa IU. kg(-1), followed by twice daily subcutaneous injections of nadroparin 86 anti-Xa IU. kg(- 1)for 6+/-2 days, and the nadroparin 14 group received an intravenous bolus of nadroparin 86 anti-Xa IU. kg(-1), followed by twice daily subcutaneous injections of nadroparin 86 anti-Xa IU. kg(-1)for 14 days. No statistically significant differences were observed between the three treatment regimens with respect to the primary outcome (cardiac death, myocardial infarction, refractory angina, or recurrence of unstable angina at day 14). The absolute differences between the groups in the incidence of the primary outcome were: -0.3% (P=0.85) for the nadroparin 6 group vs the unfractionated heparin group and +1.9% (P=0.24) for the nadroparin 14 group vs the unfractionated heparin group. Furthermore, there were no significant intergroup differences regarding any of the secondary efficacy outcomes. However, there was an increased risk of major haemorrhages in the nadroparin 14 group compared with unfractionated heparin (3.5% vs 1.6%;P=0.0035). CONCLUSIONS: Treatment with nadroparin for 6+/-2 days provides similar efficacy and safety to treatment with unfractionated heparin, for the same period, in the therapeutic management of acute unstable angina or non-Q wave myocardial infarction, and may be easier to administer. A prolonged regimen of nadroparin (14 days) does not provide any additional clinical benefit.
Prospective, randomised, double-blinded trial in patients with UA/NSTEMI. Primary outcome: cardiac death, myocardial infarction, refractory angina, or recurrence of unstable angina at day 14, secondary outcomes: above composite of cardiac events at 6 and 3 months and major hemorrhage. Same length of treatment between UFH and LMWH 6 group. 53% of patients were randomised <6 hours from their last episode of pain. Level of Evidence: 1 Quality of Evidence: Excellent design and methods. Direction of Evidence: Neutral for safety and efficacy of LMWH (Nadroparin) compared to UFH Godoy 1998 Godoy I, H. C. Z. C. K. S. A. A. C. R. (1998). "[Comparison of low-molecular-weight heparin and unfractionated heparin in the treatment of unstable angina]. [Spanish]." Revista Medica de Chile 126(3): 259-64. BACKGROUND: Low molecular weight heparin can be administered by the subcutaneous route and has a stable and prolonged antithrombotic effect. These features have prompted clinical essays about its use as an alternative to unfractionated heparin in the treatment of unstable angina. AIM: To compare the clinical effects of low molecular weight heparin and unfractionated conventional heparin in patients with unstable angina or non Q infarction. PATIENTS AND METHODS: Seventy patients (47 male) admitted to the hospital with the diagnosis of unstable angina or non Q acute myocardial infarction were randomly assigned to receive unfractionated intravenous heparin or subcutaneous low molecular weight heparin bid. All received aspirin p.o. and i.v. nitroglycerin. The incidence of recurrent angina, acute myocardial infarction or a need for emergency surgical revascularization during hospital stay were assessed in both groups. RESULTS: Compared to patients with low molecular weight heparin, patients receiving unfractionated heparin had a higher incidence of recurrent resting angina (23 and 47.5% respectively, p < 0.04) and higher need for emergency surgical revascularization (3.3 and 17.5% respectively, p < 0.06). Patients treated with unfractionated conventional heparin had a 3 times higher risk of having an adverse cardiovascular event than patients receiving low molecular weight heparin (O.R. 0.33, confidence intervals 0.11-0.58). CONCLUSIONS: Low molecular weight heparin is superior to unfractionated conventional heparin in the treatment of unstable angina and non Q acute myocardial infarction.
Spanish trial. Full text not available electronically or through AHA. From abstract, randomised single-blinded trial in patients with UA/NSTEMI. Level of Evidence: 2 Quality of Evidence: Unable to comment. Direction of Evidence: Supportive in terms of efficacy.
Goodman 2000; 1 Goodman, S. G., A. Barr, et al. (2000). "Low molecular weight heparin decreases rebound ischemia in unstable angina or non-Q-wave myocardial infarction: The Canadian 0666d73c299e1a1df1b16f7db322595f.doc Page 28 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
ESSENCE ST segment monitoring substudy." Journal of the American College of Cardiology 36(5): 1507-1513. OBJECTIVES: The goal of this study was to determine whether enoxaparin was more effective than heparin in reducing recurrent ischemic episodes. BACKGROUND: Continuous ST segment monitoring is a simple tool for assessment of ischemia and identifies patients with a worse prognosis. Little is known about the impact of low molecular weight heparin on ST segment shift. METHODS: Patients were randomized to receive enoxaparin or heparin (mean 3.4 days). Three-lead ST segment monitoring was performed for the first 48 h (n = 220) and an additional 48 h (n = 174) after intravenous study drug discontinuation (mean 1.9 days later). RESULTS: During initial monitoring, ischemia rates were similar among the heparin and enoxaparin groups (27.2% vs. 22.6%, p = 0.44); however, the time to first ischemic episode was earlier among heparin-treated patients (11 +/- 11 vs. 25 +/- 18 min, p = 0.001). After drug discontinuation, ischemic episodes occurred more frequently (44.6% vs. 25.6%, p = 0.009), and the total ischemic duration was greater among heparin patients (18 +/- 39 vs. 5 +/- 12 min/24 h, p = 0.005). Recurrent ischemia occurred more frequently after discontinuation in the heparin (46% vs. 31%, p = 0.043), but not the enoxaparin, group (18.4% vs. 25%, p = 0.33). Regardless of treatment, patients with ischemia were more likely to die or experience (re)infarction at one year (18.4% vs. 8.3%, p = 0.023). CONCLUSIONS: ST segment shift occurs frequently in unstable angina/non-Q-wave myocardial infarction despite antithrombotic therapy and is associated with worse one-year prognosis. Enoxaparin is a more effective antithrombotic treatment than unfractionated heparin and leads to greater prevention of rebound ischemia. (C) 2000 by the American College of Cardiology.
ESSENCE substudy. Prospective, randomised, double-blinded controlled trial in patients with UA/NSTEMI, applying ST segment monitoring. Hypotheses well stated. Problems with relatively small number of patients and not accounting for all patients. Some relevance to the ED setting as randomisation and treatment took part in the first 24 hours from symptom onset for the initial 48 hour monitoring period, but the outcomes from this part of the trial showed no significant difference in rates or total duration of ischemia between LMWH (enoxaparin) and UFH.
Level of Evidence: 2 Quality of Evidence: Fair design and Methods. Direction of Evidence: Supportive for efficacy of LMWH over UFH for the prevention of rebound ischemia. Goodman 2000; 2 Goodman, S. G., M. Cohen, et al. (2000). "Randomized trial of low molecular weight heparin (enoxaparin) versus unfractionated heparin for unstable coronary artery disease: One-year results of the ESSENCE study." Journal of the American College of Cardiology 36(3): 693-698. OBJECTIVES: We sought to determine whether the observed benefits of enoxaparin were maintained beyond the early phase; a one-year follow-up survey was undertaken for patients enrolled in the Efficacy and Safety of Subcutaneous Enoxaparin in Non-Q wave Coronary Events (ESSENCE) study. BACKGROUND: We have previously reported a significant benefit of low molecular weight as compared with unfractionated heparin (UFH) in the 14- and 30-day incidence of a composite end point of death, myocardial infarction (MI) or recurrent angina in patients with unstable angina or non-Q wave MI. METHODS: The study recruited 3,171 patients with recent-onset rest angina and underlying ischemic heart disease. All patients received oral aspirin daily and were randomized to receive enoxaparin subcutaneously every 12 h or UFH (intravenous bolus followed by continuous infusion) in a double-blind, double-dummy fashion for a median of 2.6 days. RESULTS: The incidence of the composite triple end point at one year was lower among patients receiving enoxaparin as compared with those receiving UFH (32.0% vs. 35.7%, p = 0.022), with a trend toward a lower incidence of the secondary composite end point of death or MI (11.5% vs. 13.5%, p = 0.082). At one year, the need for diagnostic catheterization and coronary revascularization was lower in the enoxaparin group (55.8% vs 59.4%, p = 0.036 and 35.9% vs. 41.2%, p = 0.002, respectively). CONCLUSIONS: In patients with unstable angina or non-Q wave MI, enoxaparin therapy significantly reduced the rates of recurrent ischemic events and invasive diagnostic and therapeutic procedures in the short term with sustained benefit at one year. (C) 2000 by 0666d73c299e1a1df1b16f7db322595f.doc Page 29 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
the American College of Cardiology.
ESSENCE(4) Trial – Retrospective one year follow-up results. Primary outcome: Composite triple endpoint at one year. Level of Evidence: 1 Quality of Evidence: Good Direction of Evidence: Supportive of efficacy of LMWH (Enoxaparin) compared to UFH in patients with UA/NSTEMI to one year. Goodman 2003 Goodman, S. G., D. Fitchett, et al. (2003). "Randomized evaluation of the safety and efficacy of enoxaparin versus unfractionated heparin in high-risk patients with non-ST- segment elevation acute coronary syndromes receiving the glycoprotein IIb/IIIa inhibitor eptifibatide." Circulation 107(2): 238-244. Background - Current pharmacotherapeutic options for high-risk non-ST-segment elevation acute coronary syndrome patients include aspirin, clopidogrel, heparin, and platelet glycoprotein IIb/IIIa inhibition. A key issue of uncertainty is the safety and efficacy of combination glycoprotein IIb/IIIa inhibitor and low-molecular-weight heparin therapy. Methods and Results - We randomized 746 patients with rest ischemic discomfort within 24 hours after the onset of symptoms and ST-segment deviation and/or elevation of serum cardiac markers to receive open-label enoxaparin (1 mg/kg subcutaneously twice daily) or unfractionated heparin (70-U/kg bolus; 15 U [middle dot] kg--1 [middle dot] h- -1 infusion, titrated to an activated partial thromboplastin time of 1.5 to 2 times control) for 48 hours. All patients received aspirin and eptifibatide (180-[mu]g/kg bolus; 2 [mu]g [middle dot] kg--1 - min--1 infusion). Major non- coronary artery bypass surgery-related bleeding at 96 hours (primary safety outcome) was significantly lower among enoxaparin-treated patients than among heparin-treated patients (1.8% versus 4.6%, P=0.03). Minor bleeding was more frequent in the enoxaparin group (30.3% versus 20.8%, P=0.003). Patients in the enoxaparin group were less likely to experience ischemia as detected by continuous ECG evaluation (primary efficacy outcome) during the initial (14.3% versus 25.4%, P=0.0002) and subsequent (12.7% versus 25.9%, P<0.0001) 48-hour monitoring periods. Death or myocardial infarction at 30 days was significantly lower in the enoxaparin group (5% versus 9%, P=0.031). Conclusions - When aspirin and eptifibatide are used in high-risk non-ST-segment elevation acute coronary syndrome patients, enoxaparin improves outcomes (determined on the basis of better safety and efficacy) compared with currently recommended unfractionated heparin therapy and provides a useful novel alternative therapeutic strategy.
INTERACT Trial. Prospective randomised, un-blinded trial in 746 patients with NSTEMI treated with aspirin and G2b3a inhibitor (eptifibatide) comparing the addition of LMWH (enoxaparin) or UFH. Primary outcome: Non CABG major hemorrhage (safety) and rate of recurrent ischemia (efficacy). Secondary outcomes: Composite double or triple endpoints at 30 days. Intervention was initiated after randomisation, which occurred within 24 hours of qualifying symptoms, median 4.4 hours (2.8, 7.7). Level of Evidence: 1 Quality of Evidence: Good, appropriate to ED setting. Direction of Evidence: Supportive for LMWH (enoxaparin) over UFH in combination with G2b3a Inhibitor and aspirin for NSTEMI. Gurfinkel 1995 Gurfinkel Ep, M. E. J. M. R. I. C. M. A. D. E. A. G. C. N. D. A. M. M. B. (1995). "Low molecular weight heparin versus regular heparin or aspirin in the treatment of unstable angina and silent ischemia.[comment]." Journal of the American College of Cardiology 26(2): 313-8. OBJECTIVES. This study was designed to test the hypothesis that low molecular weight heparin may lessen the severity of ischemic events in patients with unstable angina. BACKGROUND. Unstable angina is a thrombotic process that requires intensive medical treatment. Although current treatments can reduce the number of complications, serious bleeding continues to occur. Nadroparin calcium, a low molecular weight heparin, seems to be a safe therapeutic agent that does not require laboratory monitoring. METHODS. A total of 219 patients with unstable angina entered the study at a mean time of 6.17 h after the last episode of rest pain. Patients were randomized to receive aspirin (200 mg/day [group A]), aspirin plus regular heparin (400 IU/kg body weight per day 0666d73c299e1a1df1b16f7db322595f.doc Page 30 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
intravenously and titered by activated partial thromboplastin time [group B]) and aspirin plus low molecular weight heparin (214 UIC/kg anti-Xa twice daily subcutaneously [group C]). The major end points determined for the in-hospital period were 1) recurrent angina, 2) myocardial infarction, 3) urgent revascularization, 4) major bleeding, and 5) death. Minor end points were 1) silent myocardial ischemia, and 2) minor bleeding. Event rates were tested by chi-square analysis. RESULTS. Recurrent angina occurred in 37%, 44% and 21% of patients in groups A, B and C, respectively, and was significantly less frequent in group C than in either group A (odds ratio 2.26, 95% confidence interval [CI] 1 to 5.18, p = 0.03) or group B (odds ratio, 3.07, 95% CI 1.36 to 7.00, p = 0.002). Nonfatal myocardial infarction was present in seven patients in group A, four in group B and none in group C (group B vs. A, p = 0.5; group C vs. A, p = 0.01). Urgent revascularization was performed in nine patients in group A, seven in group B and one in group C (C vs. A, p = 0.01). Two episodes of major bleeding occurred in group B. Silent myocardial ischemia was present in 38%, 41% and 25% of patients in groups A, B and C, respectively, and was significantly less frequent in group C than group B (odds ratio 2.12, 95% CI 0.97 to 4.69, p = 0.04). Minor bleeding was detected in 10 patients in group B, 1 patient in group C (B vs. C, p = 0.01) and no patient in group A (A vs. B, p = 0.003). CONCLUSIONS. In this study, treatment with aspirin plus a high dose of low molecular weight heparin during the acute phase of unstable angina was significantly better than treatment with aspirin alone or aspirin plus regular heparin. Prospective randomised, single-blinded trial of patients with UA, all had the qualifying symptom of ischemic rest pain within the previous 24 hours (mean time to randomisation 6.17 hrs). Hypothesis: LMWH may lessen the severity of ischemic events in patients with UA. N=219. Endpoints as in abstract. Limitations: Study terminated early by data committee due to significant results. Level of Evidence: 2 Quality of Evidence: Fair. Small number and single blinding of heparin only (no placebo subcutaneous injections, so possibly biased. Relevant to PH/ED Setting. Direction of Evidence: Supportive of LMWH (Nadroparin) over UFH in terms of efficacy (Recurrent angina, silent ischemia and combined major events) and safety (minor bleeding). Gurfinkel 1999 Gurfinkel E, D. E. C. C. B. G. C. M. M. B. (1999). "Thrombotic reactant markers in non-ST segment elevation acute coronary syndromes treated with either enoxaparin (low molecular weight heparin) or unfractionated heparin." Journal of Thrombosis & Thrombolysis 8(3): 227-32. BACKGROUND: This study was designed to analyze the impact of treatment with either unfractionated heparin or enoxaparin (low molecular weight heparin) on plasma markers of thrombotic and endogenous thrombolytic activity in patients with non-ST segment elevation acute coronary syndromes. METHODS: A subset of 174 patients derived from the 3,171 patients of the ESSENCE study was evaluated. Eighty-seven patients were assigned to intravenous unfractionated heparin (target aPTT: 55-85 sec) (group UH), and 87 assigned to subcutaneous enoxaparin (1 mg/kg/q12hr) (group ENOX) for a minimum of 48 hours of treatment (average duration of treatment 88+/-45 hours). The thrombin time, and plasma levels of anti-factor Xa activity, prothrombin fragment F 1+2, thrombin-antithrombin complex (TAT), and D-dimer, were assayed at baseline, and at or close to peak activity 24-36 hrs, and at 72-90 hrs for those remaining on treatment with antithrombotic therapy. Major ischemic and hemorrhagic events were assessed throughout hospitalization. The levels of the thrombotic markers measured at or close to peak activity at 36 hours are presented below, and compared to clinical outcome at 30 days. RESULTS: In UH patients, the thrombin time increased 7 fold while the mean value for anti-Xa activity was 0.27 IU/ml; in ENOX patients the thrombin time increased 2.3 fold, and the mean value for anti-Xa activity was 0.83 IU/ml. In UH pts, basal levels of F 1+2, TAT, and D-dimer declined by (deltapaired) -0.8, -3. 3, and -66, respectively. In ENOX pts, basal levels of F 1+2, TAT, and D-dimer declined by (deltapaired) -0.3, -4.7, and -23, respectively. No significant differences were observed between the paired differences in thrombotic markers (UH vs ENOX), nor in the rate of recurrent ischemic events or major hemorrhage. Conclusions: In this subset of patients enrolled in the ESSENCE study, enoxaparin 1 mg/kg ql2hr significantly increased anti-Xa activity above that seen with unfractionated heparin, and reduced thrombin production without prolonging the thrombin time. The high anti-Xa activity achieved with enoxaparin was not associated with a loss of safety. 0666d73c299e1a1df1b16f7db322595f.doc Page 31 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Substudy of ESSENCE trial from Argentina. Prospective, randomised trial looking at thrombotic markers alongside the randomisation of patients with UA/NSTEMI to UFH v LMWH (Enoxaparin). N=174. Only significant difference was that anti-Xa activity was increased in the LMWH group, however, in this subgroup of patients, no significant difference was found in clinical event end- points. Not relevant to PH/ED setting. Level of Evidence: 2 Quality of Evidence: Fair. Direction of Evidence: Neutral.
Jones 2002 Jones, H. U., J. B. Muhlestein, et al. (2002). "Preoperative use of enoxaparin compared with unfractionated heparin increases the incidence of re-exploration for postoperative bleeding after open-heart surgery in patients who present with an acute coronary syndrome: Clinical investigation and reports." Circulation 106(13 SUPPL): I19-I22. Background - Enoxaparin has become an attractive therapy for use during acute coronary syndrome (ACS) because of its potential superior efficacy over unfractionated heparin (UFH), its longer activity, and its subcutaneous route of administration. However, because a significant number of patients presenting with ACS may be sent directly to open heart surgery while still on anticoagulation, it is important to understand any potential bleeding risks that may be associated with the use of enoxaparin under these circumstances. Methods - From 1998 to 2001, 1159 consecutive patients presenting with an acute coronary syndrome who received either UFH (n = 1008) or enoxaparin (n = 151) before proceeding to open heart surgery for urgent therapy during the same hospitalization were included in this study. Incidence of perioperative bleeding as evidenced by the units of blood products (packed red blood cells or platelets) transfused or the need for surgical re-exploration for postoperative bleeding was recorded. Results - Average age was 65+/-11 and 67+/-11 years for patients receiving UFH and enoxaparin, respectively (P=0.005). Seventy-five percent of those receiving UFH and 64% of those receiving enoxaparin (P<0.005) were males. After discharge, the incidence of rehospitalization for hemorrhage requiring return to surgery for re-exploration was 7.9% in the enoxaparin group and 3.7% in the UFH group (adjusted hazard ratio=2.6, P=0.03). The use of blood products did not differ between groups (UFH=2.7+/-6.5 U and enoxaparin=2.3+/-4.5 U; P=NS). Conclusion - The preoperative use of enoxaparin compared with UFH in patients presenting with an ACS who undergo open-heart surgery during the same hospitalization is associated with a significantly increased incidence of re- exploration for postoperative bleeding. Further study is needed to understand the mechanism of this phenomenon and to develop appropriate guidelines to address this potentially important issue.
Retrospective, cohort study of patients admitted with ACS/UA who received LMWH(enoxaparin) or UFH within 48 hours of subsequent cardiac surgery (CABGs or VR). Not randomised. N=1159, but only small number in enoxaparin group. Primary outcomes: Incidence and number of packed RBC transfusion, and surgical re-exploration for post-op bleeding. Secondary end point: in- hospital, post procedural death. Level of Evidence: 4 Quality of Evidence: Fair design and methods. Direction of Evidence: Opposing in terms of safety of LMWH (Enoxaparin) compared to UFH in terms of safety within 48 hours of cardiac surgery leading to an increased incidence of re- exploration for post-op bleeding. Klein 1997 Klein, W., A. Buchwald, et al. (1997). "Comparison of low-molecular-weight heparin with unfractionated heparin acutely and with placebo for 6 weeks in the management of unstable coronary artery disease: Fragmin in unstable coronary artery disease study (FRIC)." Circulation 96(1): 61-68. Background: Low-molecular-weight heparin has a number of pharmacological and pharmacokinetic advantages over unfractionated heparin that make it potentially suitable, when used in combination with aspirin, for the treatment of unstable coronary artery disease. Method and Results: Patients with unstable angina or non-Q-wave myocardial infarction (1482) were included in the study, which had two phases. In an open, acute phase (days 1 to 6), patients were assigned either twice-daily weight-adjusted 0666d73c299e1a1df1b16f7db322595f.doc Page 32 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
subcutaneous injections of dalteparin (120 IU/kg) or dose-adjusted intravenous infusion of unfractionated heparin. In the double-blind, prolonged treatment phase (days 6 to 45), patients received subcutaneously either dalteparin (7500 IU once daily) or placebo. During the first 6 days, the rate of death, myocardial infarction, or recurrence of angina was 7.6% in the unfractionated heparin- treated patients and 9.3% in the dalteparin-treated patients (relative risk, 1.18; 95% confidence interval [CI], 0.84 to 1.66). The corresponding rates in the two treatment groups for the composite end point of death or myocardial infarction were 3.6% and 3.9%, respectively (relative risk, 1.07; 95% CI, 0.63 to 1.80). Revascularization procedures were undertaken in 5.3% and 4.8% of patients in unfractionated heparin and dalteparin groups, respectively (relative risk, 0.88; 95% CI, 0.57 to 1.35). Between days 6 and 45, the rate of death, myocardial infarction, or recurrence of angina was 12.3% in both the placebo and dalteparin groups (relative risk, 1.01; 95% CI, 0.74 to 1.38). The corresponding rates for death or myocardial infarction were 4.7% and 4.3% (relative risk, 0.92; 95% CI, 0.54 to 1.57). Revascularization procedures were undertaken in 14.2% and 14.3% of patients in the placebo and dalteparin groups, respectively. Conclusions: Our results add to previous evidence suggesting that the low-molecular-weight heparin dalteparin administered by twice-daily subcutaneous injection may be an alternative to unfractionated heparin in the acute treatment of unstable angina or non-Q- wave myocardial infarction. Prolonged treatment with dalteparin at a lower once-daily dose in our study did not confer any additional benefit over aspirin (75 to 165 mg) alone.
FRIC trail – Prospective, randomised trial of 1499 patients with UA/NSTEMI symptoms in the preceding 72 hours. 2 phases to trial, acute phase (day 1-6, unblinded, comparing LMWH, dalteparin to UFH) relevant for PH/ED setting although concern as some of the patients were not randomised until up to 72 hours after their last episode chest pain, and prolonged blinded phase, comparing dalteparin to placebo. Primary outcomes: composite of death, MI or recurrent angina in 2nd phase of study (efficacy) and major and minor hemorrhage and thrombocytopenia (safety). Secondary outcomes: Composite endpoints in 1st phase of study and requirement for revascularization. Trial finds no significant difference in 2nd phase of study in terms of efficacy, but an increased number of minor bleed in the 2nd phase, no difference in major or minor bleeds in the acute phase and no difference in composite end points. The single end point of death is higher in the acute phase in the LMWH group 11 (1.5%) compared to 3(0.4%) in the UFH group (p=0.05). This is discussed as a borderline increase in mortality and it is stated that the study was not powered to find differences in the acute phase. Level of Evidence:2 Quality of Evidence: Fair design and methods. (Maybe poor given unblinded nature in acute phase, and not powered to find a difference between groups) Direction of Evidence: Neutral for efficacy and safety of LMWH (Dalteparin) compared to UFH in the acute phase of treatment. Klein 2003 Klein, W., W. Kraxner, et al. (2003). "Patterns of use of heparins in ACS: Correlates and hospital outcomes: The Global Registry of Acute Coronary Events (GRACE)." Thrombosis & Haemostasis 90(3): 519-527. A systematic study that compares the patterns of use of unfractionated heparin (UFH) and low-molecular-weight heparin (LMWH) in patients with acute coronary syndromes (ACS) has, to date, not been carried out in the 'real-world' setting. The aim of this report is to identify patterns of use of UFH and LMWH and to report their correlates and outcomes in a broad spectrum of ACS patients enrolled in the observational Global Registry of Acute Coronary Events (GRACE). The use of LMWH and UFH was analysed in 13,231 ACS patients according to patient history, concomitant treatment and invasive procedures in US and non-US sites. Frequency of use in hospitals with and without facilities for percutaneous coronary interventions (PCI) was investigated, and outcomes were analysed. Results show that younger patients (<60 years), those receiving antiplatelet therapies, thrombolytics, beta-blockers, angiotensin-converting enzyme inhibitors, patients admitted to hospitals with PCI facilities, and patients undergoing invasive procedures were more likely to receive UFH, or both UFH and LMWH than LMWH alone (80.1% enoxaparin, 19.9% other LMWH). LMWH was used less often in US than non-US sites. After adjusting for confounding variables, patients receiving LMWH had significantly lower rates of hospital mortality (P=0.009) and major bleeding (P<0.0001). Similar results were observed in patients with ST-segment elevation myocardial infarction 0666d73c299e1a1df1b16f7db322595f.doc Page 33 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
and non-ST-segment elevation myocardial infarction or unstable angina. We can conclude that UFH tends to be used more frequently than LMWH, but hospital outcomes appeared to be better with LMWH after adjusting for covariables.
Post hoc analysis of patients entered in GRACE (Global registry of Acute Coronary Events). Time between symptom onset and treatment initiation not reported. Enoxaparin was the LMWH 80% of the time. Level of Evidence: 7 Quality of Evidence: Good design and methods. Direction of Evidence: Supportive of LMWH compared to UFH in terms of efficacy and safety. Kovar 2002 Kovar, D., J. G. Canto, et al. (2002). "Safety and effectiveness of combined low molecular weight heparin and glycoprotein IIb/IIIa inhibitors." American Journal of Cardiology 90(9): 911-915. This study examines the safety and efficacy of low molecular weight heparin (LMWH) in combination with platelet glycoprotein (GP) IIb/IIIa inhibitors in patients with acute myocardial infarction (AMI). LMWH has been shown to be as effective as unfractionated heparin (UFH) in the treatment of acute coronary syndrome (ACS), but there are limited data regarding the safety and efficacy of LMWH in combination with GP IIb/IIIa inhibitors. We studied 37,320 patients in the National Registry of Myocardial Infarction 3 who were treated with GP IIb/IIIa receptor antagonists from April 1998 to September 2000. Using univariate analysis, clinical events were compared between 2,482 patients who received LMWH and 34,838 patients who were treated with UFH. To adjust for confounding covariates, a multivariate regression analysis was also performed. Major bleeding rates were 4.0% in patients on LMWH versus 4.2% in patients who were treated with UFH (odds ratio [OR] 0.99, 95% confidence interval [CI] 0.80 to 1.23, p = 0.92). Similarly, there was no significant difference in the occurrence of recurrent myocardial ischemia (OR 0.93, 95% CI 0.82 to 1.06, p = 0.26), and in-hospital death (OR 0.86, 95% CI 0.71 to 1.05, p = 0.14) between groups. There was a trend toward a decreased risk of recurrent AMI in patients who received LMWH compared with those on UFH (1.5% vs 1.9%, OR 0.74, 95% CI 0.53 to 1.05, p = 0.09). LMWH appears to be a safe and effective alternative to UFH in patients with AMI who receive IIb/IIIa inhibitors. (C) 2002 Excerpta Medica, Inc.
Patient group included all AMI (STEMI and NSTEMI) who were treated with a G2b3a Inhibitor and either UFH or LMWH. Level of Evidence: 7. Extrapolation of data from US national registry of MI Quality of Evidence: Good methods for level 7 trial. Direction of Evidence: Neutral Le Nguyen 2001 Le Nguyen, M. T. and F. A. Spencer (2001). "Low molecular weight heparin and unfractionated heparin in the early pharmacologic management of acute coronary syndromes: A meta-analysis of randomized clinical trials." Journal of Thrombosis & Thrombolysis 12(3): 289-295. Background: The standard of care in Acute Coronary Syndromes (ACS) includes a full complement of antischemic and antithrombotic therapy. Although aspirin is used widely and concomitant anticoagulation is recommended, the comparative benefits of low molecular weight heparin (LMWH) and unfractionated heparin (UFH) have not been defined. Methods/results: A meta-analysis including all randomized clinical trials comparing LMWH and UFH for the treatment of non-ST segment elevation acute coronary syndromes was performed. Risk ratios (RR), using the DerSimonian-Laird Model, were calculated from a total of 13,320 patients. Death (RR 0.98, 95% CI 0.73-1.31), death and myocardial infarction (MI) (RR 0.86, 95% CI 0.74-1.01), death, MI, recurrent angina or revascularization (RR 0.89, 95% CI 0.74-1.07) and major hemorrhage (RR 1.01, 95% CI 0.81-1.25) occurred with similar frequencies for the anticoagulant-based strategies. Conclusions: Fixed dose LMWH therapy given subcutaneously compares favorably with UFH titrated to a target level of anticoagulation and should be considered a safe, effective, and clinically acceptable alternative in the early management of patients with non-ST segment elevation ACS. The superiority of LMWH preparations characterized by high in vitro factor Xa to thrombin inhibitory capacity is supported by clinic trial data but requires further investigation. 0666d73c299e1a1df1b16f7db322595f.doc Page 34 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
A meta-analysis. Hypothesis: To determine the benefit of LMWH compared to UFH in the early management of ACS. 14% risk reduction for Death and MI for LMWH versus UFH (p=0.06). Level of Evidence: 1 Quality of Evidence: Excellent design and methods. Direction of Evidence: Neutral with regard to efficacy and safety. Magee 2004 Magee, K. D., W. Sevcik, et al. (2004). "Low molecular weight heparins versus unfractionated heparin for acute coronary syndromes." Cochrane Database of Systematic Reviews 2: 2. Background:, Acute coronary syndromes (ACS) are an important source of morbidity and mortality. Despite weak evidence for the use of unfractionated heparin (UFH) for acute coronary syndromes it is considered an accepted treatment for unstable angina and non-ST segment elevation myocardial infarction (MI). However, evidence suggests low molecular weight heparins (LMWH) are safer and more effective than UFH in the treatment and prevention of other thrombotic disorders., Objectives:, To assess the effects of LMWH compared to UFH for acute coronary syndromes., Search strategy:, We searched the Cochrane Controlled Trials Register (the Cochrane Library issue 4, 2000), MEDLINE (January 1966 to December 2000), EMBASE (1980 to December 2000) and CINAHL (1982 to December 2000) and reference lists of articles. Authors of all include studies and pharmaceutical industry representatives were contacted to determine if unpublished studies which met the inclusion criteria were available., Selection criteria:, Randomized controlled trials of subcutaneous LMWH versus intravenous UFH in people with acute coronary syndromes (unstable angina or non-ST segment elevation MI)., Data collection and analysis:, Two reviewers independently assessed quality of studies. Data were extracted independently by two reviewers. Study authors were contacted to verify and clarify missing data., Main results:, We identified 27 potentially relevant studies, 7 studies (11,092 participants) were included in this review., We found no evidence for difference in overall mortality between the groups treated with LMWH and UFH (RR = 1.0; 95% CI: 0.69, 1.44)., Some pooled outcomes showed some evidence of heterogeneity, few of the pooled outcomes were statistically heterogeneous most were homogeneous., LMWH reduced the occurrence of MI (RR = 0.83; 95% CI: 0.70, 0.99) and the need for revascularization procedures (RR = 0.88; 95% CI: 0.82, 0.95). We found no evidence for difference in occurrence of recurrent angina (RR = 0.83; 95% CI: 0.68, 1.02), major bleeds (RR = 1.00; 95% CI: 0.80, 1.24) or minor bleeds (RR = 1.40; 95% CI: 0.66, 2.90). A decrease in the incidence of thrombocytopenia (RR = 0.64; 95% CI: 0.44, 0.94) was observed for patients given LMWH. From these results, 125 patients need to be treated with LMWH to prevent 1 additional MI and 50 patients need to be treated to prevent 1 revascularization procedure. Insufficient data exist to compare different types of LMWH., Conclusions:, LMWH and UFH had similar risk of mortality, recurrent angina, and major or minor bleeding but LMWH had decreased risk of MI, revascularization and thrombocytopenia. New Trials with longer follow up are required.
Cochrane Systematic review/meta-analysis. Relevant to ED setting, but based on trials where treatment was given within 24 – 72 hours symptoms. Proposes need for trials done in ED setting (within first 4 hours). Level of Evidence: 1 Quality of Evidence: Excellent Direction of Evidence: Supportive of LMWH compared to UFH in terms of efficacy and safety for patients with high risk UA/NSTEMI. Still recommends UFH in centre where primary PCI is available and likely to be performed. Malhotra 2001; 1 Malhotra, S., V. K. Bhargava, et al. (2001). "A randomized trial to compare the efficacy, safety, cost and platelet aggregation effects of enoxaparin and unfractionated heparin (the ESCAPEU trial)." International Journal of Clinical Pharmacology & Therapeutics 39(3): 110-115. Objective: To compare the efficacy, safety, cost and effects on platelet aggregation of unfractionated heparin and low-molecular weight heparin in unstable angina patients. Patients and methods: Ninety-three patients with unstable angina were randomized to receive either unfractionated heparin (UFH) or enoxaparin in an open design clinical trial with blinded end point evaluation. The effects of the heparins on platelet aggregation were also compared. Results: The composite end point of myocardial 0666d73c299e1a1df1b16f7db322595f.doc Page 35 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
infarction, cardiac death, recurrent angina and need for intervention was observed in 62% of patients treated with UFH and in 37% of patients treated with enoxaparin (RR 1.7, 95%CI 0.75 to 3.71, p = 0.04). There was no difference in the frequency of severity of adverse events. A cost-effectiveness analysis showed both the heparins to be similar. Platelet aggregation was inhibited to a greater extent by UFH when compared to enoxaparin. Conclusions: Enoxaparin appears to be superior in efficacy to UFH and similar to UFH in safety. No difference in costs was detected in this study. The greater inhibition of platelet aggregation observed in the case of UFH compared to enoxaparin indicates that there may be more bleeding complications with UFH.
Prospective, randomised single-blinded trial in patients with UA with symptoms occurring within 72 hours. N=93. Enoxaparin was given as1mg/kg subcutaneously, without an initial IV bolus. Primary outcome: composite of death, MI, recurrent angina or revascularisation (efficacy) and major and minor bleeding complications (safety) within 7 days. A cumulative cost analysis was also done. (feasibility). Level of Evidence: 2 Quality of Evidence: Fair. Direction of Evidence: Supportive in terms of efficacy for LMWH (enoxaparin) compared to UFH. Neutral for safety and total cost.
Malhotra 2001; 2 Malhotra, S., R. S. Karan, et al. (2001). "A meta-analysis of controlled clinical trials comparing low-molecular weight heparins with unfractionated heparin in unstable angina." Indian Heart Journal 53(2): 197-202. Background: Unfractionated heparin has been used extensively for the treatment of unstable angina/non-Q wave myocardial infarction but it has several disadvantages. Low-molecular weight heparins are now recommended although they are 3-5 times costlier than unfractionated heparin since they are convenient to administer and do not require activated thromboplastin time monitoring. Whereas enoxaparin, a low-molecular weight heparin, has been demonstrated to be superior to unfractionated heparin, the results of other low-molecular weight heparins have not been so convincing. Method and Results: Through manual. MEDLINE and EMBASE search, we identified five randomized trials (excluding enoxaparin trials) that compared low-molecular weight heparins with unfractionated heparin in unstable angina. The prespecified efficacy end point of interest included a composite of death, myocardial infarction, recurrent angina and urgent revascularization. The safety end point was taken as a composite of major hemorrhage, minor hemorrhage, thrombocytopenia, allergic reaction and any other adverse event. We calculated odds ratio (95% confidence interval) for each trial for the composite end point, and the pooled odds ratio (95% confidence interval) was calculated using two established methods of meta-analysis, the Mantel-Haenszel-Peto method and the DerSirmonian-Laird method. Both the methods yielded similar odds ratio (95% confidence interval). Separate odds ratio were calculated for efficacy and safety end points. There was a nonsignificant reduction in the incidence of the composite efficacy end point: the odds ratio (95% confidence interval) was 0.83 (0.70-0.99: p=0.08). The odds ratio (95% confidence interval) for the safety data was 0.78 (0.69-1.26: p=0.33). Conclusions: No statistically significant difference was observed when the efficacy and safety of low-molecular weight heparins were compared with those of unfractionated heparin. A cost-effectiveness analysis of low- molecular weight heparins versus unfractionated heparin must be done urgently to establish more firmly the place of low-molecular weight heparins in the management of unstable angina.
Meta-analysis of trials comparing LMWH (other than enoxaparin) to UFH in patients with UA/NSTEMI. Includes 5 trials. Primary outcome: composite of death, MI, recurrent angina or revascularisation (efficacy), major and minor bleeding complications (safety). Results as above. Problem: Tests for trial heterogeneity positive for efficacy end point. Level of Evidence: 1 Quality of Evidence: Fair Direction of Evidence: Neutral for comparison of LMWHs other than enoxaparin in terms of efficacy and safety.
Mark 1998 Mark, D. B., P. A. Cowper, et al. (1998). "Economic assessment of low-molecular-weight 0666d73c299e1a1df1b16f7db322595f.doc Page 36 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
heparin (enoxaparin) versus unfractionated heparin in acute coronary syndrome patients: Results from the ESSENCE randomized trial." Circulation 97(17): 1702-1707. Background - In the ESSENCE trial, subcutaneous low-molecular-weight heparin (enoxaparin) reduced the 30-day incidence of death, myocardial infarction, and recurrent angina relative to intravenous unfractionated heparin in 3171 patients with acute coronary syndrome (unstable angina or non-Q-wave myocardial infarction). No increase in major bleeding was seen. Methods and Results - Of the 936 ESSENCE patients randomized in the United States, 655 had hospital billing data collected. For the remainder, hospital costs were imputed with a multivariable linear regression model (R2=.86). Physician fees were estimated from the Medicare Fee Schedule. During the initial hospitalization, major resource use was reduced for enoxaparin patients, with the largest effect seen with coronary angioplasty (15% versus 20% for heparin, P=.04). At 30 days, these effects persisted, with the largest reductions seen in diagnostic catheterization (57% versus 63% for heparin, P=.04) and coronary angioplasty (18% versus 22%, P=.08). All resource use trends seen in the US cohort were also evident in the overall ESSENCE study population. In the United States, the mean cost of a course of enoxaparin therapy was $155, whereas that for heparin was $80. The total medical costs (hospital, physician, drug) for the initial hospitalization were $11 857 for enoxaparin and $12 620 for heparin, a cost advantage for the enoxaparin arm of $763 (P=.18). At the end of 30 days, the cumulative cost savings associated with enoxaparin was $1172 (P=.04). In 200 bootstrap samples of the 30-day data, 94% of the samples showed a cost advantage for enoxaparin. Conclusions - In patients with acute coronary syndrome, low- molecular-weight heparin (enoxaparin) both improves important clinical outcomes and saves money relative to therapy with standard unfractionated heparin.
Prospective, in-hospital cost analysis of the US cohort of ESSENCE patients. N=655. Outcomes: LMWH (Enoxaparin) saved money compared to UFH, mainly due to reductions in diagnostic angiography and PCI. Not directly relevant to PH or ED setting costs.
Level of Evidence: 7 Quality of Evidence: Fair, sample may be biased by US only group, but study tried to address this by also applying US cost weights to non-US group resources used. Direction of Evidence: Supportive of LMWH (Enoxaparin) in terms of overall cost benefit to 30 days in the USA. Mattioli 1999 Mattioli Av, C. E. T. G. L. S. L. S. S. M. G. (1999). "Efficacy and tolerability of a very low molecular weight heparin compared with standard heparin in patients with unstable angina: a pilot study." Clinical Cardiology 22(3): 213-7. BACKGROUND: Unstable angina is an active thrombotic process that involves thrombus formation and platelets. It requires a rapid and intensive treatment with anticoagulants and antiplatelets. HYPOTHESIS: The aim of the present study was to compare the efficacy of a very low molecular weight heparin, OP 2000, with standard heparin in the treatment of unstable angina. Tolerance and safety were also assessed. METHODS: The study population included 120 consecutive hospitalized patients with unstable angina randomized for treatment with very low molecular weight heparin or with standard heparin. The dosage of the study drug was 200 mg intramuscular (i.m.) the first day followed by 150 mg IM/day. The control drug was standard heparin starting at a dosage of 5,000 UI/ml intravenously (i.v.) and followed by continuous infusion at an activated partial thromboplastin time-adjusted dosage. The primary end points were death, acute myocardial infarction, urgent revascularization, and recurrence of angina. Tolerability was assessed using bleeding parameters, thrombocytopenia, and allergic reactions. RESULTS: Fourteen clinical events were reported in the study group compared with 25 events in the control group (p < 0.05). No adverse events were reported in either group. CONCLUSION: During the acute phase of unstable angina, treatment with a very low molecular weight heparin plus aspirin was more effective than treatment with standard heparin plus aspirin.
Prospective, randomised, non-blinded pilot study in patients with UA symptoms within 60 hours of commencement of either UFH or very LMWH. N=120. Primary end points as described in abstract. Trial was terminated early after interim analysis showed a significant reduction in 0666d73c299e1a1df1b16f7db322595f.doc Page 37 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
composite of major events and recurrent angina in the very LMWH group compared to the UFH group. Level of Evidence: 2 Quality of Evidence: Fair design and methods. Direction of Evidence: Supportive of a very LMWH compared to UFH in terms of efficacy, neutral in terms of safety. Montalescot 2003 Montalescot, G., C. Bal-dit-Sollier, et al. (2003). "Comparison of effects on markers of blood cell activation of enoxaparin, dalteparin, and unfractionated heparin in patients with unstable angina pectoris or non-ST-segment elevation acute myocardial infarction (the ARMADA study)." American Journal of Cardiology 91(8): 925-930. The low-molecular-weight heparins (LMWHs) enoxaparin and dalteparin have shown superior and equivalent efficacy, respectively, over unfractionated heparin (UFH) in patients with unstable angina pectoris (UAP) or non-ST-segment elevation myocardial infarction (NSTEMI). This study aimed to identify markers of blood cell activation that are independent predictors of outcomes at 1 month and to compare the effects of enoxaparin, dalteparin, and UFH on any such markers. In this multicenter, prospective, open-label study, 141 patients with UAP or NSTEMI were randomized to treatment for 48 to 120 hours with enoxaparin (n = 46), dalteparin (n = 48), or UFH (n = 47). Blood samples were taken at the time of randomization and after >=48 hours of treatment but before catheterization. Multivariate analysis identified increased plasma levels of von Willebrand factor (vWF) and decreased platelet levels of glycoprotein Ib/IX complexes as independent predictors of 1-month adverse outcome (a composite of death, myocardial infarction, and recurrent ischemia). vWF release was strongly related to and may have been released by inflammation as measured by C-reactive protein. Both LMWHs reduced the release of vWF in plasma (as well as C-reactive protein) compared with UFH. Enoxaparin had a more favorable effect on glycoprotein Ib/IX complexes than either dalteparin or UFH. The incidence of the composite clinical efficacy end point was: 13% (enoxaparin), 19% (dalteparin), and 28% (UFH). vWF and its receptor glycoprotein Ib/IX play a key role in acute coronary syndromes. vWF is linked to inflammation and, like glycoprotein Ib/IX, is affected more favorably by the LWMHs than by UFH. (C) 2003 by Excerpta Medica, Inc. Prospective, randomised, non-blinded trial in patients with UA/NSTEMI. Symptoms occurring within the last 48 hours. Primary outcome: death, MI, recurrent ischaemia requiring readmission or revascularisation at 30 days (efficacy) and major or minor hemorrhage (safety). N=141. Trend towards decreased incidence of composite end point between enoxaparin and UFH (p=0.08) but small numbers. Level of Evidence: 2 Quality of Evidence: Fair (non-blinded). Direction of Evidence: Neutral in terms of efficacy and safety of LMWH over UFH. O'Brien 2000 O'Brien, B. J., A. Willan, et al. (2000). "Will the use of low-molecular-weight heparin (enoxaparin) in patients with acute coronary syndrome save costs in Canada?" American Heart Journal 139(3): 423-429. Background: One-year follow-up data from the Efficacy and Safety of Subcutaneous Enoxaparin in Non-Q-Wave Coronary Events (ESSENCE) trial show that use of low-molecular-weight heparin (enoxaparin) compared with unfractionated heparin in patients hospitalized with unstable angina or non- Q-wave myocardial infarction is associated with a 10% reduction in the cumulative 1-year risk of death, myocardial infarction, or recurrent angina. Given the higher acquisition cost of enoxaparin relative to unfractionated heparin, we assessed whether the reduced use of revascularization procedures and related care makes enoxaparin a cost-saying therapy in Canada. Methods and Results: We analyzed cumulative 1-year resource use data on the 1259 ESSENCE patients enrolled in Canadian centers (40% of the total ESSENCE sample). Patient- specific data on use of drugs, diagnostic cardiac catheterization, percutaneous transluminal coronary angioplasty, coronary artery bypass grafting, and hospital days were available from the initial hospital stay and cumulative to 1 year. Hospital resources were costed with the use of data from a teaching hospital in southern Ontario that is a participant in the Ontario Case Costing Project. During the initial hospital stay, use of enoxaparin was associated with reduced use of diagnostic catheterization and revascularization procedures, with the largest effect being reduced use of percutaneous transluminal coronary angioplasty (15.0% vs 10.6%; P = .03). At 1 year, the reduced risk and costs of revascularization more than offset increased drug costs for enoxaparin; 0666d73c299e1a1df1b16f7db322595f.doc Page 38 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
producing a cost-saving per patient of $1485 (95% confidence interval $-93 to $3167; P = .06). Sensitivity analysis with lower hospital per diem costs from a community hospital in Ontario still predicts cost savings of $1075 per patient over a period of 1 year. Conclusions: The acquisition and administration cost of enoxaparin is higher than for unfractionated heparin ($101 vs $39), but in patients with acute coronary syndrome, the reduced need for hospitalization and revascularization over a period of 1 year more than offsets this initial difference in cost. Evidence from this Canadian substudy of ESSENCE supports the view that enoxaparin is less costly and more effective than unfractionated heparin in this indication. Post-hoc analysis of the Canadian subset of the ESSENCE trial at 1 year. Hypothesis: The 1 year cumulative mean cost per patient treated initially with enoxaparin is less than for patients receiving UFH, and that this will be achieved through reduced use of PTCA and CABG. N=1259 Level of Evidence: 7 Quality of Evidence: Good design (6.7% patients lost to follow-up, but included at last contact time.) Direction of Evidence: Supportive of initial treatment with LMWH (enoxaparin) over UFH in terms of feasibility (overall cost saving) in patients with UA/NSTEMI in Canada. Ocampo 1999 Ocampo, S., S. Solorio, et al. (1999). "Low molecular weight heparin in unstable angina pectoris. [Spanish]." Archivos del Instituto de Cardiologia de Mexico 69(3): 222-227. We studied the therapeutic effect of standard heparin (HS) compared with low molecular weight (HBPM) in two homogeneous groups of 14 patients heparin selected at random, with clinical history and electrocardiographic signs of unstable angina pectoris. Patients received the conventional treatment with platelets' inhibitors, nitrates, adrenergic beta blockers or calcium antagonists. Both heparins, separately, showed statistical therapeutic effect on the symptoms and signs of unstable angina pectoris. They decreased to zero the number and duration of symptomatic myocardial ischemic events observed by ambulatory electrocardiogram (EKG-Holter). The symptoms of the angina pectoris disappeared at the same elapsed time: in 51.9 +/- 20.2 min. for the HS, and in 48.14 +/- 20.7 min. for the HBPM. They decreased the frequency of the silent myocardial ischemia observed at the EKG-Holter: 9 events decreased to 4 with the HS, and 8 events decreased to 3 with the HBPM. They decreased the total elapsed time of the silent ischemia from 52 min. to 15 min., and the mean elapsed time of the silent ischemia decreased from 3.71 +/- 3.29 min. to 1.07 +/- 1.81 min. with the HS (P < 0.001). With HBPM it decreased the total elapsed time of the silent ischemia from 60 min to 10 min, and the mean elapsed time of the silent ischemia decreased from 4.28 +/- 4.49 min. to 0.71 +/- 1.43 min. (P < 0.02). Both heparins considerably decreased the frequency of the lethal arrhythmias. Although in this study we did not find statistical differences in the therapeutic action of either heparins, HBPM reduced rapidly angina symptoms and the events associated to angina pectoris, cardiac arrhythmias, specially lethal extrasystolia, conduction defects and atrial paroxistic tachycardia. Compared to HS, HBPM is easily applied, does not produce side effects on coagulation or bleeding time.
Full text unavailable electronically or from the AHA. Level of Evidence: Unable to determine from abstract. Quality of Evidence: Unable to determine from abstract. Direction of Evidence: Neutral from abstract
Orlewska 2003 Orlewska, E., A. Budaj, et al. (2003). "Cost-effectiveness analysis of enoxaparin versus unfractionated heparin in patients with acute coronary syndrome in Poland: Modelling study from the hospital perspective." Pharmacoeconomics 21(10): 737-748. Aim and perspective: To estimate the cost effectiveness of enoxaparin versus unfractionated heparin (UFH) in patients with acute coronary syndrome (ACS) from a Polish hospital perspective. This was intended to facilitate the decision-making process in selecting the most cost-effective treatment for ACS. Method: A decision model was used to quantify costs and effectiveness of alternative treatments. Published results from the Efficacy and Safety of Subcutaneous Enoxaparin in Non-Q-Wave Coronary Events (ESSENCE) study were used to estimate the probability for clinical endpoints (death, myocardial infarction or recurrent angina) at 30 days. Probabilities of patients undergoing revascularisation procedures were obtained from the Global Registry of Acute Coronary Events (GRACE) which included data from 961 patients at six centres in Poland. The 0666d73c299e1a1df1b16f7db322595f.doc Page 39 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
analysis assessed only direct medical costs, determined from actual resource consumption on a patient-specific basis (6-month observational study) and estimated using Polish data on unit costs. One- and two-way sensitivity analyses and threshold analysis were performed. Results: At 30 days, 19.8% of patients receiving enoxaparin compared with 23.3% of those receiving UFH reached a composite endpoint consisting of death, myocardial infarction and recurrent angina (p = 0.02). The average costs (in zloty [Z1]; $US1 = Z14 [2000 values]) were 1085 per patient receiving enoxaparin compared with 1097 per patient receiving UFH. Therefore, for every 29 patients treated, not only would enoxaparin therapy avoid one event of the composite endpoint, it would also save Z1348. The threshold analysis suggests that enoxaparin would lose dominance when the cost of enoxaparin increased by 10%, the cost of monitoring UFH therapy decreased by 12%, the probability of reaching the composite endpoint in the enoxaparin arm increased to 0.22 or decreased to 0.21 in the UFH arm. Conclusion: According to our model enoxaparin was more effective at a lower cost than UFH, therefore this treatment was shown to be dominant for patients with ACS in Poland.
Post hoc analysis of ESSENCE and GRACE data were used to obtain probability of clinical end points for polish patients with ACS. A decision model was used to estimate costs of LMWH compared to UFH in Polish currency. Level of Evidence: 7 Quality of Evidence: Poor. Direction of Evidence: Supportive of LMWH compared to UFH in terms of feasibility (cost). Peters 2001 Peters, R. J. G., W. Spickler, et al. (2001). "Randomized comparison of a novel anticoagulant, vasoflux, and heparin as adjunctive therapy to streptokinase for acute myocardial infarction: Results of the VITAL study (vasoflux international trial for acute myocardial infarction lysis)." American Heart Journal 142(2): 237-243. Background: Vasoflux is a low-molecular-weight heparin derivative that inhibits factor IXa activation of factor X and catalyzes fibrin-bound thrombin inactivation by heparin cofactor II. We studied whether vasoflux improves the results of thrombolysis with streptokinase for acute myocardial infarction. Methods and Results: We randomized 277 patients with acute myocardial infarction to standard intravenous unfractionated heparin (UFH) or intravenous vasoflux 1, 4, 8, or 16 mg/kg as a bolus followed by 1, 4, 8, or 16 mg/kg per hour infusion, on top of streptokinase and aspirin, until angiography at 90 minutes. Patency and corrected Thrombolysis in Myocardial Infarction (TIMI) frame count were studied at 60 and 90 minutes. Rates of TIMI grade 3 flow with vasoflux at any dose (35% to 42%) were not different from UFH (41%) at either time point, nor was the corrected TIMI frame count. However, there was an excess of bleeding in the patients randomized to vasoflux 8 or 16 mg/kg: 78% and 71%, compared with 53% for UFH (P = . 004 and .043, respectively). Major bleeding was observed in 13% and 28% at these vasoflux doses compared with 8% with UFH (P = .558 and .01, respectively). Conclusion: At doses that increase the risk of bleeding, the addition of vasoflux to streptokinase and aspirin did not lead to improved patency rates compared with UFH. Targeting factor IXa and heparin cofactor II may not be a useful adjunct to thrombolysis.
Prospective, randomises, single-blinded trial in patients presenting within 6 hours of onset of STEMI. Comparison of escalating doses of vasoflux (LMWH derivative) and UFH as adjunct therapy to SK and aspirin prior to PCI. Level of Evidence: 2 Quality of Evidence: Fair design and methods. Direction of Evidence: Opposing in terms of safety of vasoflux compared to UFH in adjunctive STEMI treatment. Petersen 2004 Petersen, J. L., K. W. Mahaffey, et al. (2004). "Efficacy and bleeding complications among patients randomized to enoxaparin or unfractionated heparin for antithrombin therapy in non-ST-Segment elevation acute coronary syndromes: a systematic overview." JAMA 292: 89-96, 2004 Jul 7. CONTEXT: Antithrombin therapy has become a guidelines-recommended standard of care in the treatment of acute coronary syndromes (ACS), but recent trials comparing use of enoxaparin and unfractionated heparin in ACS have yielded less robust efficacy and safety results than have earlier trials of these antithrombin therapies. OBJECTIVE: To systematically evaluate the end points of all-cause death and nonfatal 0666d73c299e1a1df1b16f7db322595f.doc Page 40 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
myocardial infarction (MI), transfusion, and major bleeding observed in the 6 randomized controlled trials comparing enoxaparin and unfractionated heparin in treatment of ACS. DATA SOURCES: The primary data sets for ESSENCE, A to Z, and SYNERGY were available at the Duke Clinical Research Institute. Baseline characteristics and event frequencies for TIMI 11B, ACUTE II, and INTERACT were provided by the principal investigator of each study. STUDY SELECTION: All 6 randomized controlled trials comparing enoxaparin and unfractionated heparin in non-ST-segment elevation ACS were selected for analysis. DATA EXTRACTION: Efficacy and safety end points were extracted from the overall trial populations and the subpopulation receiving no antithrombin therapy prior to randomization. DATA SYNTHESIS: Systematic evaluation of the outcomes for 21 946 patients was performed using a random-effects empirical Bayes model. No significant difference was found in death at 30 days for enoxaparin vs unfractionated heparin (3.0% vs 3.0%; odds ratio [OR], 1.00; 95% confidence interval [CI], 0.85-1.17). A statistically significant reduction in the combined end point of death or nonfatal MI at 30 days was observed for enoxaparin vs unfractionated heparin in the overall trial populations (10.1% vs 11.0%; OR, 0.91; 95% CI, 0.83-0.99; number needed to treat, 107). A statistically significant reduction in the combined end point of death or MI at 30 days was also observed for enoxaparin in the populations receiving no prerandomization antithrombin therapy (8.0% vs 9.4%; OR, 0.81; 95% CI, 0.70-0.94; number needed to treat, 72). No significant difference was found in blood transfusion (OR, 1.01; 95% CI, 0.89-1.14) or major bleeding (OR, 1.04; 95% CI, 0.83-1.30) at 7 days after randomization in the overall safety population or in the population of patients receiving no prerandomization antithrombin therapy. CONCLUSION: In a systematic overview of approximately 22 000 patients across the spectrum of ACS, enoxaparin is more effective than unfractionated heparin in preventing the combined end point of death or MI. [References: 24]
Systematic review with meta-analysis of the data from 6 RCTs comparing the LMWH Enoxaparin to UFH in patients with ACS. Comparison of overall population and population receiving no prerandomisation antithrombin therapy. End points: All-cause death and the combined end point of death and nonfatal MI (efficacy) at 30 days, transfusion, and major bleeding (safety) at 7 days. N=21946. Level of Evidence: 1 Quality of Evidence: Excellent design and methods Direction of Evidence: Supportive in terms of efficacy of LMWH (Enoxaparin) compared to UFH in ACS, neutral in terms of safety. Ross 2001 Ross, A. M., P. Molhoek, et al. (2001). "Randomized comparison of enoxaparin, a low- molecular-weight heparin, with unfractionated heparin adjunctive to recombinant tissue plasminogen activator thrombolysis and aspirin: Second Trial of Heparin and Aspirin Reperfusion Therapy (HART II)." Circulation 104(6): 648-652. Background - Adjunctive unfractionated heparin (UFH) during thrombolytic therapy for acute myocardial infarction (AMI) promotes the speed and magnitude of coronary artery recanalization and reduces reocclusion. Low-molecular-weight heparins offer practical and potential pharmacological advantages over UFH in multiple applications but have not been systematically studied as adjuncts to fibrinolysis in AMI. Methods and Results - Four hundred patients undergoing reperfusion therapy with an accelerated recombinant tissue plasminogen activator regimen and aspirin for AMI were randomly assigned to receive adjunctive therapy for at least 3 days with either enoxaparin or UFH. The study was designed to show noninferiority of enoxaparin versus UFH with regard to infarct-related artery patency. Ninety minutes after starting therapy, patency rates (thrombolysis in myocardial infarction [TIMI] flow grade 2 or 3) were 80.1% and 75.1% in the enoxaparin and UFH groups, respectively. Reocclusion at 5 to 7 days from TIMI grade 2 or 3 to TIMI 0 or 1 flow and TIMI grade 3 to TIMI 0 or 1 flow, respectively, occurred in 5.9% and 3.1% of the enoxaparin group versus 9.8% and 9.1% in the UFH group. Adverse events occurred with similar frequency in both treatment groups. Conclusions - Enoxaparin was at least as effective as UFH as an adjunct to thrombolysis, with a trend toward higher recanalization rates and less reocclusion at 5 to 7 days.
Prospective, randomised, non-blinded trial comparing LMWH (enoxaparin) to UFH as adjunctive therapy in patients with STEMI, treated with rt-PA and aspirin. 0666d73c299e1a1df1b16f7db322595f.doc Page 41 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Level of Evidence: 2 Quality of Evidence: Good Direction of Evidence: Neutral. (Trend towards supportive) Spinler 2003 Spinler, S. A., S. M. Inverso, et al. (2003). "Safety and efficacy of unfractionated heparin versus enoxaparin in patients who are obese and patients with severe renal impairment: Analysis from the ESSENCE and TIMI 11b studies." American Heart Journal 146(1): 33- 41. Background: The advantages of enoxaparin over unfractionated heparin (UFH) for the treatment of patients with non-ST-segment elevation acute coronary syndromes are well established. However, no data are available about the safety and efficacy in patients who are obese and patients with severe renal impairment. Methods: A retrospective analysis of treatment effects was performed on patients who were obese and patients with severe renal impairment from the Efficacy Safety Subcutaneous Enoxaparin in Non-Q- wave Coronary Events (ESSENCE) and Thrombolysis in Myocardial Infarction (TIMI) 11B trials, in which patients were treated with enoxaparin or UFH. The primary composite end point was death, myocardial infarction (MI), and urgent revascularization (UR), and the secondary end points were major and any hemorrhage. Results: When compared with UFH, enoxaparin reduced the rate of the primary end point in patients who were obese (14.3% vs 18.0%, P = .05), patients who were not obese (16.1% vs 19.2%, P <.01), and patients without severe renal impairment (15.7% vs 18.4%, P <.01). There was no significant difference in major bleeding between enoxaparin and UFH in any of the 4 subgroups. There were no differences in either the primary end point (17.6% vs 16.2%, P = .39) or major hemorrhage (1.3% vs 0.8%, P = .12) in patients who were obese receiving either UFH or enoxaparin compared with patients who were not obese. Patients with severe renal impairment tended toward a higher rate of the primary end point (25.9% vs 17%, P = .09) and experienced more major hemorrhages (6.6% vs 1.1%, P <.0001). Conclusions: Enoxaparin reduced the rate of the combined end point of death/MI/UR in the subgroups of patients who were obese, patients who were not obese, and patients without renal insufficiency. Obesity did not impact clinical outcomes in the combined analysis of ESSENCE and TIMI 11B. Patients with severe renal impairment have a higher risk of clinical events and major and any hemorrhages than patients without severe renal impairment, whether they are treated with UFH or enoxaparin.
Post-hoc meta-analysis from ESSENCE and TIMI 11B trials in subgroup of patients who were obese or who had renal impairment. End points as in abstract. Renal impairment group very small, study not powered to show a difference in this subgroup. Mean time to first dose study drug (not clear if from randomisation or symptom onset) 10 – 11.4 hours. Level of Evidence: 7 Quality of Evidence: Fair Direction of Evidence: Supportive for LMWH (Enoxaparin) compared to UFH regardless of weight.
Suvarna 1997 Suvarna Tt, P. J. A. K. R. P. M. G. P. D. B. G. M. J. (1997). "Comparison of clinical outcome of fixed-dose subcutaneous low molecular weight heparin (tinzaparin) with conventional heparin in unstable angina: a pilot study." Indian Heart Journal 49(2): 159-62. Forty patients who were hospitalized for unstable angina were randomized to receive treatment with either regular heparin (Group I) in conventional dose as continuous infusion for 5 days or fixed-dose low molecular weight heparin (LMWH) (Group II), 3500 units subcutaneous twice daily for a period of 5 days. Both the groups were evenly matched with regard to age, sex presence of risk factors and adjunctive drug therapy. The clinical endpoints at the end of 5 day therapy were: recurrence of angina, occurrence of myocardial infarction and need for urgent revascularization. In Group I, 6 out of 20 patients had recurrence of angina, of whom 3 required urgent coronary angiography and revascularization. In Group II, 4 out of 20 patients had recurrence of angina, of whom one patient required urgent angiography and angioplasty. There were no bleeding complications in either of the groups. The recurrent anginal episodes in the conventional heparin group correlated with low aPTT values at the time of angina. Thus, this pilot study suggests that LMWH is equally effective in the treatment of unstable angina, the advantage of LMWH being the ease of administration and no need for monitoring aPTT levels during therapy. 0666d73c299e1a1df1b16f7db322595f.doc Page 42 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Prospective, randomised, single-blinded pilot study in patients with UA, with symptoms occurring within 24 hours of randomisation. N=40 (very small). End points at day 5 as in abstract. Study not powered to show statistically significant differences in clinical end points. Study used Tinzaparin for LMWH. Level of Evidence: 2 Quality of Evidence: Fair (? poor given study size so small) Direction of Evidence: Neutral
Theroux 2003 Theroux, P. and R. C. Welsh (2003). "Meta-analysis of randomized trials comparing enoxaparin versus unfractionated heparin as adjunctive therapy to fibrinolysis in ST- elevation acute myocardial infarction." American Journal of Cardiology 91(7): 860-864. No abstract. Meta-analysis of 6 trials: 5 trials comparing enoxaparin to UFH (ASENOX, ASSENT 3, Baird et al, ENTIRE TIMI 23, HART-2); 1 comparing enoxaparin to placebo (AMI-SK). N=6069. End- points: Death, AMI, recurrent ischaemia or angina, and their double or triple composites, early and late angiographic vessel patency, major, intracranial and minor bleeding complications. Results: The rates of AMI, recurrent ischaemia, death or AMI, and recurrent ischaemia or AMI were all significantly reduced and there was a trend toward a 14% decrease in mortality with enoxaparin. Late angiographic patency was significantly improved. However, enoxaparin had significantly more major and minor bleeding complications. Level of Evidence: 1 Quality of Evidence: Excellent Direction of Evidence: Supportive for LMWH (Enoxaparin) over UFH in terms of efficacy, and opposing in terms of safety as adjunctive therapy to fibrinolysis in patients with STEMI. Van de Werf 2001 Van de Werf, F. J., P. W. Armstrong, et al. (2001). "Efficacy and safety of tenecteplase in combination with enoxaparin, abciximab, or unfractionated heparin: The ASSENT-3 randomised trial in acute myocardial infarction." Lancet 358(9282): 605-613. Background: Current fibrinolytic therapies fail to achieve optimum reperfusion in many patients. Low-molecular-weight heparins and platelet glycoprotein IIb/IIIa inhibitors have shown the potential to improve pharmacological reperfusion therapy. We did a randomised, open-label trial to compare the efficacy and safety of tenecteplase plus enoxaparin or abciximab, with that of tenecteplase plus weight-adjusted unfractionated heparin in patients with acute myocardial infarction. Methods: 6095 patients with acute myocardial infarction of less than 6 h were randomly assigned one of three regimens: full- dose tenecteplase and enoxaparin for a maximum of 7 days (enoxaparin group; n=2040), half-dose tenecteplase with weight-adjusted low-dose unfractionated heparin and a 12-h infusion of abciximab (abciximab group; n=2017), or full-dose tenecteplase with weight- adjusted unfractionated heparin for 48 h (unfractionated heparin group; n=2038). The primary endpoints were the composites of 30-day mortality, in-hospital reinfarction, or in- hospital refractory ischaemia (efficacy endpoint), and the above endpoint plus in-hospital intracranial haemorrhage or in-hospital major bleeding complications (efficacy plus safety endpoint). Analysis was by intention to treat. Findings: There were significantly fewer efficacy endpoints in the enoxaparin and abciximab groups than in the unfractionated heparin group: 233/2037 (11.4%) versus 315/2038 (15.4%; relative risk 0.74 [95% CI 0.63- 0.87], p=0.0002) for enoxaparin, and 223/2017 (11.1%) versus 315/2038 (15.4%; 0.72 [0.61-0.84], p<0.0001) for abciximab. The same was true for the efficacy plus safety endpoint: 280/2037 (13.7%) versus 347/2036 (17.0%; 0.81 [0.70-0.93], p=0.0037) for enoxaparin, and 287/2016 (14.2%) versus 347/2036 (17.0%; 0.84 [0.72-0.96], p=0.01416) for abciximab. Interpretation: The tenecteplase plus enoxaparin or abciximab regimens studied here reduce the frequency of ischaemic complications of an acute myocardial infarction. In light of its ease of administration, tenecteplase plus enoxaparin seems to be an attractive alternative reperfusion regimen that warrants further study. Prospective, randomised, single-blinded study in patients with STEMI onset within 6 hours. No hypothesis described. N=6095. End points and results as in abstract. Level of Evidence: 1 Quality of Evidence: Good Direction of Evidence: Supportive for safety and efficacy of LMWH (enoxaparin) compared to UFH as adjunctive treatment with tenectaplase in STEMI. 0666d73c299e1a1df1b16f7db322595f.doc Page 43 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Wallentin 2003; 1 Wallentin L, B. L. D. M. F. C. G. C. B. L. B. L. L. E. N. T. P. K. S. A. S. E. (2003). "Low molecular weight heparin (dalteparin) compared to unfractionated heparin as an adjunct to rt-PA (alteplase) for improvement of coronary artery patency in acute myocardial infarction-the ASSENT Plus study." European Heart Journal 24(10): 897-908. BACKGROUND: Current thrombolytic-antithrombotic regimens in acute myocardial infarction (AMI) are limited by incomplete early coronary reperfusion and by reocclusion and reinfarction. We compared the effects of low molecular weight heparin (LMWH) versus unfractionated heparin (UFH) as an adjunct to recombinant tissue- plasminogen activator (alteplase) on coronary artery patency and clinical outcomes in AMI. METHODS: Patients with AMI treated with alteplase (n=439) were randomised to either subcutaneous dalteparin (120 IU/kg every 12h) for 4-7 days or intravenous infusion of UFH for 48 h. Coronary angiography was performed between day 4 and hospital discharge. Clinical events and safety were evaluated until day 30. RESULTS: Overall there were higher thrombolysis in myocardial infarction (TIMI) flows in the infarct related coronary artery in the dalteparin group (p=0.016). The predefined primary end-point, TIMI grade 3 flow, did not reach statistical significance (dalteparin 69.3% versus heparin 62.5%; p=0.163). However, TIMI 0-1 flow (13.4 versus 24.4%; p=0.006) and its combination with intraluminal thrombus (27.9 versus 42.0%; p=0.003) were less common in the dalteparin group. During the period of randomised treatment there were less myocardial reinfarctions in the dalteparin group(p=0.010) but after cessation of dalteparin there were more reinfarctions resulting in no difference in death or MI at 30 days. There were no significant differences in major bleeding or stroke after 30 days. CONCLUSIONS: In alteplase treated AMI adjunctive dalteparin for 4-7 days seems to reduce the risk of early coronary artery occlusion and reinfarction. However, early after cessation of treatment there is a raised risk of events, which might eliminate any long-term gains. Prospective, randomised, single-blinded trial comparing the adjunctive treatment of LMWH (Dalteparin) to UFH in patients with STEMI, onset within 6 hours, receiving fibrinolysis. N=439 Primary end point: TIMI grade 3 flow at angiography at or after day4, clinical end points were death, recurrent MI, revascularization, stroke and major hemorrhage. Level of Evidence: 2 Quality of Evidence: Good Direction of Evidence: Supportive for LMWH (dalteparin) over UFH in terms of overall TIMI flow and for early clinical efficacy end points but no difference at 30 days. Neutral in terms of safety. Wallentin 2003; 2 Wallentin L, G. P. A. P. W. G. C. B. A. A. A. A. H. R. B. K. D. T. L. B. M. M. V. (2003). "Efficacy and safety of tenecteplase in combination with the low-molecular-weight heparin enoxaparin or unfractionated heparin in the prehospital setting: the Assessment of the Safety and Efficacy of a New Thrombolytic Regimen (ASSENT)-3 PLUS randomized trial in acute myocardial infarction." Circulation 108(2): 135-42. BACKGROUND: The combination of a single-bolus fibrinolytic and a low- molecular-weight heparin may facilitate prehospital reperfusion and further improve clinical outcome in patients with ST-elevation myocardial infarction. METHODS AND RESULTS: In the prehospital setting, 1639 patients with ST-elevation myocardial infarction were randomly assigned to treatment with tenecteplase and either (1) intravenous bolus of 30 mg enoxaparin (ENOX) followed by 1 mg/kg subcutaneously BID for a maximum of 7 days or (2) weight-adjusted unfractionated heparin (UFH) for 48 hours. The median treatment delay was 115 minutes after symptom onset (53% within 2 hours). ENOX tended to reduce the composite of 30-day mortality or in-hospital reinfarction, or in-hospital refractory ischemia to 14.2% versus 17.4% for UFH (P=0.080), although there was no difference for this composite end point plus in-hospital intracranial hemorrhage or major bleeding (18.3% versus 20.3%, P=0.30). Correspondingly, there were reductions in in- hospital reinfarction (3.5% versus 5.8%, P=0.028) and refractory ischemia (4.4% versus 6.5%, P=0.067) but increases in total stroke (2.9% versus 1.3%, P=0.026) and intracranial hemorrhage (2.20% versus 0.97%, P=0.047). The increase in intracranial hemorrhage was seen in patients >75 years of age. CONCLUSIONS: Prehospital fibrinolysis allows 53% of patients to receive reperfusion treatment within 2 hours after symptom onset. The combination of tenecteplase with ENOX reduces early ischemic events, but lower doses of ENOX need to be tested in elderly patients. At present, therefore, tenecteplase and UFH are recommended as the routine pharmacological reperfusion treatment in the prehospital setting. Prospective, randomised, single-blinded trial of patients with STEMI, done in prehospital setting, 0666d73c299e1a1df1b16f7db322595f.doc Page 44 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
comparing the adjunctive treatment of LMWH (enoxaparin) to UFH in combination with prehospital fibrinolysis. N=1639. End points: composite of death, recurrent MI, recurrent ischaemia, and composite of above plus ICH or major hemorrhage. Level of Evidence: 2 Quality of Evidence: Excellent. Direction of Evidence: Supportive for feasibility of LMWH (enoxaparin) over UFH in prehospital setting. Supportive for efficacy (reinfarction). Opposing for safety in the elderly (>75 years). Zhang 2004 Zhang, Y., X. K. Wang, et al. (2004). "[Use of unfractionated heparin and a low-molecular- weight heparin following thrombolytic therapy for acute ST-segment elevation myocardial infarction]." Di Yi Jun Yi Da Xue Xue Bao 24(1): 81-4. OBJECTIVE: To compare the efficacy and safety of unfractionated heparin with a low-molecular-weight heparin (parnaparin) in the management of anticoagulation following thrombolytic therapy for acute ST-segment elevation myocardial infarction. METHODS: One hundred and eighty-six patients with acute ST-segment elevation myocardial infarction undergoing thrombolytic therapy were randomly assigned to receive either unfractionated heparin (100 U/kg x b.w. intravenous bolus, 1,000 U/h continuous infusion for 3 days just 12 h after thrombolysis to maintain the activated partial thromboplastin time at 1.5 to 2.0 times as normal, then subcutaneous 7500 U every 12 h for 4 days, n=90) or parnaparin (0.4 ml subcutaneously every 12 h for 7 days 12 h after thrombolysis, n=96) in conjunction with routine therapy. The patients enrolled stayed in hospital for at least 14 days and were followed for 45 days after admission into the hospital. RESULTS: The composite triple end-point (death, recurrent myocardial infarction, emergency revascularization assessed at 2, 7, 14, 45 days) was significantly reduced in patients receiving parnaparin 42.22% vs 37.08%, P=0.03 . Compared with unfractionated heparin group, the incidences of hemorrhage 10.00% vs 3.13%, P=0.06 and heparin-induced thrombocytopenia (3.33% vs 0, P=0.07) were also lower in parnaparin group. CONCLUSION: Parnaprin is more effective in reducing composite cardiac events, hemorrhage and heparin-induced thrombocytopenia at least in 45 days as compared with unfractionated heparin during anticoagulation following thrombolytic therapy for acute ST- segment elevation myocardial infarction.
Full text in Chinese, unavailable electronically or via AHA. Randomised single-blinded controlled trial of patients with STEMI receiving fibrinolysis. Level of Evidence: 2 Quality of Evidence: Unable to determine from abstract. Direction of Evidence: Supportive *Type the citation marker in the first field and then paste the full citation into the second field. You can copy the full citation from EndNote by selecting the citation, then copying the FORMATTED citation using the short cut, Ctrl-K. After you copy the citation, go back to this document and position the cursor in the field, then paste the citation into the document (use Ctrl-V). For each new citation press Tab to move down to start a new field.
Excluded references (187 with notes) 0666d73c299e1a1df1b16f7db322595f.doc Page 45 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Ageno, W. and M. V. Huisman (2001). "Arterial indications for the low molecular weight heparins." Current Controlled Trials in Cardiovascular Medicine 2(5): 233-239. Review Article only.
Ageno, W. and A. G. G. Turpie (2000). "Therapy of unstable angina with the low molecular weight heparins." Vascular Medicine 5(4): 217-223. Review Article only.
Ageno, W. and A. G. G. Turpie (2002). "Low molecular weight heparins in the treatment of unstable angina." Minerva Cardioangiologica 50(6): 643-651 Review Article only.
Agnelli, G. and F. Sonaglia (2002). "Perspectives on antithrombotic agents: From unfractionated heparin to new antithrombotics." Haematologica 87(7): 757-770. Review Article only.
Ahrens, J. (1998). "Advantages of enoxaparin (Clexane(TM)) in comparison with unfractionated heparin in unstable angina pectoris. [German]." Therapiewoche Schweiz 14(5-6): 228-230. No abstract available.
Almeda, F. Q., R. C. Hendel, et al. (2003). "Improved in-hospital outcomes in acute coronary syndromes (unstable angina/non- ST segment elevation myocardial infarction) despite similar TIMI risk scores." Journal of Invasive Cardiology 15(9): 502-506. In-hospital trial.
Altman, R. (1998). "Controversies in antithrombotic therapy in cardiovascular diseases." Clinical & Applied Thrombosis/Hemostasis 4(1): 11-24 Review Article only.
Anonymous (1997). "Combined anticoagulant and antiplatelet therapy required for unstable angina." Prescrire International 6(29): 80-82. Review Article only.
Anonymous (2004). "Enoxaparin clinically equivalent to UFH in the treatment of high-risk ACS." Formulary 39(5). Note in a formulary only.
Antman, E. M. (1998). "TIMI 11B. Enoxaparin versus unfractionated heparin for unstable angina or non-Q-wave myocardial infarction: A double-blind, placebo-controlled, parallel-group, study design, and methods." American Heart Journal 135(6 III SUPPL): S353-S360. Design and methods part of ESSENCE Trial, no results, repeated in Antman, 1999 Circulation.
Antman, E. M. (2001). "The search for replacements for unfractionated heparin." Circulation 103(18): 2310-2314. No abstract available.
Aroney, C. (2001). "Management of the acute coronary syndromes." Australian Prescriber 24(3): 56-58 Review Article only.
Aronow, W. S. (2001). "Drug treatment of elderly patients with acute myocardial infarction: Practical recommendations." Drugs & Aging 18(11): 807-818. Review Article only
Aronow, W. S. (2003). "Management of unstable angina/non-ST-segment elevation myocardial infarction." Annals of Long Term Care 11(4): 19-23 Review Article only.
Averkov, O. V., N. N. Slavina, et al. (2003). "[Non-ST elevation acute coronary syndrome: changes of parameters of hemostasis during and after treatment with unfractionated heparin and enoxaparin]." Kardiologiia 43(9): 28-40. Trial focus on haemostasis factors.
Barbash, I. M., D. Freimark, et al. (2002). "Outcome of myocardial infarction in patients treated with aspirin is enhanced by pre- hospital administration." Cardiology 98(3): 141-7. 0666d73c299e1a1df1b16f7db322595f.doc Page 46 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Main focus on Aspirin, no UFH v LMWH comparison.
Bergqvist, D. (2002). "Enoxaparin: A pharmacoeconomic review of its use in the prevention and treatment of venous thromboembolism and in acute coronary syndromes." Pharmacoeconomics 20(4): 225-243. Review Article only.
Bijsterveld, N. R., A. H. Moons, et al. (2002). "Rebound thrombin generation after heparin therapy in unstable angina: A randomized comparison between unfractionated and low-molecular-weight heparin." Journal of the American College of Cardiology 39(5): 811-817. Factor trial done in in-hospital setting. Not relevant to the PH or ED settings.
Bijsterveld, N. R., R. J. G. Peters, et al. (2003). "Recurrent cardiac ischemic events early after discontinuation of short-term heparin treatment in acute coronary syndromes. Results from the TIMI 11B and ESSENCE studies." Journal of the American College of Cardiology 42(12): 2083-9. Post hoc analysis of ESSENCE and TIMI 11B trials. Not relevant to ED/Prehospital setting.
Bonan, R. and G. Gosselin (1996). "The antithrombotic and antiplatelet therapies of tomorrow. [French]." Archives des Maladies du Coeur et des Vaisseaux Pratique. Issue 28(pp 19-21). No abstract available.
Borja, J. and P. Olivella (2002). "Enoxaparin and unfractionated heparin in acute coronary syndromes without ST-segment elevation." Thrombosis & Haemostasis 87(3). Letter to the Editor.
Bottiger, B. W., C. Bode, et al. (2001). "Efficacy and safety of thrombolytic therapy after initially unsuccessful cardiopulmonary resuscitation: a prospective clinical trial.[see comment]." Lancet 357(9268): 1583-5. Only UFH use, no comparison to LMWH. Main focus on thrombolytic therapy.
Bosanquet, N. and K. A. A. Fox (2001). "Longer term economic benefits reflect improved clinical outcomes with enoxaparin versus unfractionated heparin in acute coronary syndromes: One-year data." British Journal of Cardiology 8(1): 36-37. No abstract available.
Bozovich, G. E. and E. P. Gurfinkel (1998). "Chlamydia pneumoniae: More than a bystander in acute coronary syndromes." British Journal of Cardiology 5(2): 84-90. Review article, main focus not on UFH/LMWH management.
Branzi, A., V. Cervi, et al. (1988). "Subcutaneous low-molecular weight heparin versus unfractionated heparin in acute myocardial infarction." Atherosclerosis VIII: proceedings of the 8th International Symposium on Atherosclerosis. ICS817. Conference: The 8th International Symposium on Atherosclerosis 09(13): 443-445. No abstract available. Conference paper.
Breddin, H. K. (1996). "Coronary heart disease, unstable angina, PTCA: New indications for low molecular weight heparins?" Thrombosis Research 81(2 SUPPL): S47-S51. Review article only.
Breddin, H. K. (2002). "The role of antithrombin agents and factor Xa-inhibitors in antithrombotic treatment." Turkish Journal of Haematology 19(2): 113-120. Review article focusing on Hirudin.
Brewster, G. S. and M. E. Herbert (2000). "Heparin should be administered to every patient admitted to the hospital with possible unstable angina." Western Journal of Medicine 173(2): 138-140. No abstract
Brieger, D. (2004). "Optimizing adjunctive antithrombotic therapy in the treatment of acute myocardial infarction: a role for low-molecular-weight heparin." Clin Cardiol 27(1): 3-8. Review article only
Brogan, G. X., Jr. (2000). "Managing chest pain in the emergency room." European Heart Journal Supplements 2(C): C15-C21. Review article only. 0666d73c299e1a1df1b16f7db322595f.doc Page 47 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Cannon, C. P. (2000). "Elderly Patients with Acute Coronary Syndromes: Higher Risk and Greater Benefit from Antithrombotic and Interventional Therapies." Am J Geriatr Cardiol 9(5): 265-270. Review article only.
Cannon, C. P. and A. G. G. Turpie (2003). "Unstable angina and non-ST-elevation myocardial infarction: Initial antithrombotic therapy and early invasive strategy." Circulation 107(21): 2640-2645. Review article only.
Casaccia, M., F. Bertello, et al. (1996). "Prehospital management of acute myocardial infarct in an experimental metropolitan system of medical emergencies [in Italian]." G Ital Cardiol 26(6): 657-672. No use or comparison of LMWH in trial.
Cheng, J. W. M. (1153). "Pharmacotherapeutic options for the management of myocardial infarction." Expert Opinion on Pharmacotherapy 3(8): 1153-1168. Review article only.
Choo, J. K. and D. J. Kereiakes (2001). "Low molecular weight heparin therapy for percutaneous coronary intervention: A practice in evolution." Journal of Thrombosis & Thrombolysis 11(3): 235-246. Review article only.
Cohen, M., R. Blaber, et al. (1997). "The ESSENCE trial: Efficacy and safety of subcutaneous enoxaparin in unstable angina and non-Q-wave MI: A double-blind, randomized, parallel-group, multicenter study comparing enoxaparin and intravenous unfractionated heparin: Methods and design." Journal of Thrombosis & Thrombolysis 4(2): 271-274. ESSENCE(1) Prospective, double-blinded, randomised controlled trial of patients with ACS/NSTEMI within 24 hours onset of symptoms. This article describes the methods and design of ESSENCE. Preliminary results only given, no comparative outcome data. Repeated in subsequent publication.
Cohen, M., C. Demers, et al. (1998). "Low-molecular-weight heparins in non-ST-segment elevation ischemia: The ESSENCE trial." American Journal of Cardiology 82(5 B) ESSENCE Trial, same information as {Cohen, 1997} except published with odds ratios and confidence intervals.
Cohen, M. (1998). "New therapies for unstable angina and non-Q-wave myocardial infarction: Recent clinical trials." American Heart Journal 135(6 III SUPPL): S343-S352. Review article.
Cohen, M., F. Maritz, et al. (2000). "The TETAMI trial: The safety and efficacy of subcutaneous enoxaparin versus intravenous unfractionated heparin and of tirofiban versus placebo in the treatment of acute myocardial infarction for patients not thrombolyzed: Methods and design." Journal of Thrombosis & Thrombolysis 10(3): 241-246. Design and methods of TETAMI trial (Cohen 2003 reports results).
Cohen, M., S. S. Stinnett, et al. (2000). "Predictors of recurrent ischemic events and death in unstable coronary artery disease after treatment with combination antithrombotic therapy." American Heart Journal 139(6): 962-970. Post-hoc analysis of ESSENCE trial. Little mention of comparison between UFH and LMWH. No additive information that is not in original ESSENCE trial.
Cohen, M. and E. M. Antman (2002). "Enoxaparin and unfractionated heparin in acute coronary syndromes without ST-segment elevation." Thrombosis & Haemostasis 88(5): 884-886. No abstract, ?letter only.
Cohen, M., E. M. Antman, et al. (2002). "Superiority of enoxaparin over unfractionated heparin for the treatment of acute coronary syndromes." Pharmacotherapy 22(4): 542-550. Review article only.
Cohen, M., H. Arjomand, et al. (2004). "The Evolution of Thrombolytic Therapy and Adjunctive Antithrombotic Regimens in Acute ST-Segment Elevation Myocardial Infarction." American Journal of Emergency Medicine 22(1): 14-23. Systematic Review article, does not include a meta-analysis.
David Talley, J. (1999). "Medical management of acute coronary syndromes." Journal of Interventional Cardiology 12(1): 33-49. Review article only. 0666d73c299e1a1df1b16f7db322595f.doc Page 48 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Davis, R. and D. Faulds (1997). "Nadroparin calcium. A review of its pharmacology and clinical use in the prevention and treatment of thromboembolic disorders." Drugs & Aging 10(4): 299-322. Review article only.
Di Chiara, A., F. Chiarella, et al. (2003). "Epidemiology of acute myocardial infarction in the Italian CCU network: the BLITZ study.[see comment]." European Heart Journal 24(18): 1616-29. No comparison of LMWH to UFH, only epidemiological data.
Dudek, D., S. Bartus, et al. (2001). "Combined use of platelet glycoprotein IIb/IIIa receptor blocker and thrombolysis in acute myocardial infarction avoided the necessity for primary angioplasty - A case report." Kardiologia Polska 55(10): 325-328. Case report, combination therapy included LMWH, no comparison to UFH.
Dunn, C. J. and B. Jarvis (2000). "Dalteparin: An update of its pharmacological properties and clinical efficacy in the prophylaxis and treatment of thromboembolic disease." Drugs 60(1): 203-237. Review article only.
Dunn, C. J., E. M. Sorkin, et al. (1996). "Dalteparin sodium. A review of its pharmacology and clinical use in the prevention and treatment of thromboembolic disorders." Drugs 52(2): 276-305. Review article only.
Eikelboom, J. W. and G. J. Hankey (2002). "Low molecular weight heparins and heparinoids." Medical Journal of Australia 177(7): 379-383. Review article only.
Fareed, J., D. Hoppensteadt, et al. (2004). "Biochemical and pharmacologic heterogeneity in low molecular weight heparins. Impact on the therapeutic profile." Current Pharmaceutical Design 10(9): 983-999. Review of LMWH only.
Fareed, J., D. A. Hoppensteadt, et al. (2003). "Management of thrombotic and cardiovascular disorders in the new millenium." Clinical & Applied Thrombosis/Hemostasis 9(2): 101-108. Review article only.
Faxon, D. P., T. E. Spiro, et al. (1994). "Low molecular weight heparin in prevention of restenosis after angioplasty: Results of Enoxaparin restenosis (ERA) trial." Circulation 90(2): 908-914. Trial post angioplasty, not relevant to prehospital/ED setting.
Federman, J. (2003). "Unstable angina assessment and management." Medicine Today 4(1): 37-45. Review article only.
Ferguson, I. J. (1997). "New pharmacological adjuncts for coronary stenting: Can new anticoagulants improve outcomes?" Journal of Interventional Cardiology 10(2): 155-159. Review article only.
Ferguson, J. J. (2002). "Low molecular weight heparins and glycoprotein IIb/IIIa antagonists." Journal of Interventional Cardiology 15(2): 147-154. Review article only.
Ferrario, M., P. A. Merlini, et al. (1999). "Antithrombotic therapy of unstable angina and non-Q-wave myocardial infarction." International Journal of Cardiology 68(Suppl 1): S63-71. Review article only.
Ferreira, D. (1005). "Pharmacological reperfusion in acute myocardial infarction after ASSENT 3 and GUSTO V." Revista Portuguesa de Cardiologia 22(7-8): 1005-1009. Guideline which has main focus on PCI and thrombolysis rather than LMWH and UFH.
Fitchett, D., S. G. Goodman, et al. (1179). "Preventing thrombosis: Update of first-line therapy in the management of non-ST segment elevation acute coronary syndromes." Canadian Journal of Cardiology 18(11): 1179-1190. Review article only. 0666d73c299e1a1df1b16f7db322595f.doc Page 49 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Fox, K. A. A. (2001). "Antithrombotic therapy in acute coronary syndromes: Key notes from ESSENCE and TIMI 11B." Seminars in Hematology 38(2 SUPPL. 5): 67-74. Review article only.
Fox, K. A. A. and N. Bosanquet (1998). "Assessing the UK cost implications of the use of low molecular weight heparin in unstable coronary artery disease." British Journal of Cardiology 5(2): 92-105. Post-hoc analysis of cost of LMWH, full text unavailable.
Gaede, A. and W. Terres (1999). "Therapy of the acute coronary syndrome. ASA, heparin, LMWH, hirudin and the GP-IIb/IIIa blockers. [German]." Herz 24(5): 353-362. Review in German.
Gerrah, R., S. Tshori, et al. (2004). "Pericardial fluid and serum VEGF in response to different types of heparin treatment." International Journal of Cardiology 94(2-3): 193-196. In-hospital trial of peri-operative group of patients undergoing CABG. Not relevant to prehospital/ED setting. No clinical outcome data, measurement of serum vascular endothelial growth factor but unsure if results clinically beneficial or detrimental.
Ghali, W. A., A. Pannatier, et al. (2002). "Transition from unfractionated heparin to low molecular weight heparins." Thrombosis & Haemostasis 88(3): 539-540. Letter only.
Giangrande, P. L. F. (2002). "Fondaparinux (Arixtra): A new anticoagulant." International Journal of Clinical Practice 56(8): 615-617. Review article focuses on a pentasaccharide factor Xa inhibitor.
Goldstein, P., N. Assez, et al. (2003). "Prehospital reperfusion strategies to optimize outcomes in acute myocardial infarction." Jeur 16(3): 132-141. Review article only, emphasis on thrombolysis not UFH v LMWH.
Gonzalez, E. R., L. A. Jones, et al. (1992). "Adjunctive medications in patients receiving thrombolytic therapy: a multicenter prospective assessment. The Virginia Multicenter Thrombolytic Study Group." Ann Pharmacother 26(11): 1383-1384. No comparison with LMWH.
Gonzalez, E. R. (1999). "Low-molecular-weight heparins for acute coronary syndromes: An emergency medicine perspective." Pharmacotherapy 19(9). Review article only.
Gonzalez Pacheco, H. (2001). "[Non-fractionated heparin versus low molecular weight heparin in acute coronary syndromes]." Archivos de Cardiologia de Mexico 71(Suppl 1): S63-8. Review article only.
Goodman, S. G. (2000). "Low-molecular-weight heparin in patients with non-ST-segment elevation acute coronary syndrome: Role in the emergency department." Journal of Emergency Medicine 19(3 SUPPL). Review article only.
Graf, J. and U. Janssens (2004). "Low-molecular weight heparins in percutaneous coronary interventions: Current concepts, problems, and perspectives." Current Pharmaceutical Design 10(4): 375-386. Review article only.
Gratsianskii, N. A. (2003). "[Enoxaparin failed to show superiority to unfractionated heparin in patients with non ST-elevation acute coronary syndrome in a phase of A to Z trial]." Kardiologiia 43(6): 70-1. Russian, no abstract available.
Grines, C. L., K. F. Browne, et al. (1993). "A comparison of immediate angioplasty with thrombolytic therapy for acute myocardial infarction. The Primary Angioplasty in Myocardial Infarction Study Group." N Engl J Med 328(10): 673-679. No use of LMWH.
Gulba, D. (1999). "Differentiation of low molecular weight heparins in acute coronary syndromes: An interventionalist's perspective." Seminars in Thrombosis & Hemostasis 25(4 SUPPL. 3): 123-127. Review article only. 0666d73c299e1a1df1b16f7db322595f.doc Page 50 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Gurfinkel, E. (1998). "Current treatment and future prospects for the management of acute coronary syndromes." Clinical Drug Investigation 15(5): 367-380. Review article only.
Gurfinkel, E., J. Fareed, et al. (1998). "Rationale for the management of coronary syndromes with low-molecular- weight heparins." American Journal of Cardiology 82(5 B). Review article only.
Gurfinkel E, D. E. C. C. B. G. C. M. M. B. (1999). "Thrombotic reactant markers in non-ST segment elevation acute coronary syndromes treated with either enoxaparin (low molecular weight heparin) or unfractionated heparin." Journal of Thrombosis & Thrombolysis 8(3): 227-32. Trial focuses on anti-Xa activity and other thrombotic markers.
Haas, S. (1999). "Low molecular weight heparins in the prevention of venous thromboembolism in nonsurgical patients." Seminars in Thrombosis & Hemostasis 25(4 SUPPL. 3): 101-105. Review article focuses on venous thromboembolism, not ACS/MI.
Haas, S. (2003). "The present and future of heparin, low molecular weight heparins, pentasaccharide, and hirudin for venous thromboembolism and acute coronary syndromes." Seminars in Vascular Medicine 3(2): 139-146. Review article focuses on pentasaccharides and hirudin.
Habis, M. and M. C. Morice (1998). "Review of clinical trials of antithrombotics in unstable angina. [French]." Annales de Cardiologie et d Angeiologie 47(1): 22-31. Review article only.
Hahn, S., I. K. Jang, et al. (1999). "Antithrombotic therapy for acute coronary syndromes, Part 2: UA, NSTE- MI." Journal of Critical Illness 14(1): 42-50. Review article only.
Hamm, C. W. (1998). "Progress in the diagnosis of unstable angina and perspectives for treatment." Eur Heart J 19 Suppl N: N48-50. General review article only. No comparison LMWH to UFH.
Hayes, O. W. (1998). "Emergency management of acute myocardial infarction: focus on pharmacologic therapy." Emerg Med Clin North Am 16(3): 541-563. Review article only.
Herren, K. R. and K. Mackway-Jones (2001). "Emergency management of cardiac chest pain: a review." Emerg Med J 18(1): 6- 10. Review article only.
Hirsh, J. (1997). "Low-molecular-weight heparin should replace unfractionated heparin for treatment of venous thrombosis and unstable angina." Journal of Thrombosis & Thrombolysis 4(3-4): 349-351. No abstract available.
Hirsh, J. and S. M. Bates (2000). "The emerging role of low-molecular-weight heparin in cardiovascular medicine." Progress in Cardiovascular Diseases 42(4): 235-246. Review article only.
Hlatky, M. A. (1998). "Enoxaparin had lower costs than unfractionated heparin for acute coronary syndrome." Evidence Based Medicine 3(6). No abstract available.
Hoekstra, J. W., C. V. Pollack Jr, et al. (2002). "Improving the care of patients with non-ST-elevation acute coronary syndromes in the emergency department: The CRUSADE initiative." Academic Emergency Medicine 9(11): 1146-1155. No information on UFH verses LMWH.
Holdright, D. R. (2001). "Dalteparin sodium (Fragmin) in the management of acute coronary syndromes." British Journal of Cardiology 8(3). 0666d73c299e1a1df1b16f7db322595f.doc Page 51 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Review article only.
Holper, E. M., E. M. Antman, et al. (1008). "A simple, readily available method for risk stratification of patients with unstable angina and non-ST elevation myocardial infarction." American Journal of Cardiology 87(8): 1008-1010. No UFH/LMWH comparison
Hovanessian, H. C. (1999). "New-generation anticoagulants: the low molecular weight heparins." Ann Emerg Med 34(6): 768- 79. Review article only.
Ibbotson, T. and K. L. Goa (1407). "Enoxaparin: An update of its clinical use in the management of acute coronary syndromes." Drugs 62(9): 1407-1431 Review article only.
Iqbal, O., M. Tobu, et al. (2002). "The role of thrombolytic drugs in the management of acute myocardial infarction and stroke." Turkish Journal of Haematology 19(2): 151-177. No abstract.
Jafri, S. M. (2000). "Unfractionated heparin is the heparin of choice in the management of patients with acute coronary syndromes." Journal of Thrombosis & Thrombolysis 9(2): 145-147 No abstract available.
Julian, D. and W. B. Saunders (1996). "Acute myocardial infarction: Pre-hospital and in-hospital management." European Heart Journal 17(1): 43-63. No abstract.
Karpov, R. S., V. A. Markov, et al. (1992). "Effectiveness of pre-hospital thrombolytic therapy in acute myocardial infarction [in Russsian]." Kardiologiia 32(9-10): 23-26. No comparison with LMWH.
Karsch, K. R., M. B. Preisack, et al. (1996). "Low molecular weight heparin (reviparin) in percutaneous transluminal coronary angioplasty. Results of a randomized, double-blind, unfractionated heparin and placebo-controlled, multicenter trial (REDUCE trial)." Journal of the American College of Cardiology 28(6): 1437-1443. In-hospital trial during and post PTCA. Exclusion criteria contained ACS requiring treatment with heparin infusion prior to PTCA.
Kaul, S. and P. K. Shah (1699). "Low molecular weight heparin in acute coronary syndrome: Evidence for superior or equivalent efficacy compared with unfractionated heparin?" Journal of the American College of Cardiology 35(7): 1699-1712. Systematic Review article only.
Kauw, F. H. W., T. J. M. Cleophas, et al. (1998). "Low molecular weight heparins better than unfractionated heparin in unstable coronary artery disease? Unstable angina pectoris/non-Q wave infarction a partly outpatient clinic condition?" International Journal of Clinical Pharmacology & Therapeutics 36(7): 392-397. Review article only. Also focus on long term outpatient care.
Keller, N. M. and F. Feit (1998). "Thrombolytic therapy in acute MI, part 2: Update on adjuvants." Journal of Critical Illness 13(10): 646-652. Review article only.
Kereiakes, D. J. (2000). "Debate: Unstable angina - When should we intervene?" Current Controlled Trials in Cardiovascular Medicine 1(1): 9-14. Review article only.
Kher, A., M. Samama, et al. (1991). "[Heparin in the treatment and secondary prevention of myocardial infarction. A critical review of the main trials]." Archives des Maladies du Coeur et des Vaisseaux 84(11): 1581-6. Review article only. Full text in French.
Kher, A. and M. M. Samama (1495). "Low molecular weight heparin in unstable angina. [French]." Archives des Maladies du Coeur et des Vaisseaux 89(11 SUPPL): 1495-1500. Review article only. Full text in French. 0666d73c299e1a1df1b16f7db322595f.doc Page 52 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Klein, W., A. Buchwald, et al. (1997). "Battle of the heparins: LMWH v unfractionated heparin in unstable CAD." Journal of Critical Illness 12(12). No abstract available. ?note
Klein, W., A. Buchwald, et al. (1997). "Fragmin in unstable angina pectoris or in non-Q-wave acute myocardial infarction: Fragmin in Unstable Coronary Artery Disease study (FRIC)." Am J Cardiol 80(5A): 30E-34E. FRIC trail – Prospective, randomised trial of patients with UA/NSTEMI symptoms in the preceding 72 hours. Trial published again in Circulation in same year with results of 10 more patients and including odds ratios and confidence intervals (Klein, 1997).
Knight, C. J., M. Panesar, et al. (1998). "Increased platelet responsiveness following coronary stenting. Heparin as a possible aetiological factor in stent thrombosis." European Heart Journal 19(8): 1239-48. In-hospital trial looking at in stent thrombosis, post PTCA.
Lewandowski, K., W. Elikowski, et al. (1996). "Low molecular weight heparin and the heparin mobilisable pool of platelet factor 4 are reduced in young survivors of myocardial infarction." Thrombosis Research 81(6): 615-22. Not relevant to topic, study looks at factor levels.
Li, Y. F., M. Rodriguez, et al. (2002). "Comparative effects of unfractionated heparin and low molecular weight heparin on vascular endothelial cell tissue factor pathway inhibitor release: A model for assessing intrinsic thromboresistance." Journal of Thrombosis & Thrombolysis 14(2): 123-129. Not relevant to topic, in vitro study looks at effects of UFH and LMWH on thrombogenic factors.
Lindahl, B., P. Venge, et al. (1997). "Troponin T identifies patients with unstable coronary artery disease who benefit from long- term antithrombotic protection. Fragmin in Unstable Coronary Artery Disease (FRISC) Study Group." J Am Coll Cardiol 29(1): 43-48. Study looks at long term treatment with LMWH. No comparison to UFH.
Lopez Bescos, L., F. Aros Borau, et al. (2002). "2002 update of the guidelines of the Spanish Society of Cardiology for Unstable Angina/without ST-segment elevation myocardial infarction." Revista Espanola de Cardiologia 55(6): 631-642. Systematic Review.
Lopez-Sendon, J., E. Lopez de Sa, et al. (1999). "The importance of thrombin and its inhibition in unstable angina. Non fractionated heparin, hirudin and fractionated heparin. [Spanish]." Revista Espanola de Cardiologia 52(SUPPL. 1): 76-89. Review article only.
Mahaffey, K. W. (2002). "The SYNERGY trial: Study design and rationale." American Heart Journal 143(6): 952-960. Study design and rationale description only.
Marmur, J. D., S. X. Anand, et al. (2003). "The activated clotting time can be used to monitor the low molecular weight heparin dalteparin after intravenous administration." Journal of the American College of Cardiology 41(3): 394-402. Trial of intravenous LMWH during PCI. Not relevant to ED or prehospital.
Matheson, A. J. and K. L. Goa (2000). "Desirudin: A review of its use in the management of thrombotic disorders." Drugs 60(3): 679-700. Review article on Desirudin.
McKay, G. A. and K. R. Paterson (2001). "Low molecular weight heparins - A safer option than unfractionated heparin?" Adverse Drug Reactions & Toxicological Reviews 20(4): 256-276. Review article.
Melandri G, B. A. S. F. C. V. M. B. (1992). "Effects of two dosages of subcutaneous low molecular weight heparin (Parnaparin) and of unfractionated heparin on fibrin formation and lipolysis in acute myocardial infarction." Thrombosis Research 66(2-3): 141-50. Trial of subcutaneous heparin versus LMWH in AMI to prevent venous and arterial thromboembolism. Looks at in vivo thrombotic factor differences.
Menon, V., S. D. Berkowitz, et al. (2001). "New heparin dosing recommendations for patients with acute coronary syndromes.” American Journal of Medicine 110(8): 641-650. 0666d73c299e1a1df1b16f7db322595f.doc Page 53 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Review article.
Montalescot, G., J. P. Collet, et al. (2000). "Effects of various anticoagulant treatments on von Willebrand factor release in unstable angina." Journal of the American College of Cardiology 36(1): 110-114. Study looks at effects of 2 different LMWHs, UFH and Hirudin on vWf release over 48 hours, not relevant to Emergency setting.
Moreadith, R. W. and D. Collen (1337). "Clinical development of PEGylated recombinant staphylokinase (PEG-Sak) for bolus thrombolytic treatment of patients with acute myocardial infarction." Advanced Drug Delivery Reviews 55(10): 1337-1345. Review of a thrombolytic agent, no comparison UFH and LMWH.
Moser, LR and Kalus, JS (2004). “Role of Low Molecular-Weight Heparin in invasive management of Non-ST-Elevation Acute Coronary Syndromes.” The Annals of Pharmacotherapy 38: 2094-104 Review of LMWH in PCI. No comparative data documented.
Nenci, G. G. and A. Minciotti (2000). "Low molecular weight heparins for arterial thrombosis." Vascular Medicine 5(4): 251- 258. Review article only.
Nesvold, A., F. Kontny, et al. (1991). "Safety of high doses of low molecular weight heparin (Fragmin) in acute myocardial infarction. A dose-finding study." Thrombosis Research 64(5): 579-587. No comparison with UFH.
Nguyen, P., M. G. Remy, et al. (1999). "Comparative inhibition of LPS-activated human monocyte-induced thrombin generation by unfractionated heparin and low molecular weight heparins." Haemostasis 29(6): 301-309. In vitro study looks at effects of UFH and LMWH on monocyte induced thrombin generation.
Nguyen-Ho, P. and G. N. Levine (2002). "The role of low-molecular-weight heparins in non-ST-segment elevation acute coronary syndromes." Panminerva Medica 44(2): 115-22. Review article only.
Nicolaides, A. N. (2002). "Clinical results with direct thrombin inhibitors." Pathophysiology of Haemostasis & Thrombosis 32(SUPPL. 3): 36-38. Review article on Hirudin.
Nilsen, D. W. T., L. Goransson, et al. (1997). "Systemic thrombin generation and activity resistant to low molecular weight heparin administered prior to streptokinase in patients with acute myocardial infarction." Thrombosis & Haemostasis 77(1): 57- 61. Comparison of UFH and LMWH on systemic Factor Xa and thrombin activity.
Nurmohamed, M. T., H. Ten Cate, et al. (1997). "Low molecular weight heparin(oid)s. Clinical investigations and practical recommendations." Drugs 53(5): 736-751. Drug review article, little on ACS/MI.
O'Connor, R., D. Persse, et al. (2001). "Acute coronary syndrome: Pharmacotherapy." Prehospital Emergency Care 5(1): 58-64. Review article by prehospital consensus group.
Olariu, C. T. and L. Olariu (2001). "Current therapeutic options in unstable angina." Journal of Clinical & Basic Cardiology 4(4): 269-274. General review article only.
O'Neill, W. W., R. Weintraub, et al. (1992). "A prospective, placebo-controlled, randomized trial of intravenous streptokinase and angioplasty versus lone angioplasty therapy of acute myocardial infarction." Circulation 86(6): 1710-1717. No LMWH.
Ornato, J. P. (1473). "Acute coronary syndromes: What role for LMWH and other cardiac drugs?" Consultant 42(12): 1473- 1480. General review article only. 0666d73c299e1a1df1b16f7db322595f.doc Page 54 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Otterstad, J. E. and F. Brosstad (2003). "Results from clinical trials on ST-elevation myocardial infarction in a historic perspective with some pathophysiological aspects." Scandinavian Cardiovascular Journal 37(6): 316-323. Review article.
Pacheco, H. G. (2001). "Unfractionated heparin vs low molecular weight heparin in acute coronary syndromes. [Spanish]." Archivos de Cardiologia de Mexico 71(SUPPL. 1): S63-S68. Review article only.
Parchure, N. and S. J. D. Brecker (2002). "Management of acute coronary syndromes." Current Opinion in Critical Care 8(3): 230-235 Review article only.
Pollack, C. V., Jr. and W. B. Gibler (2001). "2000 ACC/AHA guidelines for the management of patients with unstable angina and non-ST-segment elevation myocardial infarction: A practical summary for emergency physicians." Annals of Emergency Medicine 38(3): 229-240. Review, and superseded by same author in similar guidelines published in 2003. {Pollack Jr, 2003}
Pollack, C. V., Jr. and W. B. Gibler (2001). "Advances create opportunities: Implementing the major tenets of the new unstable angina guidelines in the emergency department." Annals of Emergency Medicine 38(3): 241-248. Review, but does have a statement about using LMWH in ED, as soon as diagnosis of ACS is considered possible, rather than waiting until admission to CCU. Level 8 (Expert opinion).
Preisack, M. B., R. Bonan, et al. (1998). "Incidence, outcome and prediction of early clinical events following percutaneous transluminal coronary angioplasty. A comparison between treatment with reviparin and unfractionated heparin/placebo (results of a substudy of the REDUCE trial)." European Heart Journal 19(8): 1232-8. Intravenous LMWH at time of PTCA, not relevant to PH/ED setting.
Redwood, S., M. Marber, et al. (1999). "Glycoprotein IIB/IIIA antagonists: Do they have a role in the management of unstable angina?" International Journal of Clinical Practice 53(8): 618-622. Main focus on Glycoprotein 11B/111A antagonists, no comparison of UFH and LMWH.
Reeder, G. S. (2000). "Contemporary diagnosis and management of unstable angina." Mayo Clin Proc 75(9): 953-7. Review article only. No comparison LMWH to UFH.
Roberts, C. (1999). "Have we reached the therapeutic ceiling in acute myocardial infarction?" Crit Care Nurse 19(5 Suppl): 7-11. Review article only. No comparison LMWH to UFH.
Ross, A. M., K. Coyne, et al. (2000). "Low-molecular-weight heparins in acute myocardial infarction: Rationale and results of a pilot study." Clinical Cardiology 23(7): 483-485. HART II Pilot study, primary outcome was coagulation stability.
Roth, A., G. I. Barbash, et al. (1990). "Should thrombolytic therapy be administered in the mobile intensive care unit in patients with evolving myocardial infarction? A pilot study.[see comment]." Journal of the American College of Cardiology 15(5): 932- 6. Trial focuses on thrombolysis, all patients were fully heparinised, no LMWH comparison.
Ryan, T. J. and R. M. Melduni (2002). "Highlights of latest American College of Cardiology and American Heart Association Guidelines for Management of Patients with Acute Myocardial Infarction." Cardiology in Review 10(1): 35-43. Review only. No comparison UFH to LMWH.
Salam, A. M. (1567). "Low molecular weight herapins combined with platelet glycoprotein IIb/IIIa inhibitors in the management of acute coronary syndromes." Expert Opinion on Investigational Drugs 12(9): 1567-1570. Review article only.
Salvioni, A., F. Casilli, et al. (2001). "Comparison of enoxaparin and unfractionated heparin on thrombin generation in acute coronary syndromes without ST-segment elevation." Thrombosis & Haemostasis 86(4): 991-994. Trial focus is thrombogenic factors.
Savenkov, M. P., M. V. Borshchevskaia, et al. (1996). "[A trial of the use of low-molecular-weight heparin (fraksiparin) in myocardial infarct]." Terapevticheskii Arkhiv 68(8): 8-12. 0666d73c299e1a1df1b16f7db322595f.doc Page 55 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Trial looks at LMWH versus UFH for prevention of thromboembolic events in AMI.
Schreiber, W., D. Gabriel, et al. (2002). "Thrombolytic therapy after cardiac arrest and its effect on neurological outcome." Resuscitation 52(1): 63-9. Not relevant. Post VF arrest treatment with thrombolytics, no UFH/LMWH.
Schroeder, W. S. and P. J. Gandhi (2003). "Emergency management of hemorrhagic complications in the era of glycoprotein IIb/IIIa receptor antagonists, clopidogrel, low molecular weight heparin, and third-generation fibrinolytic agents." Current Cardiology Reports 5(4): 310-7. Not relevant, emphasis on reversal of agents and management hemorrhagic complications.
Schror, K. (2003). "Antithrombotic drugs in vascular medicine: A historical perspective." Seminars in Vascular Medicine 3(2): 97-105. Review article only.
Sekaran, N. K., D. J. Moliterno, et al. (2001). ""Hot" unstable angina--is it worse than subacute unstable angina? Results from the GUARANTEE Registry." Journal of Thrombosis & Thrombolysis 12(3): 207-16. Trial without comparison between UFH and LMWH.
Shannon, A. W. and R. A. Harrigan (2001). "General pharmacologic treatment of acute myocardial infarction." Emergency Medicine Clinics of North America 19(2): 417-31. Review article only.
Smith, R. E., G. E. Townsend, et al. (1996). "Enoxaparin for unstable angina and ancrod for cardiac surgery following heparin allergy." Annals of Pharmacotherapy 30(5): 476-480. Not relevant. Single case study of a patient with heparin allergy undergoing cardiac surgery.
Solomon, A. J., J. A. Breall, et al. (1998). "Unstable angina: Current recommendations and new directions." ACC Current Journal Review 7(3): 18-23. Review article only.
Spinier, S. A., S. M. Inverso, et al. (2004). "Antithrombotic therapy for acute coronary syndromes." J Am Pharm Assoc (Wash DC) 44(2 Suppl 1): S14-26; quiz S26-7. Review. Not specific to UFH v LMWH
Steg, P. G., E. Bonnefoy, et al. (2003). "Impact of time to treatment on mortality after prehospital fibrinolysis or primary angioplasty: data from the CAPTIM randomized clinical trial.[see comment]." Circulation 108(23): 2851-6. Focus on thrombolysis v primary PCI, not UFH v LMWH.
Stollerman, G. H. (2000). "Is heparin beneficial in acute coronary syndromes?" Hospital Practice 35(8). No abstract available.
Sutsch, G., F. W. Amann, et al. (2002). "Medical treatment of non-ST-elevation acute coronary syndrome." Therapeutische Umschau 59(2): 82-86. Review article only.
Swahn, E. and L. Wallentin (1997). "Low-molecular-weight heparin (Fragmin) during instability in coronary artery disease (FRISC)." American Journal of Cardiology 80(5 A) LMWH only, no comparison to UFH
Tani, S. and K. Kanmatsuse (2003). "[Anti thrombotic therapy after coronary thrombolysis]." Nippon Rinsho - Japanese Journal of Clinical Medicine 61(Suppl 4): 484-8. Review article without abstract.
The RESTORE Investigators (1997). "Effects of platelet glycoprotein IIb/IIIa blockade with tirofiban on adverse cardiac events in patients with unstable angina or acute myocardial infarction undergoing coronary angioplasty: randomized Efficacy Study of Tirofiban for Outcomes and REstenosis trial." Circulation 96(5): 1445-1453. No LMWH. 0666d73c299e1a1df1b16f7db322595f.doc Page 56 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
The Thrombolysis in Myocardial Infarction (TIMI) 11A Trial Investigators. (1997). "Dose-ranging trial of enoxaparin for unstable angina: results of TIMI 11A." J Am Coll Cardiol 29(7): 1474-1482. LMWH only, no comparison to UFH.
Tideman, P. A. (1999). "Antithrombins and the importance of good control." Australian & New Zealand Journal of Medicine 29(3): 444-451. Review article only.
Tolleson, T. R. and R. A. Harrington (1999). "Recent clinical trials in acute coronary syndromes without persistent ST elevation." Current Opinion in Cardiology 14(5): 403-411. Review article only.
Trujillo, T. C. and P. E. Nolan, Jr. (1998). "Unfractionated heparin in acute coronary syndromes: Has its time come and gone?" American Journal of Health System Pharmacy 55(22): 2402-2409. No abstract.
Tufano, A., A. M. Cerbone, et al. (2002). "The use of antithrombotic drugs in older people." Minerva Medica 93(1): 13-26. General review article.
Turpie, A. G. G. (1996). "New therapeutic opportunities for heparins: What does low molecular weight heparin offer?" Journal of Thrombosis & Thrombolysis 3(2): 145-149. Review article only.
Turpie, A. G. G. (1998). "Clinical potential of antithrombotic drugs in coronary syndromes." American Journal of Cardiology 82(5 B). Review article only.
Turpie, A. G. G. (1999). "Clinical trials of low molecular weight heparins." European Heart Journal Supplements 1(R): R18- R27. Review article only.
Turpie, A. G. G. and J. A. Mason (2002). "Review of enoxaparin and its clinical applications in venous and arterial thromboembolism." Expert Opinion on Pharmacotherapy 3(5): 575-598. Review article only.
Van den Merkhof, L. F., F. Zijlstra, et al. (1999). "Abciximab in the treatment of acute myocardial infarction eligible for primary percutaneous transluminal coronary angioplasty. Results of the Glycoprotein Receptor Antagonist Patency Evaluation (GRAPE) pilot study." Journal of the American College of Cardiology 33(6): 1528-32. Main focus of trial on G 11B/111A inhibitor, all patients received UFH, no comparison to LMWH.
Van de Werf, F. (2002). "ASSENT-3: Implications for future trial design and clinical practice." European Heart Journal 23(12): 911-912. Editorial only. Does support use of TNK and Enoxaparin in Pre-hospital setting (expert opinion).
Vila V, M.-S. V. R. E. P. E. P. F. R. M. A. J. (2001). "Effects of unfractionated and low molecular weight heparins on plasma levels of hemostatic factors in patients with acute coronary syndromes." Haematologica 86(7): 729-34. Study looks at in vivo effects of UFH and LMWH on thrombogenic factors.
Villareal, R. P., P. Kim, et al. (2001). "Unstable angina and non-ST-segment elevation myocardial infarction perspective on combination." Texas Heart Institute Journal 28(4): 276-287. General review, no comparison of UFH and LMWH.
Vorchheimer, D. A. and V. Fuster (1142). "Thrombin inhibitors in acute coronary artery disease." European Heart Journal 23(15): 1142-1144. Editorial only.
Wallentin, L. (2000). "Low molecular weight heparin in unstable coronary artery disease." Expert Opinion on Investigational Drugs 9(3): 581-592. Review article only. 0666d73c299e1a1df1b16f7db322595f.doc Page 57 of 57
REMEMBER TO SAVE THE BLANK WORKSHEET TEMPLATE USING THE FILENAME FORMAT
Walsh, C. R., D. M. Lloyd-Jones, et al. (2000). "Clinical trials of unfractionated heparin and low-molecular-weight heparin in addition to aspirin for the treatment of unstable angina pectoris: Do the results apply to all patients?" American Journal of Cardiology 86(9): 908-912. Trial does not directly compare treatments of UFH to LMWH, looks at outcomes of patients who meet exclusion criteria for major clinical trials comparing each drug type to aspirin.
Weaver, W. D., M. Cerqueira, et al. (1993). "Prehospital-initiated vs hospital-initiated thrombolytic therapy. The Myocardial Infarction Triage and Intervention Trial." JAMA 270(10): 1211-1216. No LMWH.
Welsh, R. C., J. Ornato, et al. (2003). "Prehospital management of acute ST-elevation myocardial infarction: A time for reappraisal in North America." American Heart Journal 145(1): 1-8. Review article only.
White, H. D., C. J. Ellis, et al. (1998). "Low molecular weight heparins in acute ischaemic syndromes." Australian & New Zealand Journal of Medicine 28(4): 555-557. Review article only.
Wiszniewski, A., A. Misiak, et al. (2002). "Low molecular weight and unfractionated heparins in the prevention of deep vein thrombosis after arterial reconstruction. [Polish, English]." Polski Przeglad Chirurgiczny 74(11): 979-989. Study of venous thromboembolism.
Wolf, H., A. Encke, et al. (1991). "Comparison of the efficacy and safety of Sandoz low molecular weight heparin and unfractionated heparin: Interim analysis of a multicenter trial." Seminars in Thrombosis & Hemostasis 17(4): 343-346. Trial on perioperative prophylaxis of thromboembolism.
Woo, K. S. and H. D. White (1994). "Thrombolytic therapy in acute myocardial infarction." Current Opinion in Cardiology 9(4): 471-82. Review article with emphasis on fibrinolytics.
Wong, G. C., R. P. Giugliano, et al. (2003). "Use of low-molecular-weight heparins in the management of acute coronary artery syndromes and percutaneous coronary intervention." Journal of the American Medical Association 289(3): 331-342. Systematic review, no meta-analysis.
Wright, R. S., S. L. Kopecky, et al. (2000). "Update on intravenous fibrinolytic therapy for acute myocardial infarction." Mayo Clin Proc 75(11): 1185-91; quiz 1192. Review article with emphasis on fibrinolytics.
Zaacks, S. M., P. R. Liebson, et al. (1999). "Unstable angina and non-Q wave myocardial infarction: Does the clinical diagnosis have therapeutic implications?" Journal of the American College of Cardiology 33(1): 107-118. Review article only.
Zijlstra, F., N. Ernst, et al. (2002). "Influence of prehospital administration of aspirin and heparin on initial patency of the infarct-related artery in patients with acute ST elevation myocardial infarction." Journal of the American College of Cardiology 39(11): 1733-7. Prehospital trial, but did not include LMWH use.
Zimmermann, A. T., W. S. Jeffries, et al. (2003). "Utility of a weight-based heparin nomogram for patients with acute coronary syndromes." Internal Medicine Journal 33(1-2): 18-25. Trial with UFH only. Supports weight based UFH dosing