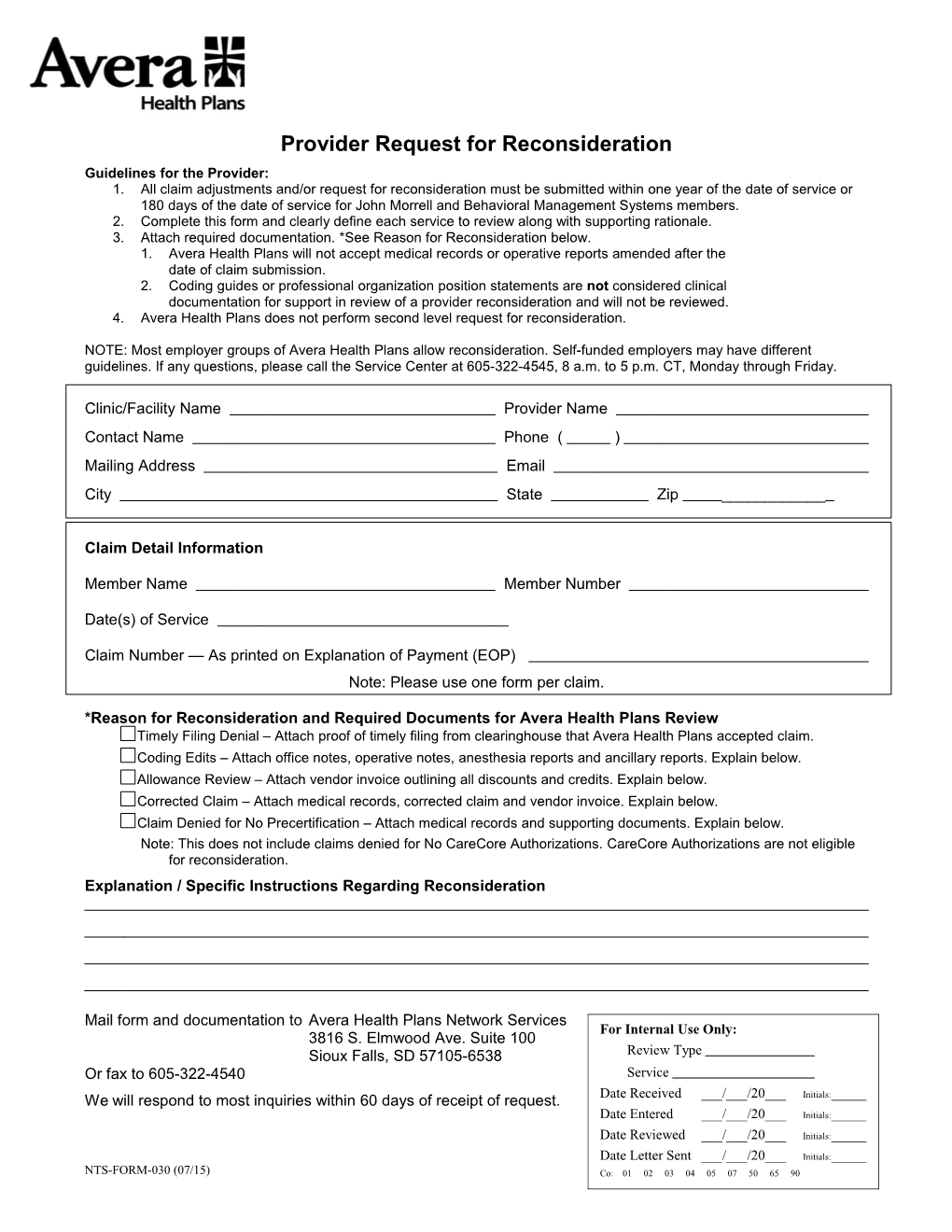
Provider Request for Reconsideration Guidelines for the Provider: 1. All claim adjustments and/or request for reconsideration must be submitted within one year of the date of service or 180 days of the date of service for John Morrell and Behavioral Management Systems members. 2. Complete this form and clearly define each service to review along with supporting rationale. 3. Attach required documentation. *See Reason for Reconsideration below. 1. Avera Health Plans will not accept medical records or operative reports amended after the date of claim submission. 2. Coding guides or professional organization position statements are not considered clinical documentation for support in review of a provider reconsideration and will not be reviewed. 4. Avera Health Plans does not perform second level request for reconsideration.
NOTE: Most employer groups of Avera Health Plans allow reconsideration. Self-funded employers may have different guidelines. If any questions, please call the Service Center at 605-322-4545, 8 a.m. to 5 p.m. CT, Monday through Friday.
Clinic/Facility Name Provider Name Contact Name Phone ( ) Mailing Address Email City State Zip ______
Claim Detail Information
Member Name Member Number
Date(s) of Service
Claim Number — As printed on Explanation of Payment (EOP) Note: Please use one form per claim.
*Reason for Reconsideration and Required Documents for Avera Health Plans Review Timely Filing Denial – Attach proof of timely filing from clearinghouse that Avera Health Plans accepted claim. Coding Edits – Attach office notes, operative notes, anesthesia reports and ancillary reports. Explain below. Allowance Review – Attach vendor invoice outlining all discounts and credits. Explain below. Corrected Claim – Attach medical records, corrected claim and vendor invoice. Explain below. Claim Denied for No Precertification – Attach medical records and supporting documents. Explain below. Note: This does not include claims denied for No CareCore Authorizations. CareCore Authorizations are not eligible for reconsideration. Explanation / Specific Instructions Regarding Reconsideration
Mail form and documentation to Avera Health Plans Network Services For Internal Use Only: 3816 S. Elmwood Ave. Suite 100 Sioux Falls, SD 57105-6538 Review Type Or fax to 605-322-4540 Service We will respond to most inquiries within 60 days of receipt of request. Date Received ___/___/20___ Initials:_____ Date Entered ___/___/20___ Initials:_____
Date Reviewed ___/___/20___ Initials:_____
Date Letter Sent ___/___/20___ Initials:_____ NTS-FORM-030 (07/15) Co: 01 02 03 04 05 07 50 65 90