PSYCHOLOGICAL THERAPIES FOR DEPRESSION To read up on psychological therapies for depression, refer to pages 459–468 of Eysenck’s A2 Level Psychology.
Ask yourself How can the behavioural approach be applied to the treatment of depression? How can the cognitive approach be applied to the treatment of depression? Which psychological therapy do you think will be most effective for depression?
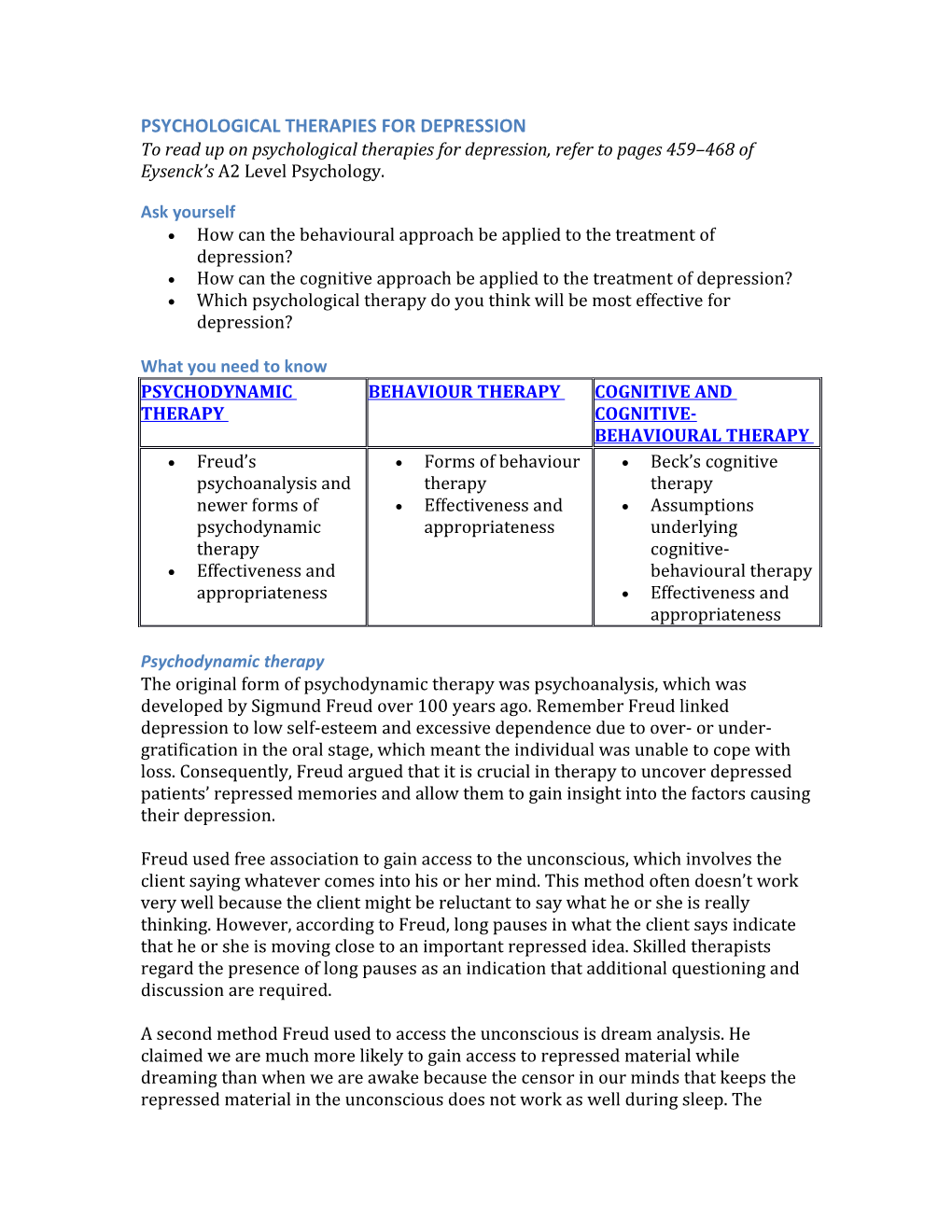
What you need to know PSYCHODYNAMIC BEHAVIOUR THERAPY COGNITIVE AND THERAPY COGNITIVE- BEHAVIOURAL THERAPY Freud’s Forms of behaviour Beck’s cognitive psychoanalysis and therapy therapy newer forms of Effectiveness and Assumptions psychodynamic appropriateness underlying therapy cognitive- Effectiveness and behavioural therapy appropriateness Effectiveness and appropriateness
Psychodynamic therapy The original form of psychodynamic therapy was psychoanalysis, which was developed by Sigmund Freud over 100 years ago. Remember Freud linked depression to low self-esteem and excessive dependence due to over- or under- gratification in the oral stage, which meant the individual was unable to cope with loss. Consequently, Freud argued that it is crucial in therapy to uncover depressed patients’ repressed memories and allow them to gain insight into the factors causing their depression.
Freud used free association to gain access to the unconscious, which involves the client saying whatever comes into his or her mind. This method often doesn’t work very well because the client might be reluctant to say what he or she is really thinking. However, according to Freud, long pauses in what the client says indicate that he or she is moving close to an important repressed idea. Skilled therapists regard the presence of long pauses as an indication that additional questioning and discussion are required.
A second method Freud used to access the unconscious is dream analysis. He claimed we are much more likely to gain access to repressed material while dreaming than when we are awake because the censor in our minds that keeps the repressed material in the unconscious does not work as well during sleep. The repressed material is included in our dreams in a disguised or symbolic form because of its unacceptable nature. Freud called the dream as we remember it the manifest content and the true or underlying meaning the latent content. Dream analysis involves interpretation of the symbols in the manifest content and questioning clients about their dreams to work out the latent content.
Progress in therapy depends partly on transference. This involves the client transferring onto the therapist the powerful emotional reactions previously directed at his/her own parents or other highly significant others. These intense feelings can be negative or positive and the client is usually unaware of what is happening. Transference often provides a direct link back to the client’s childhood by providing a re-creation of dramatic conflicts that were experienced at that time. As a result, transference can facilitate the uncovering of repressed memories.
Psychodynamic therapy today has moved away from Freud’s original approach because patients’ social relationships are considered, and current psychotherapy does not place the same emphasis on childhood experiences that Freud did.
EVALUATION OF PSYCHODYNAMIC THERAPY Effectiveness Major depressive vs. bipolar disorder. Psychodynamic therapy (in line with most other forms of therapy) is more effective in treating major depressive disorder than bipolar disorder. Strong empirical support. Traditional psychodynamic therapy was often found to have very limited effectiveness. However, modern forms of psychotherapy have been found to be much more effective. For example, Leichsenring (2001, see A2 Level Psychology page 461) used the findings from a meta-analysis to compare the effectiveness of psychodynamic therapy and cognitive-behavioural therapy (CBT) and found in 58 of 60 comparisons no significant differences between the two. Thus, psychodynamic therapy may no longer compare unfavourably to CBT. Limited effectiveness for bipolar disorder. Colom et al. (1998, see A2 Level Psychology page 461) compared studies in which psychodynamic therapy and CBT therapy had been used. There was no clear evidence that either form of therapy was effective. Sajatovic et al. (2007, see A2 Level Psychology page 461), however, argue that the use of psychodynamic therapy with bipolar patients makes patients better informed and more likely to continue taking their medication. Thus, the therapy on its own has limited effectiveness but is not without use if combined with drug therapy.
Appropriateness The cognitive nature of the treatment. Psychodynamic therapy focuses on the cognitive, helping patients to change their cognitive beliefs about themselves, and as cognitive distortions often underpin depression this makes the nature of the therapy appropriate. The focus on current problems. The fact more modern forms of psychotherapy focus on current problems again makes this treatment appropriate. Ignores motivational factors. Psychodynamic therapy doesn’t treat motivational issues, which means it lacks appropriateness because many of the problems faced by depressed patients revolve around their loss of motivation and disengagement from the world. Ignores behavioural problems. Doesn’t focus on patients’ behavioural problems, such as their very low involvement in pleasurable activities. Requires patient to be active and articulate. Psychodynamic therapy requires patients to participate fully in complex discussions with the therapist. They may be too passive and lacking in motivation to do this. Slow-acting. The therapy takes a long time, which can be de-motivating for the patient. Drop-out rate. The fact the therapy takes time and requires the patient to be active can lead patients to drop out because these challenges make it hard for them to believe in the therapy, given that they are generally pessimistic in outlook. Less appropriate for bipolar disorder. The “talking cure” that psychodynamic therapists provide is of limited use for the complexities of bipolar disorder. YAVIS. Psychodynamic therapy may work for some better than others, i.e. young, attractive, verbally skilled, intelligent, and successful, which forms the acronym YAVIS.
Behaviour therapy Behaviour therapy focuses on rewarding non-depressive behaviours and not rewarding depressive behaviour. Particular focus is given to using reinforcement to improve depressed patients’ social skills.
Therapists use the Pleasant Events Schedule and an Activity Schedule to help clients to set up a weekly schedule for engaging in pleasurable activities. Behavioural activation recommended by Beck et al. (1979, see A2 Level Psychology page 463) encourages the patient to become engaged in activities and situations that provide reinforcement or reward and that fit in with the individual’s long-term goals. The client schedules daily activities, rates how much pleasure and sense of achievement are associated with each activity, and explores different forms of behaviour designed to achieve his or her goals.
EVALUATION OF BEHAVIOUR THERAPY Effectiveness Moderate effectiveness. Behaviour therapy of the kinds we have discussed is of moderate effectiveness in treating major depressive disorder. Compares unfavourably with other treatments. Patients receiving behaviour therapy often exhibit less improvement than those receiving cognitive or drug therapy (Comer, 2001, see A2 Level Psychology page 463). May not work for severe depression. It has generally been argued that behaviour therapy is mainly effective with patients who have relatively mild depression. It is hard to see how a severely depressed patient could engage with rating pleasurable activities. Empirical support. Evidence suggests it may be more effective for severe depression than previously thought. Dimidjian et al. (2006, see A2 Level Psychology page 463) compared the effectiveness of behavioural activation with that of cognitive therapy and drug therapy using the SSRI paroxetine. No differences in improvement between the treatments were found for less severely depressed patients. Behavioural activation was found to be most effective for the severely depressed because full recovery was achieved by 56% of the patients receiving behaviour therapy compared to only 36% of those receiving cognitive therapy and 23% of those receiving drug therapy. Low effectiveness for bipolar disorder. Behavioural therapy is of little use for patients in the manic phase of bipolar as they are generally already engaged in a number of pleasurable activities.
Appropriateness The motivational nature of the therapy. Patients with depression have low motivation to engage in pleasurable activities and so the treatment of this is highly appropriate. Low drop-out rate. Most patients can see the value of increasing their involvement in such activities and this encourages them to continue with treatment. Ignores cognition. Behavioural treatment does not treat the cognitive symptoms of depression, and so does not deal with the underlying problems. Treats symptoms not causes. It can be argued that, because the behavioural treatment ignores cognition and just focuses on behaviour, the treatment is superficial and so just treats the symptoms (the behaviour). This means that symptom substitution may occur, which means that once one maladaptive behaviour has disappeared another symptom will develop and the depression will resurface because the underlying causes have not been dealt with. Reductionism. The fact that important factors are ignored such as cognition makes the treatment over simplistic.
Cognitive and cognitive-behavioural therapy Aaron Beck has contributed the most towards the development of cognitive therapy for depression. According to Beck, the negative and unrealistic beliefs of depressed clients need to be challenged. This is accomplished through a stage process: the first stage of cognitive therapy involves the therapist and the client agreeing on the nature of the problem and the goals for therapy. In the next stage the client’s negative thoughts are challenged. This involves homework assignments and hypothesis testing. Clients typically predict that carrying out their homework assignments will make them feel anxious or depressed, and so they are told to test their predictions. The clients’ hypotheses are generally shown to be too pessimistic and discovering that many of their fears are groundless speeds recovery (Beck et al., 1979, see A2 Level Psychology page 464).
Cognitive therapists have expanded upon their original approach to include the behavioural element thus recognising the interconnectedness of cognition, emotion, and behaviour. Cognitive-behavioural therapy (CBT) involves a cognitive element, challenging negative thinking, and a behavioural element, learning adaptive behaviours. Thus, CBT recognises that it is important to focus on changing depressed individuals’ behaviour as well as their ways of thinking about themselves and the world around them. Kendall and Hammen (1998, see A2 Level Psychology page 465) have identified four basic assumptions underlying cognitive-behavioural therapy: 1. Patients’ interpretations of themselves and the world around them often differ from what is actually the case. 2. Thoughts, behaviour, and feelings are all interrelated and so it is wrong to identify one of these factors (e.g. behaviour) as being more important than the others. 3. Therapy needs to change the ways people think about themselves and the world around them. 4. Therapy needs to change the client’s cognitive processes and his or her behaviour, because the benefits will be greater than if only one element is changed.
EVALUATION OF COGNITIVE AND COGNITIVE-BEHAVIOURAL THERAPY Effectiveness Strong empirical support. Elkin (1994, see A2 Level Psychology page 466) studied depressed patients who were assigned to different treatments: Beck’s cognitive therapy, treatment with the tricyclic antidepressant drug imipramine, and a placebo group that received no specific treatment. 55% of patients who completed treatment made an almost full recovery in the drug and cognitive treatment and this was much higher than the placebo group. Also note the findings by Hollon et al. (2005, see A2 Level Psychology page 466) in the section on drug therapy, which found drugs compared unfavourably to CBT, thus supporting its effectiveness. Curative not just palliative. Research suggests that cognitive therapy is a curative rather than a palliative treatment because it treats the underlying causes, the faulty cognition, rather than just symptoms. Thus, it is more effective than drug and behavioural therapy because cognitive treatment treats causes not just symptoms. Evidence for a curative effect is provided by Segal et al. (2006, see A2 Level Psychology page 466) who tested patients that had recovered from depression after receiving drug and behavioural treatment. After treatment patients were made to feel sad and those who had previously received drug therapy showed greater negative attitudes than those who had received cognitive-behavioural therapy. This suggests CBT provided greater protection against relapse than drug therapy. Long-lasting effects. CBT produces long-lasting beneficial changes in patients’ dysfunctional attitudes so they are relatively unlikely to relapse back into depression. Moderately effective for bipolar disorder. Lam et al. (2000, see A2 Level Psychology page 467) compared patients with bipolar disorder receiving drug therapy with patients receiving cognitive therapy and drug therapy over a 30-month period. There were two main findings. The cognitive therapy patients spent 12% less time than the drug-only patients in bipolar episodes, and they reported better mood states and social functioning, and fewer dysfunctional attitudes about goal attainment. Reliability. Jones (2004, see A2 Level Psychology page 467) also found that bipolar patients who received CBT had fewer depressive symptoms, better social functioning, and a lower risk of relapse and so there is consistency (reliability) in the evidence for CBT.
Appropriateness The cognitive nature of depressive symptoms. Most of the symptoms of depression have a cognitive basis and so cognitive therapy and CBT are appropriate to attempt to change negative and irrational attitudes into more positive and realistic ones. Dual focus of CBT. CBT combines features of cognitive therapy and behavioural therapy. As such, it is broader and more effective than either of the forms of therapy from which it arose. The behavioural aspect. The behavioural element of CBT is appropriate in that it also focuses on increasing depressed patients’ involvement in pleasurable and rewarding activities. Cognitions may be realistic rather than faulty. The depressed person’s beliefs may be realistic and so not cognitive distortions. Maybe the person’s economic prospects are not good or they struggle with relationships because they lack social skills, and so treatment is not as straightforward as changing faulty cognitions. The effects of changing faulty cognitions may be exaggerated. Those who advocate Cognitive Behavioural Therapy may exaggerate the importance of cognitive processes. Many clients develop more rational and less distorted ways of thinking about important issues with no beneficial changes in their maladaptive behaviour. Insufficient consideration of personal relationships. Cognitive and cognitive-behavioural therapists don’t consider these relationships sufficiently, which is a weakness because these are often at the heart of the depressed person’s problems. Relapse rates. Many depressed patients do relapse, which suggests that the therapy might simply suppress patients’ negative and dysfunctional beliefs rather than eliminating them. This does question how much the treatment is curative but on the other hand relapse rate are usually lower with than other forms of treatment. Less invasive than biological therapies. CBT does not have the same undesirable side effects as biological treatments and so on these grounds alone some would prefer to use this therapy. So what does this mean? Any comparisons of the effectiveness of different treatments should be treated with caution as it is difficult to know if differences are due to the actual therapy or the individual differences of the patient or therapist. Therapy depends in part on the skills of the therapist and so differences in improvement may be due to such differences rather than the treatment itself. The fact that patients usually choose their own treatment and so are a self-selected sample also complicates comparisons of treatments. Moreover, recovery may not be due to the specific nature of the treatment but to general factors that underpin all treatments, such as the effect of having someone sensitive to talk to and being able to express all worries and fears, which is known as the “general therapy effect”.
Assessing the effectiveness of treatments is further complicated by the “hello– goodbye effect” whereby patients overestimate their symptoms at the start of treatment and underestimate their symptoms at the end. Another issue is publication bias whereby significant findings are published more than non- significant ones. These biases may make therapies appear more effective than they really are. Imagine if all the findings that a therapy doesn’t work are suppressed, then of course it’s going to appear effective!
Ethical issues raise further concerns as can the patient really give fully informed consent? A number of things can limit this, such as the patient not being provided with enough information about the treatment, they may not remember the information accurately, and they may agree just because they respect the therapist rather than understand the treatment.
However, in spite of all of these issues it is important to understand as best we can the effectiveness and appropriateness of therapies because treatment is usually better than no treatment, even if part of the improvement is a placebo effect. The psychological therapies do show there is more to treatment than just drugs for depression. However, many would consider the optimal approach to treatment is a multi-dimensional one in which drugs are combined with one or more other treatments. However, on the other hand, given that CBT is more curative than other therapies and doesn’t have the unpleasant side effects that biological therapies have, many may prefer to opt for this.
Over to you (a) Outline one or more psychological therapy(ies) for depression. (9 marks) (b) Evaluate the therapy(ies) described in (a). (16 marks)