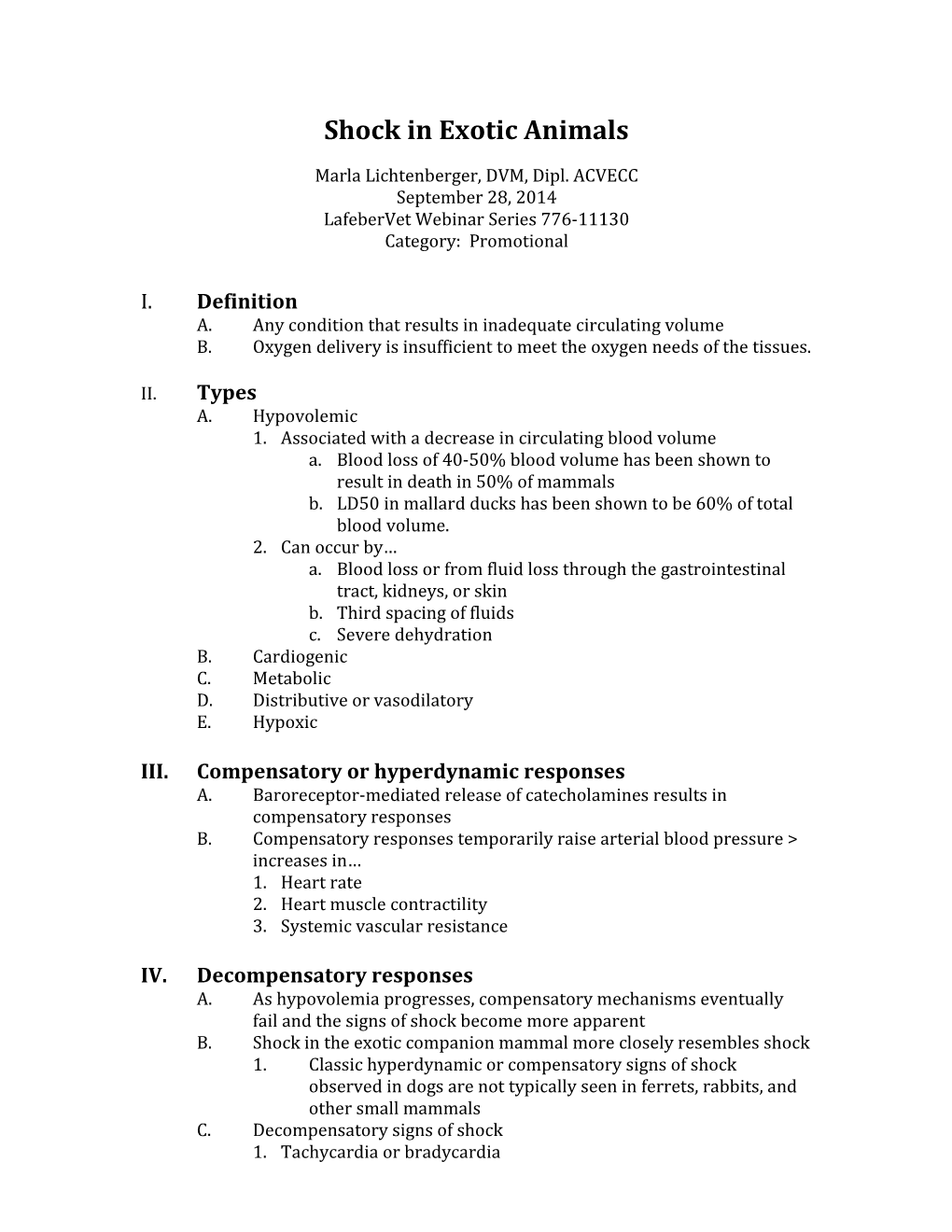
Shock in Exotic Animals
Marla Lichtenberger, DVM, Dipl. ACVECC September 28, 2014 LafeberVet Webinar Series 776-11130 Category: Promotional
I. Definition A. Any condition that results in inadequate circulating volume B. Oxygen delivery is insufficient to meet the oxygen needs of the tissues.
II. Types A. Hypovolemic 1. Associated with a decrease in circulating blood volume a. Blood loss of 40-50% blood volume has been shown to result in death in 50% of mammals b. LD50 in mallard ducks has been shown to be 60% of total blood volume. 2. Can occur by… a. Blood loss or from fluid loss through the gastrointestinal tract, kidneys, or skin b. Third spacing of fluids c. Severe dehydration B. Cardiogenic C. Metabolic D. Distributive or vasodilatory E. Hypoxic
III. Compensatory or hyperdynamic responses A. Baroreceptor-mediated release of catecholamines results in compensatory responses B. Compensatory responses temporarily raise arterial blood pressure > increases in… 1. Heart rate 2. Heart muscle contractility 3. Systemic vascular resistance
IV. Decompensatory responses A. As hypovolemia progresses, compensatory mechanisms eventually fail and the signs of shock become more apparent B. Shock in the exotic companion mammal more closely resembles shock 1. Classic hyperdynamic or compensatory signs of shock observed in dogs are not typically seen in ferrets, rabbits, and other small mammals C. Decompensatory signs of shock 1. Tachycardia or bradycardia a. Most small mammals with hypovolemic shock demonstrate a normal or slow heart rate b. HR < 200 bpm 2. Arrhythmia or pulse deficits 3. Pulmonary edema 4. Pallor 5. Prolonged capillary refill time 6. Weak peripheral pulses, cool extremities 7. Hypothermia (temp < 98 F) 8. Dull mentation 9. BP < 90 mmHg C. If left untreated, shock eventually leads to… 1. Acid-base abnormalities 2. Organ failure 3. Cardiac arrest 4. Death
V. Treatment goal: Support the cardiovascular system with fluids and improve oxygen delivery to tissues A. Early recognition of shock B. Supplemental oxygen C. Fluid therapy 1. Single most important treatment for shock a. Expands the vascular space i. Improving cardiac output ii. Restoring tissue perfusion b. An intravenous or intraosseous catheter is required followed by administration of a shock fluid bolus. 2. Crystalloids a. “Interstitial hydrators” that only briefly expand intravascular volume b. Rapidly redistribute i. After 1 hour only a small fraction remains within the circulatory system ii. This means that large volumes of crystalloids must be administered. c. Buffered crystalloid solutions i. Containing acetate, gluconate or lactate ii. Usually indicated for shock iii. Lactate may not be tolerated with end-stage liver disease d. Normal saline i. Head trauma ii. Conditions causing hyperkalemia Urinary obstruction
2 Oliguric renal failure Hypercalcemia, hypochloremic metabolic acidosis d. Large volumes i. Required when crystalloids alone are given ii. Like cats, small mammals do not tolerate rapid, large volume boluses iii. Large increases in intravascular fluid can lead to tissue edema in some patients, including significant cerebral edema or pulmonary fluid accumulation
3. Hypertonic saline a. Hyperosmolar crystalloid i. Useful in hypovolemia ii. Uses one-fourth the volume of crystalloids b. Hyperosmolarity causes rapid intravascular volume expansion by drawing fluids from all body compartments into the intravascular space c. 3 ml/kg slow bolus IV or IO over 10 minutes d. Potential adverse effects i. Hypernatremia ii. Hyperchloremia iii. Hypokalemia iv. Dehydration 3. Colloids a. Examples: i. Hetastarch (3 ml/kg IV or IO over 5-10 min) ii. Dextran 70 iii. Oxyglobin, whole blood, plasma; b. Another type of intravascular volume expander c. Contain large molecular weight substances that generally are not able to pass through capillary membranes d. Indications: increase in capillary permeability or reduced tolerance for large volume resuscitation i. Head injury ii. Pulmonary contusions iii. Myocardial dysfunction iv. Hypovolemic cats e. Blood products are given when albumin, antithrombin, coagulation factors, platelets and/or red blood cells are required
4. Combination therapy 3 a. Rapid effects of hypertonic saline can be maintained by adding a colloid b. Crystalloid + colloid c. Increases the duration of volume expansion from 30 minutes to 3 hours d. Isotonic crystalloids (10 ml/kg) + HES in increments of 3-5 ml/kg can be repeated over 15 min until systolic BP > 90 mm Hg and/or improvement in clinical markers D. Supplemental heat 1. As body temperature falls, adrenergic receptors can become refractory to catecholamine release a. As rectal temp approaches 100 F, adrenergic receptors begin to respond to catecholamines allowing compensatory responses to occur 2. Techniques a. Rewarm the patient over 30-60 min using forced warm air blankets, incubators, or circulating warm water blankets b. Warm fluids to patient body temp (100-103 F) c. Monitor body temperature closely i. Make sure rewarming does not occur too quickly ii. Prevent hyperthermia E. Corticosteroids 1. Not routinely indicated 2. No longer recommended as a first line of therapy
VI. Monitoring A. Monitor parameters during and after resuscitation B. Clinical markers
4 1. Respiratory rate 1. Blood pressure (measure 2. Respiratory frequently) effort C. Overhydration 3. Auscultation 1. Reassess and readjust 4. Heart rate fluid therapy at frequent 5. Heart rhythm intervals to obtain 6. Mental status optimal tissue perfusion 7. Skin turgor 2. Signs of overhydration 8. Pulse quality a. Serous nasal 9. Mucous discharge membrane color b. Tachypnea 10. Capillary refill c. Dyspnea time d. Pulmonary edema 11. Body e. Subcutaneous temperature edema 12. Urine production 3. If the patient is known to 13. Oxygen be hypoproteinemic, give saturation hetastarch 0.8 ml/kg/h 14. Body weight during rehydration
VII. Resources and recommended reading
5