Delaware Health and Social Services Medical Care Advisory Council (MCAC) Meeting Minutes
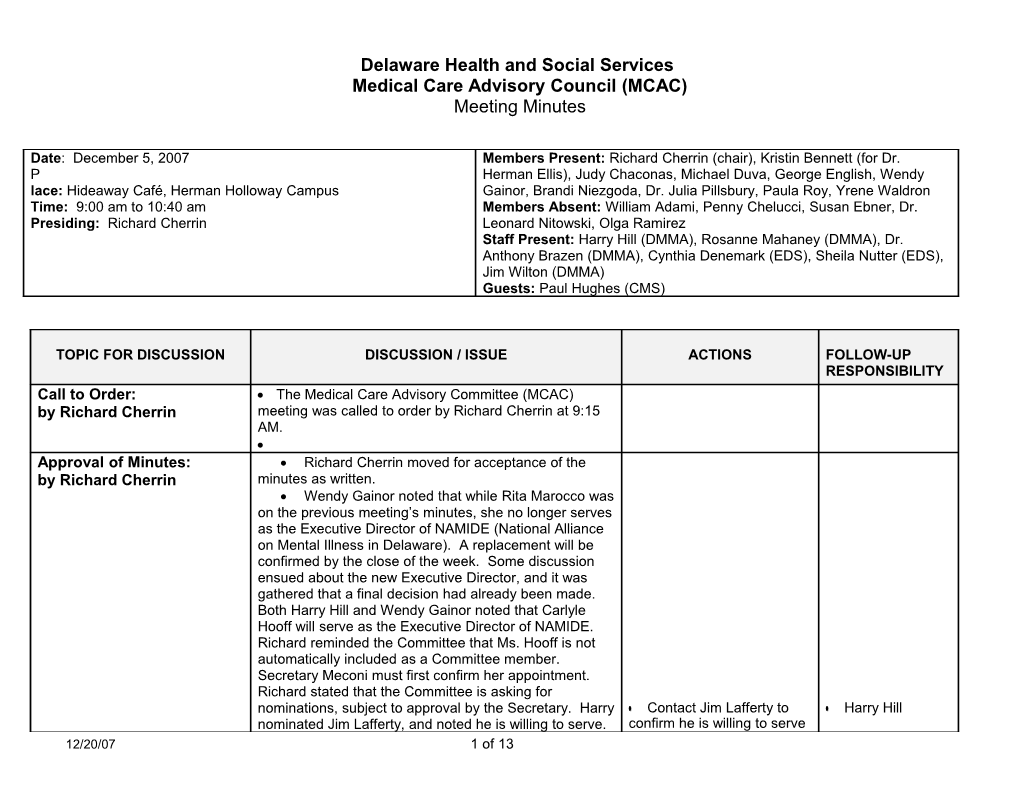
Date: December 5, 2007 Members Present: Richard Cherrin (chair), Kristin Bennett (for Dr. P Herman Ellis), Judy Chaconas, Michael Duva, George English, Wendy lace: Hideaway Café, Herman Holloway Campus Gainor, Brandi Niezgoda, Dr. Julia Pillsbury, Paula Roy, Yrene Waldron Time: 9:00 am to 10:40 am Members Absent: William Adami, Penny Chelucci, Susan Ebner, Dr. Presiding: Richard Cherrin Leonard Nitowski, Olga Ramirez Staff Present: Harry Hill (DMMA), Rosanne Mahaney (DMMA), Dr. Anthony Brazen (DMMA), Cynthia Denemark (EDS), Sheila Nutter (EDS), Jim Wilton (DMMA) Guests: Paul Hughes (CMS)
TOPIC FOR DISCUSSION DISCUSSION / ISSUE ACTIONS FOLLOW-UP RESPONSIBILITY Call to Order: The Medical Care Advisory Committee (MCAC) by Richard Cherrin meeting was called to order by Richard Cherrin at 9:15 AM. Approval of Minutes: Richard Cherrin moved for acceptance of the by Richard Cherrin minutes as written. Wendy Gainor noted that while Rita Marocco was on the previous meeting’s minutes, she no longer serves as the Executive Director of NAMIDE (National Alliance on Mental Illness in Delaware). A replacement will be confirmed by the close of the week. Some discussion ensued about the new Executive Director, and it was gathered that a final decision had already been made. Both Harry Hill and Wendy Gainor noted that Carlyle Hooff will serve as the Executive Director of NAMIDE. Richard reminded the Committee that Ms. Hooff is not automatically included as a Committee member. Secretary Meconi must first confirm her appointment. Richard stated that the Committee is asking for nominations, subject to approval by the Secretary. Harry Contact Jim Lafferty to Harry Hill nominated Jim Lafferty, and noted he is willing to serve. confirm he is willing to serve 12/20/07 1 of 13 DHSS MCAC Meeting Minutes
TOPIC FOR DISCUSSION DISCUSSION / ISSUE ACTIONS FOLLOW-UP RESPONSIBILITY Wendy thought that Jim would serve as an excellent as a member of the MCAC Approval of Minutes candidate, as he is involved with the mental health (continued): taskforce. by Richard Cherrin Richard moved for the acceptance of the minutes as written. Paula Roy seconded, and the motion was approved. New Business: Richard brought the issue of meeting frequency to the Frequency of Committee table. Richard reminded the Committee that the group Meetings has the possibility of meeting quarterly. by Richard Cherrin and Mollie Daughtrey prepared a tentative 2008 meeting Committee schedule as follows: (bi-monthly) 1/9/08, 3/12/08, 5/14/08, 7/9/08, 9/10/08, 11/12/08 and (quarterly) 2/13/08, 5/14/08, 8/13/08, 11/12/08. Yrene Waldron thought that quarterly meetings would be a good idea as many members hold a tight schedule. She added that should an urgent matter arise, the Committee could perhaps agree to a conference call on the issue at hand. Wendy Gainor and George English both agreed this was a good idea. Kris Bennett suggested that the Committee take unexpected cancellations into account, and schedule a bi-monthly meeting with the intention of canceling some meetings (perhaps canceling a July meeting as well as another date). Yrene and Richard did express one concern with quarterly meetings—if an unexpected cancellation arose there would be a large space of time between meetings. Dr. Brazen suggested moving the proposed August 13, 2008 meeting to September, and the November meeting to December. Yrene proposed a conference call instead of a live meeting every other month. Yrene noted that conference calls work well for her and her business associates. Paula Roy also proposed canceling a meeting
12/20/07 2 of 13 DHSS MCAC Meeting Minutes
TOPIC FOR DISCUSSION DISCUSSION / ISSUE ACTIONS FOLLOW-UP RESPONSIBILITY depending on tentative attendance numbers. New Business: Richard proposed the next meeting occur in March Frequency of Committee 2008, followed by one meeting each quarter – June Meetings (continued) 2008, September 2008, and December 2008. This by Richard Cherrin and schedule would avoid August vacations. The Committee Committee would still meet on the second Wednesday of the designated month. Harry agreed that he liked this option. And, to further support the meeting dates, Harry noted the September meeting would fall nicely before the Office of Management and Budget (OMB) Hearings and the December meeting would fall nicely before the Joint Finance Committee (JFC) meeting. The Committee was in consensus, agreeing to the above quarterly meeting schedule. Harry noted that in the event a quarterly meeting must be canceled, the Division of Medicaid and Medical Assistance (DMMA) would quickly reschedule the meeting so that it would fall shortly after the original date. Richard moved for the acceptance of the quarterly Distribute and post the Mollie Daughtrey meeting schedule (3/12/08, 6/11/08, 9/10/08, 12/10/08). 2008 meeting schedule, Paula Roy seconded, and the motion was approved. make accommodations for the meetings. Old Business: Cindy Denemark reminded the Committee that the Pharmacy Update Drug Utilization Review (DUR) Board met on November by Cindy Denemark 19, 2007. The Board is waiting on several items: 1. The December release of the Federal Upper Limit (FUL) from the Centers for Medicare and Medicaid Services (CMS) 2. Provider feedback on the new FUL. Cindy stated that the National Association of Chain Drug Stores has filed a lawsuit against CMS for an inequitable definition of Average Manufacturing Price (AMP). Cindy also noted that many drugs are losing their patents, shortly. Companies must be creative with 12/20/07 3 of 13 DHSS MCAC Meeting Minutes
TOPIC FOR DISCUSSION DISCUSSION / ISSUE ACTIONS FOLLOW-UP RESPONSIBILITY formularies. Old Business: The next DUR Board meeting will be held on January Pharmacy Update 14, 2008. (continued) The Pharmaceutical and Therapeutics (P&T) by Cindy Denemark Committee will meet on February 14, 2008. Richard asked if there were any questions from the Committee. No response was heard.
Old Business: Medicaid Overview by Harry Hill
Harry reminded the Committee that the fiscal year 2009 budget will be very tight. In fiscal year 2009, DMMA is requesting $558 million in general funds (which totals $1.2 billion with federal matching funds). Harry thanked DMMA’s budget staff. The staff perform an amazing job, in that their fiscal projections cannot be off by even 1% as this would mean DMMA would need an additional $5.6 million which was not in the State budget. The OMB Hearings took place last week, before Budget Director Jennifer Davis. Secretary Meconi spoke for DHSS and all the divisions.
12/20/07 4 of 13 DHSS MCAC Meeting Minutes
TOPIC FOR DISCUSSION DISCUSSION / ISSUE ACTIONS FOLLOW-UP RESPONSIBILITY Harry reminded the Committee that MCAC supported Medicaid Buy-In (MBI). DMMA requested approximately $928,600 for full-year funding in fiscal year 2009. Harry stated that DMMA has requested an additional $41 million for Medicaid inflation in fiscal year 2009. Old Business: Medicaid inflation involves an increase in the number of Medicaid Overview clients (which has seen approximately a 4% growth), and an increase in the cost of services and changes in (continued) the mix of services. by Harry Hill Richard inquired about the total number of Medicaid clients. Harry responded that 157,000 total citizens are currently funded by Medicaid in Delaware (146,000 strictly receive Medicaid only while the remaining 11,000 received various ancillary services). Funding for Money Follows the Person (MFP) is drawn from tobacco funds (approximately $691,000). The MFP goal is to shift the balance from institutions to community-based placements. Twenty-five individuals per year (for five years) will be placed in a less- restrictive, community-based environment. Yrene noted that the cost for elderly care will only grow, as our aging population is increasing. A lengthy discussion ensued over the issue of the Children’s Health Insurance Program (CHIP). POVERTY LIMIT: Harry reported that CHIP has sufficient funding in the State of Delaware. At present, the State covers those at 200% of the poverty limit (not including adults without children). Paula Roy noted that states requesting a higher poverty limit are oftentimes not receiving approval from CMS (as the states must demonstrate they are first serving 95% of their eligible children before expanding the eligibility population). PARTICIPATION: Harry stated that the University of Delaware reports approximately 13,000 children in our state are eligible for CHIP. We provide services to about 10,000 per year, with 5,000 receiving care at any given 12/20/07 5 of 13 DHSS MCAC Meeting Minutes
TOPIC FOR DISCUSSION DISCUSSION / ISSUE ACTIONS FOLLOW-UP RESPONSIBILITY time. Paula noted that the program experiences some churn. Harry responded, yes, children go on and off the program. Many children go back and forth between CHIP and Medicaid. ELIGIBILTY: Yrene inquired what 200% of the poverty limit was, and Paula responded $41,000 annually, for a family of four. George English asked if Old Business: CHIP eligibility was determined on a monthly basis and Medicaid Overview Harry responded yes. Shelia Nutter added that if (continued) parents pay for three months, they receive one month at by Harry Hill no charge. George noted that the burden of compliance falls on the parent. Oftentimes, this issue is hard for the parent to manage. BARRIERS: Yrene asked what barriers prevent children from enrolling in CHIP. Dr. Pillsbury responded that a barrier was reoccurring recertification. She stated that if parents are turned down or loose eligibility, they are oftentimes too discouraged to apply again. Additionally, Dr. Pillsbury commented that children do not see the doctor for well visits; parents wait until the child is sick before visiting the doctor (and immunizations are free for children without insurance). ENROLLMENT: Dr. Pillsbury thought that CHIP was first established for children whose parents’ employer did not offer child health insurance. Even if the employer offers this insurance, it is often too expensive. Paul Hughes questioned whether there is a waiting period for CHIP. Big changes are forthcoming for this program, he noted. Paul also referenced the “crowd out” effect, whereby employers such as Wal-Mart, offer insurance to their employees, and hand out applications for CHIP as a solution to dealing with children’s health insurance coverage. George asked how the average person would be able to navigate CHIP enrollment. Rosanne noted this was a good point. She stated that CHIP eligibility is determined by the Division of Social Services (DSS). 12/20/07 6 of 13 DHSS MCAC Meeting Minutes
TOPIC FOR DISCUSSION DISCUSSION / ISSUE ACTIONS FOLLOW-UP RESPONSIBILITY There is an online application and a screening tool. Brandi Niezgoda and Yrene both asked if the poor or disadvantaged would have access to the Internet. Cindy Denemark reminded the Committee that the paper application is only one page. PREMIUMS: George understood why parents making $41,000 are on the cusp of bouncing their child in, and Old Business: out of CHIP. Sheila Nutter stated that CHIP premiums Medicaid Overview are $10-$25 per household, per month. If a family is in (continued) dire straights, they may be unable to pay this amount. A by Harry Hill family may now want to pay for preventative/well care when a child is visibly healthy. Sheila stated that many children leave the program due to lack of premium payment. Efforts in the past have included waiving premiums, for six months. This did result in a higher number of children staying in the program. Premiums are not a federal requirement. However, without a premium payment, it becomes difficult to track clients when they leave the state. Paula suggested a slight buy-in. Yrene suggested a deductible instead of a premium. Dr. Pillsbury responded that providers often end up paying the deductible. Richard asked what the State would you loose if there were no premiums. Paula surmised that the State would need to recoup the cost of the premium plus account for a significant increase in the participating population. Richard thought the elimination of premiums would solve two issues: 1.) the issue of trying to increase the 5,000 clients participating at any given time, and 2.) remove the barrier of cost for enrolling a child. Paula estimated the cost to the State for eliminating premiums to be $25 multiplied by 12 months, multiplied by roughly 10,000 clients (for a total of $3 million). THOUGHTS FOR THE FUTURE: Paula asked if anyone had seen results from the (Insurance Commissioner) Matt Denn outreach effort. Sheila 12/20/07 7 of 13 DHSS MCAC Meeting Minutes
TOPIC FOR DISCUSSION DISCUSSION / ISSUE ACTIONS FOLLOW-UP RESPONSIBILITY responded that Matt Denn worked with DMMA for CHIP causes and produced a 1-page flyer, but no enrollment changes are discernable. Richard inquired about the maximum age of eligibility to which Rosanne responded eighteen. Richard then inquired about potential federal legislation to change the age. Harry responded that no federal legislation is proposed to change the age limit. Dr. Pillsbury stated that the number of employers who Old Business: offer family health coverage are in the minority. If these Medicaid Overview select employers do offer coverage, it is expensive (continued) ($600-700 per month). George asked how the by Harry Hill premiums are collected. Sheila responded that EDS collects premiums by working with Walgreen’s/Happy Harry’s, collecting monthly invoices, and billing credit cards. George suggested automatic withdrawal for CHIP from the parents’ paycheck (authorization to do so on behalf of the employee is all that is required). Many companies are already familiar with practices as such. Harry responded that this proposal might alleviate the problem of children bouncing in and out of the program. Yrene still expressed concerns with the escalating cost of living (e.g. the price of gas). George expanded on his initial proposal: premiums could be reduced (as some administrative management of the program would shift to employers). Sheila reminded the Committee that premiums are based on income (families at 110% of the poverty limit pay $10 per month, families at 199% of the poverty limit pay $25 per month). George noted that with the premium deducted from an employee’s paycheck the family will start getting used to living on less. Troubles still lie for those families making close to $41,000 as an annual raise of 2% to 3% would eliminate their participation in the program. Touching on an earlier point, Wendy noted that CHIP premium payments via credit cards come at a detriment to the parent with potential accrued interest on their card. Yrene asked if 12/20/07 8 of 13 DHSS MCAC Meeting Minutes
TOPIC FOR DISCUSSION DISCUSSION / ISSUE ACTIONS FOLLOW-UP RESPONSIBILITY there was ever a small focus group study relating to CHIP premiums. Rosanne and Dr. Pillsbury both responded, yes, but a long time ago. Rosanne detailed that the State received $500,000 in grant money to review premiums and create brochures in the past. Yrene asked if we could try to obtain grant money again. Employers would also benefit in knowing when a client moves out of the state. Richard inquired how the group Old Business: could move this issue along. Harry responded that the Medicaid Overview Committee should wait for now, as the immediate future (continued) holds many changes for CHIP. Harry noted that both by Harry Hill Lieutenant Governor Carney and Secretary Meconi have focused on this issue. Richard stated that he was in favor of $1 premiums (to be charged for the reason of tracking clients). Dr. Brazen noted that George’s idea of the premium being deducted from the paycheck is difficult because a lot of the uninsured are self-employed (i.e., electricians, plumbers). Dr. Pillsbury stated that the individuals must fill out required paperwork with the state now, and this would simply be another form. Richard asked about the timing of federal legislation. Harry anticipated hearing some discussion on this issue by Per Richard’s request, Harry Hill December 14, 2007. Paula reminded the Committee of provide a list of DMMA all previous delays. A decision was supposed to be accomplishments in 2007 made back in September 2007. Yrene heard discussion of a Presidential veto on the issue. Harry detailed the Division’s accomplishments in the past year: 1. DRA – Required changes were completed which included specialty Long Term Care modifications; 2. Managed Care Organization (MCO) Bids – The managed care bid process saved the State of Delaware approximately $10 million due to competition and offered more options for clients; 3. New Eligibility Unit Location – DMMA received funding for a Long Term Care eligibility unit in 12/20/07 9 of 13 DHSS MCAC Meeting Minutes
TOPIC FOR DISCUSSION DISCUSSION / ISSUE ACTIONS FOLLOW-UP RESPONSIBILITY Smyrna, Delaware with seven new employees; 4. National Provider Identifier (NPI) – Delaware was the first state in the country to complete this task due to the dedicated work of EDS and DMMA staff; 5. Part D implementation – Delaware implemented changes and was ranked #1 in the country for effectiveness; 6. Tamper-resistant prescription pads – DMMA Old Business: faced implementation challenges and questions, Medicaid Overview participated in town meetings, supported a soft (continued) start and did extensive research, received a by Harry Hill positive editorial in the Delaware News Journal; and 7. The Delaware Information Network (DHIN) – Health record databases have been established, ensuring an easier implementation for E- prescribing. Wendy and Dr. Brazen have spent a lot of time on telemedicine. Telemedicine, though not a Medicaid covered service, would be useful to treat the prison population. Richard asked for an executive summary on the issue. Richard also asked about using this in nursing homes. Dr. Pillsbury noted that the development of this issue has progressed so far as to establish billing codes. CMS now supports billing codes when a doctor consults via telephone, email, or online. Wendy noted that this technology includes robots and various equipment, and would even work well for psychiatrists. Rosanne Dr. Brazen suggested building on current infrastructure, as some providers already have compatible technology. Dr. Pillsbury would like follow up regarding newborns Follow up: If a parent is who do not yet have an assigned pediatrician. For the working and has health Harry/Rosanne initial months of the MCO transition, the managed care insurance, when is the child companies were good about paying out-of-network eligible for CHIP? providers. Now the MCOs will pay them for the birth, but Follow up on Dr. 12/20/07 10 of 13 DHSS MCAC Meeting Minutes
TOPIC FOR DISCUSSION DISCUSSION / ISSUE ACTIONS FOLLOW-UP RESPONSIBILITY will not pay for follow-up care provided after their release Pillsbury’s 30-day gap from the hospital. When the baby is born, they are concern. covered on the mother’s plan. The mother has 90 days to move the baby to another plan. Yrene stated that this transition should be seamless. DMMA will follow up.
New Business: Unison Rosanne expressed her excitement in having two Implementation Update by MCOs for healthy market competition. Harry Hill/Rosanne Richard inquired about representatives from Unison Mahaney and Delaware Physicians Care (DPCI) making a presentation to the Committee. Harry stated that this would be possible, but Richard decided against the idea.
12/20/07 11 of 13 DHSS MCAC Meeting Minutes
TOPIC FOR DISCUSSION DISCUSSION / ISSUE ACTIONS FOLLOW-UP RESPONSIBILITY
New Business: Jim Wilton noted the August and September 2007 Review of Quarterly Quality Quality Initiatives Improvement Taskforce meetings (QII) Assurance Report went well and were well-attended. A quality by Jim Wilton management strategy was developed. In the July meeting, DMMA presented the quality Research medical home Paul grant strategy which CMS used in their best practices. Dr. Pillsbury inquired about a medical home grant. Yrene stated that you want to be in the home. Dr. Pillsbury noted she heard of this in September at an American College of Physicians meeting. Dr. Pillsbury noted the CMS grant would chose 50 to 100 practices from around the country (rural to inner city) for the paid model study. Dr. Pillsbury noted that the CMS representatives noted this was limited to Medicare. Paul said nothing was sent to states. No members of the Committee were aware of this grant. In September, Unison presented their quality strategy including discussion of disease management, high-risk pregnancies, and diabetes management. Jim noted that DMMA’s actions drive the MCOs as we require certain measureables (which DMMA is also working to refine). Now that two MCOs are on board, we Per Richard’s request, have better cumulative data with both plans. present results of the MCO Jim DMMA is working on an MCO satisfaction survey. satisfaction surveys DMMA is upgrading case management software in January 2008, to the web-based Atlantes system. This will allow staff a better opportunity for case 12/20/07 12 of 13 DHSS MCAC Meeting Minutes
management. Miscellaneous:
The meeting was adjourned at 10:35 AM. Each member must let Mollie Daughtrey know IMPORTANT NOTES: if they will attend the March 12, 2008 meeting ([email protected] or 302-255- 9658). DMMA requests an accurate head count for preparation of the room and all materials.
Respectfully submitted,
Mollie Daughtrey December 20, 2007 __ Richard Cherrin Recorder Date approved Chairperson
12/20/07 13 of 13