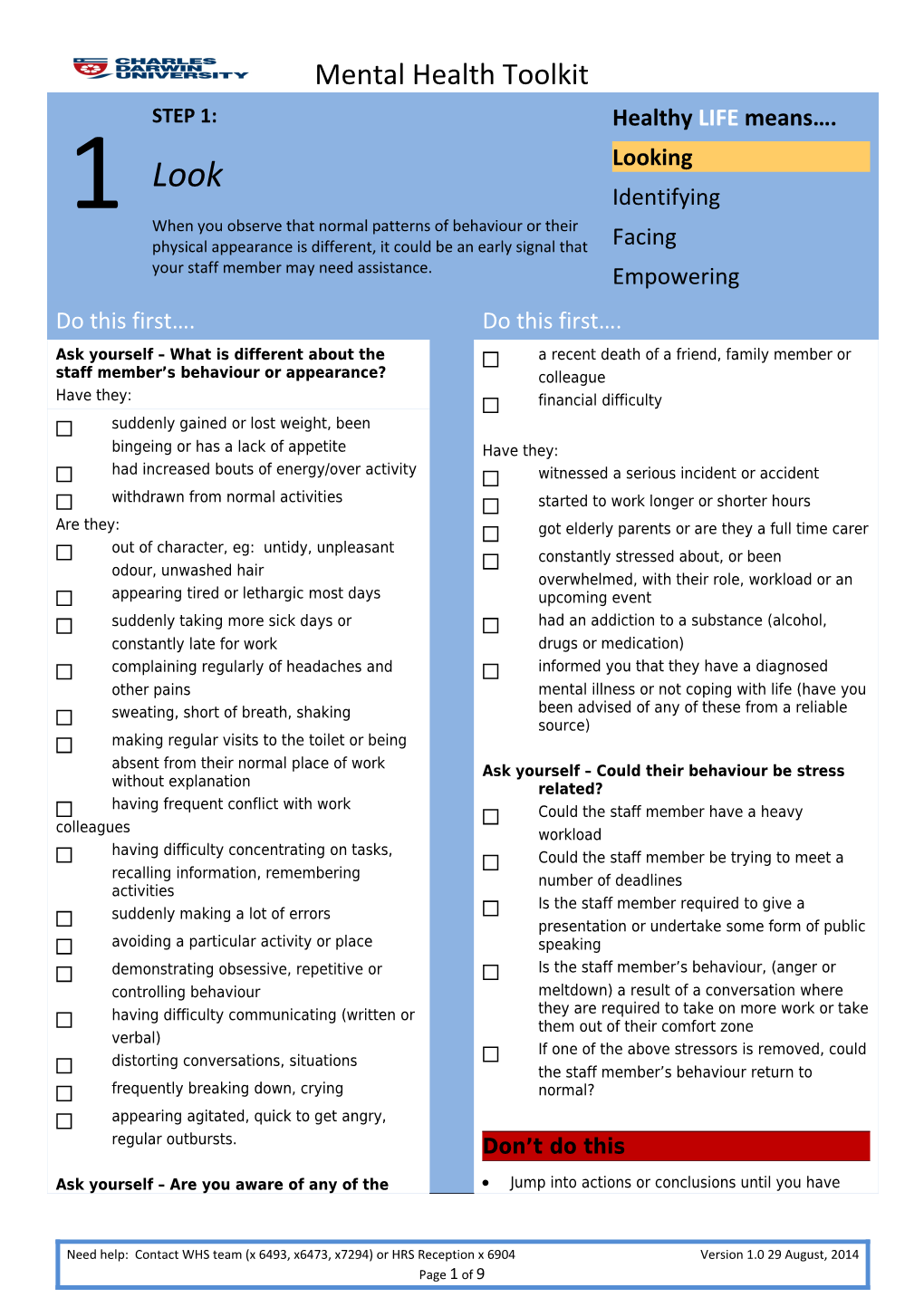
Mental Health Toolkit STEP 1: Healthy LIFE means…. Look Looking Identifying 1 When you observe that normal patterns of behaviour or their physical appearance is different, it could be an early signal that Facing your staff member may need assistance. Empowering Do this first…. Do this first…. Ask yourself – What is different about the a recent death of a friend, family member or staff member’s behaviour or appearance? colleague Have they: financial difficulty suddenly gained or lost weight, been bingeing or has a lack of appetite Have they: had increased bouts of energy/over activity witnessed a serious incident or accident withdrawn from normal activities started to work longer or shorter hours Are they: got elderly parents or are they a full time carer out of character, eg: untidy, unpleasant constantly stressed about, or been odour, unwashed hair overwhelmed, with their role, workload or an appearing tired or lethargic most days upcoming event suddenly taking more sick days or had an addiction to a substance (alcohol, constantly late for work drugs or medication) complaining regularly of headaches and informed you that they have a diagnosed other pains mental illness or not coping with life (have you sweating, short of breath, shaking been advised of any of these from a reliable source) making regular visits to the toilet or being absent from their normal place of work Ask yourself – Could their behaviour be stress without explanation related? having frequent conflict with work Could the staff member have a heavy colleagues workload having difficulty concentrating on tasks, Could the staff member be trying to meet a recalling information, remembering number of deadlines activities Is the staff member required to give a suddenly making a lot of errors presentation or undertake some form of public avoiding a particular activity or place speaking demonstrating obsessive, repetitive or Is the staff member’s behaviour, (anger or controlling behaviour meltdown) a result of a conversation where having difficulty communicating (written or they are required to take on more work or take them out of their comfort zone verbal) If one of the above stressors is removed, could distorting conversations, situations the staff member’s behaviour return to frequently breaking down, crying normal? appearing agitated, quick to get angry, regular outbursts. Don’t do this
Ask yourself – Are you aware of any of the Jump into actions or conclusions until you have
Need help: Contact WHS team (x 6493, x6473, x7294) or HRS Reception x 6904 Version 1.0 29 August, 2014 Page 1 of 9 Mental Health Toolkit following inside or outside of work? gathered the facts Has there been: Make assumptions about the staff member and recent family or workplace conflict then discuss this assumption with other staff or work colleagues recent divorce or separation Treat the person differently or make an example of involvement in a serious incident or them in front of others accident (recently or in the past) Assume that the problem or their uncharacteristic behaviour will go away
STEP 2: Healthy LIFE means…. Looking Identify Identifying 2 Gather the facts: It is often difficult to distinguish normal Facing mental health from mental illness because there is no simple test to show you. Gather information to help you to make an Empowering informed decision. Do this first…. Do this first…. Assess the information you have about the have you inadvertently contributed to the staff member:
Need help: Contact WHS team (x 6493, x6473, x7294) or HRS Reception x 6904 Version 1.0 29 August, 2014 Page 2 of 9 Mental Health Toolkit Check how many of the boxes you have problem ticked in Step 1 and the issues that they do you have the skills to manage the situation raise. or do you require additional advice (see Start documenting and collating a contacts in footer below). chronological record on the Notes page. Ensure your notes are saved/held in a Identify if the University has other policies and secure location processes that need to be considered: Identify if there are other indicators which have you checked the HRS website to identify may highlight that there are issues: what policies and procedures relate to the issues identified and that could also provide Increased or high numbers of sick you with assistance/guidance (eg: Enterprise leave reports Agreement, Performance Management, Injury formal complaints Management, non-work rehabilitation) feedback from clients or colleagues Does the policy/process require you to inform other Managers or HRS? specific incident reports
Other: Be satisfied before you take the next Other: step(step 3) that you have identified the issues and have the facts to back it up
Ask yourself: Is what you are identifying above repeated Don’t do this patterns of behaviour? Dismiss the fact that they: may be afraid that their disability will provoke Have you tried other strategies? unnecessary concern and affect job opportunity may not have come to terms with their mental Could you change/modify their behaviour by: illness altering their work environment may have been discriminated against in the past increasing predictability and scheduling, ie: may be afraid that they will lose their job. routine increasing opportunities for choice, Procrastinate and avoid taking the next step. flexibility and control adapting and/or modifying workload acknowledging positive behaviour minimising triggers which could lead to stress related behaviours Ask yourself: do you have a clear and consistent approach with all your staff and haven’t developed any biases toward this staff member due to an event in the past have you created a work environment that may create or exacerbate mental health problems
Need help: Contact WHS team (x 6493, x6473, x7294) or HRS Reception x 6904 Version 1.0 29 August, 2014 Page 3 of 9 Mental Health Toolkit STEP 3: Healthy LIFE means…. Face Looking Identifying 3 A conversation can be difficult, but needs to occur to help the Facing staff member and help you at work. Empowering Do this first…. Do this first…. Continue documenting and collating records Continuing the Conversation on the Notes page Guide the conversation with questions that Have you reviewed your findings and considered an appropriate setting: help explore – you want the person to do most of the talking – silence is not necessarily bad. How will you inform the staff member of Listen without judgement. why you are having the meeting: phone call Ask open-ended questions. face to face If the staff member appears uncomfortable or unwilling to talk: Have you planned for different scenarios, Encourage conversation along with examples eg: of the behaviour that has changed in recent performance management times, eg: does the staff member want “How has that made you feel” support at the meeting “What do you think may have caused this the staff person does not want to reaction” meet Are you getting any assistance, support from others, medical assistance” the staff member gets emotional Give the staff member time to reply – Have you allowed enough time? Allow remember: silence is not necessarily bad. more than less. Maybe have the meeting late morning Acknowledge there is an issue Record time: Don’t rush to solve problems, but let the staff Is the setting in a private quiet space and member know solutions are available when at a time that suits the staff member. they are ready to start exploring them Review both your and the staff member’s Paraphrase or reflect back to the staff member commitments the main concerns to show you understand Record location: Use clarifying questions if there is something missing or wrong, eg: “It seems to me that Initiate the Meeting you’re saying…..” Have all of your information ready “What have I missed…?” Remember – open posture, good eye Reassure the staff member and ask them what contact and body language is important they would like to do from here. Explain why you are having the meeting – Don’t do this you are concerned about them – their physical or behavioural changes, using Schedule too little time to have the conversation, examples, eg: or schedule in-between back-to-back meetings “I’m concerned about you. You are a very Try to diagnose a medical condition competent worker but I have noticed lately Agree with thoughts or beliefs that are out of that you are having trouble with……” control “You don’t seem yourself lately and I’m Speak down to the staff member or use derogatory
Need help: Contact WHS team (x 6493, x6473, x7294) or HRS Reception x 6904 Version 1.0 29 August, 2014 Page 4 of 9 Mental Health Toolkit wondering if you are OK. Is there anything terms, eg: crazy or schizo that is contributing…” Don’t treat the staff member as an invalid “I don’t want to intrude on your privacy, Don’t assume that you will be able to “cure” the but something is impacting on you at work staff member of their mental illness and I’m concerned. I have a duty of care to Don’t assume that a single conversation will be all you and others. I want you to know help is that is required. available.”
STEP 4: Healthy LIFE means…. Empower Looking Identifying 4 Empowering will enable open communication; improve trust; Facing encourage the person to take responsibility and control; and provide a positive work environment and clear pathway. Empowering Do this first…. Do this first….
Need help: Contact WHS team (x 6493, x6473, x7294) or HRS Reception x 6904 Version 1.0 29 August, 2014 Page 5 of 9 Mental Health Toolkit Determine the best path forward based on information you have collected and through Option 4 – Crisis care discussion with the staff member in Step 3. Choose: Immediate intervention Option 1 – Agree on reasonable The person may have reached the point where a staged and planned approach is no longer an option. adjustments If you think that they are an immediate risk to Option 2 – Person to self-manage with themselves or others then you will need to determine monitoring who to contact: Option 3 – Commence performance Violent, aggressive behaviour: Security management 7777and/or Police Option 4 – Crisis care: referral and Incoherent/irrational – Contact someone they immediate intervention trust – a family member or friend to ensure that they are accompanied and supported. If Option 5 – Workers Compensation (person their behaviour becomes uncontrollable, is claiming that their illness is caused by contact Security on 7777 and/or Police. Stay work) with the person until assistance arrives. Continue documenting and collating records on the Physical symptoms that indicate emergency Notes page medical treatment is required (eg: chest pain). Option 1 – Reasonable adjustments Ring 000 if necessary. Threat of suicide – Express care and concern Identify changes to a job which can be and do not leave them. Contact Lifeline on made to enable the person to perform 13 11 14 or ring 000 if necessary. Contact their duties more effectively in the someone they trust – a family member or workplace while still meeting the inherent friend. Do not take responsibility on your own. requirements of the job. Refer to examples on the following pages. Option 5 – Workers compensation Option 2 – Self manage and monitor If the person believes their condition is related to work Ensure the person knows that their and wishes to lodge a Workers Compensation claim, behaviour needs to change advise them to contact the Injury Management Consultant on extension 6493 or access the WHS Allow the person to self-manage and rectify website for further information. their behaviour without workplace intervention Encourage the person to seek other Don’t do this assistance. This might include: Make assumptions about the person’s ability to do speaking to their GP, or if they don’t their job based solely on the fact that they have a have one, providing information about mental illness EASA Agree to something that is not substantive or Speaking to a counsellor reasonable from an operational perspective Clarify expectations around performance Wait until the end of an agreed timeframe to and that if work issues continue, there may provide feedback regarding progress. This needs be no choice but to commence the to be an ongoing conversation performance management process (Option Forget to gain assistance for yourself in managing 3) the situation Agree on times to catch up Forget to remind the person that they can have a support person with any of the options Maintain contact. Do nothing. Option 3 – Performance management Seek advice from Employee Relations Follow the Employee Relations advice
Need help: Contact WHS team (x 6493, x6473, x7294) or HRS Reception x 6904 Version 1.0 29 August, 2014 Page 6 of 9 Mental Health Toolkit STEP 4: Healthy LIFE means…. Empower Looking Identifying 4 Empowering will enable open communication; improve trust; Facing encourage the person to take responsibility and control; and provide a positive work environment and clear pathway. Empowering
Reasonable adjustments Reasonable adjustments Inherent Requirements plan the use of annual or sick leave (with Identify and record the inherent the support of a medical certificate) to requirements of the job including key temporarily reduce hours or allow medical operational needs of the area appointment attendance Ensure that the person understands the change usual shift patterns to longer core requirements of their job and explore periods of day / afternoon / night shifts to ways that they can meet these allow for changing schedules of medication which can be difficult support the use of a flexible work Reasonable Adjustments arrangement to allow the person to As the person’s supervisor, you are best placed and gradually transition back to work should feel empowered to provide support and following a period of time off (contact monitoring on a day to day basis. However, if it is Injury Management Consultant on identified during the process that reasonable extension 6493 for assistance with this) adjustments will (whether temporary or permanent): change the inherent requirements of the Concentrating on – or remembering tasks person’s job; or Provide the person with daily “To do” lists and include changes that will exceed a three schedule regular breaks to accommodate a month period; or reduced concentration span require any advice or assistance. Write work instructions down rather than Contact the Injury Management Consultant on verbalising what to do extension 6493 who will work with you to develop a Break down job tasks into small steps and use formal Return to Work (RTW) plan. prompts for each step in order to assist the The types of adjustments will depend on the person to refocus and continue with tasks if individual and their symptoms. Encourage the they forget what comes next, eg: step tasks person to think about their own solutions as well as out in an email or develop a checklist offering some of your own. These can include: Allow extra time to complete tasks or swap increasing the frequency of one-on-one complex tasks until the person gains meetings to prioritise tasks and review confidence. Enable rotation between tasks deadlines Discuss progress at agreed time-frames review how tasks are allocated, for example: Use colour coding or other methods to help ensure that a person who is finding the prioritise tasks pressure of meetings very difficult, Minimise potential distractions by partitioning arranges their diary to allow off the workspace or having a workstation appropriate time to prepare away from other colleagues. consider whether a temporary change to some duties is appropriate and can Avoiding social interactions / colleagues be supported (eg: reduced contact with
Need help: Contact WHS team (x 6493, x6473, x7294) or HRS Reception x 6904 Version 1.0 29 August, 2014 Page 7 of 9 Mental Health Toolkit the public/students Identify what areas of the role/interactions the appoint a buddy or mentor – someone person is having difficulty with on a similar grade and outside the Swap or minimise those tasks/interactions, eg: usual management structure where the person is required to regularly meet Offering flexible work arrangements: with colleagues/others – can they provide a summary in an email or report investigate variable start/finish times Position the person in an area where they feel and/or structure work and work hours to match the person’s most productive more comfortable or can work alone. time of day
STEP 4: Healthy LIFE means…. Empower Looking Identifying 4 Empowering will enable open communication; improve trust; Facing encourage the person to take responsibility and control; and provide a positive work environment and clear pathway. Empowering
Need help: Contact WHS team (x 6493, x6473, x7294) or HRS Reception x 6904 Version 1.0 29 August, 2014 Page 8 of 9 Mental Health Toolkit Reasonable adjustments Reasonable adjustments What if they can’t be met Where the inherent requirements of the job When planned arrangements/reasonable are not being met and reasonable adjustments adjustments aren’t being met, it may be for a are no longer an option then seek advice from variety of reasons: HRS advisors. Go back to Step 2 and identify and document the issues. If there is a formal agreed arrangement or documented RTW Remember the inherent requirements plan, what hasn’t been met: Where a person is unable to perform the inherent has the person been compliant requirements of their position and no adjustment can reasonably be made to allow them to perform the core was support offered as outlined, were work requirements, then it may be necessary to the goals and planned arrangements explore alternative work options. realistic, eg: an agreement was It is not unlawful discrimination to terminate a made to start at 10:00am but person person’s employment where they cannot perform the is having difficulty waking up in time role after reasonable adjustments have been made. because of medication side effects Assistance should be sought from the Employee Consider if there are any other reasonable Relations team to ensure obligations under the strategies which would address the issues Enterprise Agreement and legal obligations are met identified and to provide you with guidance on the next steps. Go to Step 3 and plan to have the conversation with the person and follow the What can you say to other staff prompts. This may be in consultation with When you make changes to a person’s working the Injury Management Consultant where arrangements (temporary or permanent) make sure required you inform other staff who need to know about it. Identify what the person considers that This does not mean that you need to tell other staff they need in order to resolve the issues about the person’s health condition – in fact, this Ensure that there is a balance between the would be breaching confidentiality. You just need to ensure they know about the arrangement, so that they options put forward and what is appropriate do not prevent reasonable adjustments from working for the Team/area in practice; eg: Acknowledge and agree on a plan of action “…… will be working part-time for the next (eg: a review by the doctor to determine three months. They will continue to perform capacity to complete duties, a period of the functions of their role, so please continue leave, a revised RTW plan) to forward accounts for payment. However Allow them some time to consider the student enquiries should be directed to the options if required front counter. If you have any questions regarding this arrangement, please come and Document the agreed actions and provide a see me.” copy to the person (email or hard copy) Consult with the person regarding any formal Where there is a disagreement in a course of action communications to staff – you must have evidence of between the person and yourself, don’t let it drag their consent. on. A problem won’t necessarily go away if you Remember that the person is free to disclose as much don’t talk about it and you may be making things or as little information as they like to colleagues about worse in the longer term. their health condition. Consider engaging a third party to facilitate the process. This allows for professional and independent advice to both the supervisor and the person. Contact the Injury Management Consultant who will facilitate this process and/or provide advice.
Reproduced with kind permission from The University of Adelaide, “HSW Mental Health Toolkit to assist supervisors”
Need help: Contact WHS team (x 6493, x6473, x7294) or HRS Reception x 6904 Version 1.0 29 August, 2014 Page 9 of 9