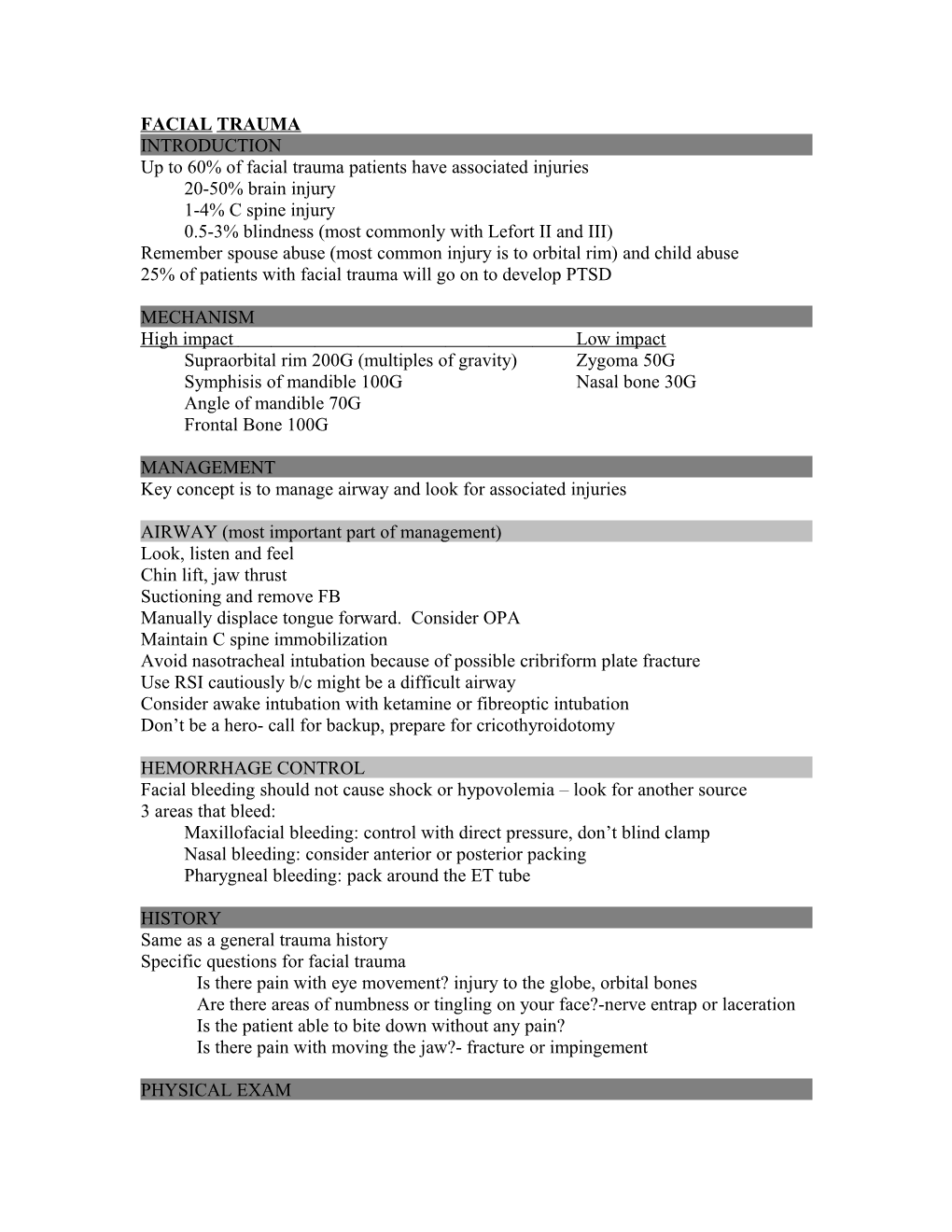
FACIAL TRAUMA INTRODUCTION Up to 60% of facial trauma patients have associated injuries 20-50% brain injury 1-4% C spine injury 0.5-3% blindness (most commonly with Lefort II and III) Remember spouse abuse (most common injury is to orbital rim) and child abuse 25% of patients with facial trauma will go on to develop PTSD
MECHANISM High impact Low impact Supraorbital rim 200G (multiples of gravity) Zygoma 50G Symphisis of mandible 100G Nasal bone 30G Angle of mandible 70G Frontal Bone 100G
MANAGEMENT Key concept is to manage airway and look for associated injuries
AIRWAY (most important part of management) Look, listen and feel Chin lift, jaw thrust Suctioning and remove FB Manually displace tongue forward. Consider OPA Maintain C spine immobilization Avoid nasotracheal intubation because of possible cribriform plate fracture Use RSI cautiously b/c might be a difficult airway Consider awake intubation with ketamine or fibreoptic intubation Don’t be a hero- call for backup, prepare for cricothyroidotomy
HEMORRHAGE CONTROL Facial bleeding should not cause shock or hypovolemia – look for another source 3 areas that bleed: Maxillofacial bleeding: control with direct pressure, don’t blind clamp Nasal bleeding: consider anterior or posterior packing Pharygneal bleeding: pack around the ET tube
HISTORY Same as a general trauma history Specific questions for facial trauma Is there pain with eye movement? injury to the globe, orbital bones Are there areas of numbness or tingling on your face?-nerve entrap or laceration Is the patient able to bite down without any pain? Is there pain with moving the jaw?- fracture or impingement
PHYSICAL EXAM Bird’s eye view and Worm’s eye view Palpate supra and infraorbital rims Globe: enopthalmus or exothalmus, abnormal shape of pupil, subconjunctival hemorrhage, visual acuity Check cornea for abrasions, anterior chamber for hyphema Fundoscopy to assess retina Lids- look for lac. Injuries to medial 1/3 may involve lacrimal apparatus Palpate the medial orbit area to r/o naso ethmoidal orbital fx. (Q tip inside the nose directed towards the medial canthus, place your finger outside the medial canthus. If the bone moves NEO #.) Palpate zygomaticofrontal suture, zygomaticotemporal suture and arch Palpate nose: asymmetry, widening of nasal bridge (telecanthus- normal intercathi distance is 32-34mm), septal hematoma, blood, deformity, crepitus, subq air and CSF – halo sign on paper towel Palpate maxilla for facial instability/mobility Palpate mandible for tenderness, swelling and step off Cranial nerve exam- most important- EOM and facial nerve Intraoral exam: Inspect the teeth for malocclusions, bleeding and step-off. Must account for all teeth. Manipulate each tooth, check for gum lacerations, Tongue blade test. (twist tongue blade while pt bites down. If jaw broke, pt will open mouth) 95% sens and 65% spec. Palpate the mandible for deformities, step-offs, tender areas
RADIOLOGY Xrays are useful for assessment of: Bones, fluid-filled spaces, herniation of orbital contents, subQ air Basic Facial Series 1)Water’s: (occipitomental view): Single best xray, good screening view for maxillary #. 37o caudal to canthomeatal line- good to see superior and inferior orbital rims, nasal bones zygoma and maxilla 2) Caldwell view (PA or occipitofrontal view): 15o caudal to canthomeatal line - frontal sinus and supraorbital rim
3)Lateral view – anterior wall of frontal sinus and maxillary sinus views 4)Submentovertex view:occasionally done. Good for zygomatic arch
Jaw series: 1) PA, 2) lateral obliques, 3) Towne’s view and 4) panorex ( best view of mandible)
CT face Better than Xray; gold standard for facial fractures Indicated if # suspected on exam Can’t cooperate well for x-ray Penetrating injury
FRACTURE/DISLOCATIONS FRONTAL SINUS FRACTURES Palpate along frontal bone and supraorbital rim for deformity or subq air Associated with dural tears, intracranial injury and injury to orbital roof MUST evaluate posterior wall of sinus with CT Non displaced anterior wall: abx, should still consult neursurg for outpatient followup Depressed anterior wall or posterior wall fractures- assume to have assoc dural tear Admit Neurosurg consultation Abx and tetanus Complications of posterior wall fracture: mucocele, CSF leak, epidural empyema, meningitis, associated orbital fracture
MAXILLARY FRACTURES- LeFort fractures High force mechanism, consider associated injuries LeFort Classification (rarely isolated, most commonly occur in combination) LeFort I - maxilla at level of nasal fossa Maxilla mobile, nasal bridge stable Malocclusion of teeth LeFort II - maxilla, nasal bones, medial aspect of orbits (pyramidal dysfn) nose and upper jaw mobile on exam LeFort III - maxilla, zygoma, nasal bones, ethmoid, vomer, cranial base (craniofacial dysfunction) dish face deformity ( elongation of eyes with flat sunken face) At risk for airway obstruction Management : plastics consult for OR Airway is most important: ETT –> cric Rhinorrhea uncommon with I, more common with LF II/III admit for abx prophylaxis (not proven) and elevation of head of bed 40-60% if C spine cleared
ZYGOMATIC FRACTURES 2nd MC facial # Two types: arch and tripod Arch fracture Pain over arch +/- bony deformity Pain with opening mouth or impingement of temporalis muscle/coronoid process
Look for flattened cheek Submental view (bucket handle view) Management: refer for outpt ORIF
Tripod fracture Fracture through 1) arch (or zygomaticotemporal suture) 2) zygomaticofrontal suture 3) infraorbital rim and floor Presents with flat cheek, infraorbital nerve damage (anesthesia), diplopia, change in consensual gaze, step defect, globe injury Water’s is best Xray but you should CT face Refer for ORIF (may be outpt if non displaced and without eye involvement) NASO-ETHMOIDAL-ORBITAL FRACTURE Suspect if trauma to nose or medial orbit Pain with EOM Associated lacriminal disruption and dural tears Look for flat or saddle shaped nasal bridge, telecanthus, epistaxis or CSF rhinorhea Q tip test Needs CT Consult plastics Abx?
ORBITAL BLOWOUT FRACTURES Can be isolated or combined (commonly with zygomatic #) Blow out fracture: force transmitted to thin orbital floor (or medially) Direct globe pressure from object < 5 cm radius. Also from direct blow to infraorbital rim that causes orbital floor to buckle Possible herniation of fat or muscle into maxillary sinus (tear drop sign) Presentation Step off of infraorbital rim Diplopia due to muscle/fat entrapment, intramuscular hematoma, V2 neuropraxia True entrapment will be vagal, vomiting, refuse to move eye Enopthalmos (sunken eye) and limited EOM (limited upward gaze) Infraorbital anesthesia Orbital emphysema Should have a CT but on xray look for Tear drop sign (herniated fat into maxillary sinus) Open bomb bay sign (bony fragments protrude into maxillary sinus) Air fluid level in sinus Management Refer to plastics and ophthalmology Tetanus and abx Avoid valsalva Decongestant for 3 days Most observe for 10 - 14d then decide on OR based on enopthalmos/diplopia Orbital emphysema May present with visual acuity loss b/c of pressure on orbit causing central retinal artery occlusion Emergent decompression with needle or canthotomy w/ cantholysis
NASAL FRACTURES MC facial # - 3 kinds: nondisplaced, depressed and laterally displaced Ask pt if they have broken nose before, how is your breathing, does it look normal Crepitus, deformity, swelling, tenderness, edema Epistaxis usually mild but can be heavy Clinical dx: NO Xrays although can sometimes see on facial lateral xray Management Pack bleeding R/o septal hematoma: drain, pack, ENT follow up if present Immediate reduction: can do if full edema not yet dev’t (within 3 hours) Delayed reduction: if already dev full edema- refer for reduction in 6-10 days If you choose to reduce- intranasal cocaine, bilateral infraorbital nerve blocks and bilateral external nasal nerve. Use boies elevator or scalpel handle to elevate depressed bone and forceps to reduce deviated septum Peds: do not reduce, refer for evaluation in 4/7 Consider assoc injuries: Bridge of nose: nasoethmoid # -----> rhinorrhea, CT face, abx, neurosurg consult
MANDIBULAR FRACTURES Mandibular pain/tenderness, malocclusion, separation of teeth, periauricular pain Trauma + malocclusion = mandibular # Ecchymosis on floor of mouth very suggestive Multiple locations in > 50%; may be distant from site of trauma Locations Condylar 35% Body 21% Angle 20% Symphysis 14% Ramus 3% Coronoid 3% Panorex view best CT may be needed for condylar # Non-displaced: soft diet, analgesic, orif in 1-2 days Displaced and open #’s are closed sooner Antibiotics if open: usually penicillin
MANDIBULAR DISLOCATIONS Risks Weak TMJ Shallow articular eminence Overstretched joint capsule Neuromuscular disorders Trauma to jaw Excessive mouth opening Mostly anterior but posterior (direct blow to chin), lateral (associated with fracture) and superior can occur Mostly bilateral For anterior: jaw will jut out forward and will deviate away from dislocated side if unilateral Muscles of mastication spasm preventing spontaneous reduction X-ray if mechanism suggests potential #
To reduce: Thumbs or fingers in buccal sulcus or wrapped in gauze on mandibular teeth Downward backward pressure with rotation so chin goes upward and angle of mandible goes backcward May be easier to reduce one side at a time D/C home with soft diet x 2wks and outpatient F/U with oral surgery WOUND MANAGEMENT Don’t forget tetanus May close facial lacerations up to 24hrs Indications for delayed primary closure Wound older than 24 hrs FB that can’t be removed Severe contamination can close early if thoroughly debride but if > 6 hours, should treat with abx for 4 days and then close Presence of # requiring further evaluation/therapy When to consult plastics? Uncomfortable w/ lac Underlying nerve injury Injury requiring OR Delayed primary closure Wound Management Avoid epi in ear, nose, tarsal plate of eyelid Regional blocks, LAT useful Vigorous scrubbing for abrasions to prevent traumatic tattooing Careful exploration for FB Copious, forceful irrigation Deep: 4-0, 5-0 vicryl Skin: 5-0, 6-0 prolene/ethilon No drsg, polysporin, remove 3-5d (minimizes scar) Indications for antibiotics in facial injuries Bite wounds Devascularization Through-and-through buccal mucosa Cartilage involvement (nose/ear) Extensive contamination
SPECIFIC INJURIES Always consider nerve blocks Lips Close vermillion border first Tongue Close big lacs and flaps, midline lacs, avulsions, nonlinear lacerations Oral cavity Refer if salivary ducts involved Ear Auricular nerve block Approximate cartilage with 5-0, 6-0 absorbable; Staph abx coverage b/c avascularity of cartilage is high risk for condritis Subperichondral hematoma: will develop “cauliflower” ear if not drained; aspirate and compressive dressing for 7d with close f/u and repeat aspiration prn Periorbital Refer to optho: lid margin and medial canthus lacs Through-and-through cheek Begin intraoral and work outwards Copious irrigateion after each layer closed Abx prophylaxis Eyelid Plastics for lid margin, canalicular, lacrimal 6-0 Ethilon for superficial lacs
Retro orbital hematoma -proptosis, decreased visual acuity, IOP > 40, afferent papillary defect Management: time is EYE therefore pt needs lateral canthontomy Lateral canthotomy steps: Local anesthesia and sedation Crimp skin downward from lateral eye with kellys to reduce bleeding x 1 minute Cut the skin (canthotomy) Lift inferior skin flap to identify tendon (tendon feels like guitar string) Cut the tendon (cantholysis) Goal IOP < 40 Repeat same steps for superior lateral canthal tendon