Hyperandrogenic States in Women: Pitfalls in Laboratory Diagnosis
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Dehydroepiandrosterone – Is the Fountain of Youth Drying Out?
Physiol. Res. 52: 397-407, 2003 MINIREVIEW Dehydroepiandrosterone – Is the Fountain of Youth Drying Out? P. CELEC 1,2, L. STÁRKA3 1Faculty of Medicine, 2Faculty of Natural Sciences, Comenius University, Bratislava, Slovakia and 3Institute of Endocrinology, Prague, Czech Republic Received September 15, 2002 Accepted October 7, 2002 Summary Dehydroepiandrosterone (DHEA) and its sulphate-bound form (DHEAS) are important steroids mainly of adrenal origin. Their physiological and pathophysiological functions are not yet fully identified, although a number of various possible features have been hypothesized. Most popular is the description of the “hormone of youth” as the long-term dynamics of DHEA levels are characterized by a sharp age-related decline in the late adulthood and later. Low levels of DHEA are, however, associated not only with the ageing process but also with diabetes mellitus, cardiovascular diseases and some neurological or immunological entities. In the past decade, a number of brief studies have concentrated on these relationships and also on the role of exogenous DHEA in health, disease and human well-being. This article tries to summarize some of the most important facts achieved recently. Key words Dehydroepiandrosterone • Intracrinology • Hormone replacement therapy • Steroids Introduction functions: 1) DHEA is an endogenous metabolite that cannot be patented so that pharmaceutical companies are In 1934 Butenandt and Dannenbaum isolated not interested in supporting research in this field. dehydroepiandrosterone (DHEA) from urine and in 1944 2) DHEA can be described as a “human molecule” Munson and colleagues identified its 3β-sulphate because other investigated species have much lower (DHEAS). Even now, nearly 70 years later, we still do concentrations. -

Sex Hormones Related Ocular Dryness in Breast Cancer Women
Journal of Clinical Medicine Review Sex Hormones Related Ocular Dryness in Breast Cancer Women Antonella Grasso 1, Antonio Di Zazzo 2,* , Giuseppe Giannaccare 3 , Jaemyoung Sung 4 , Takenori Inomata 4 , Kendrick Co Shih 5 , Alessandra Micera 6, Daniele Gaudenzi 2, Sara Spelta 2 , Maria Angela Romeo 7, Paolo Orsaria 1, Marco Coassin 2 and Vittorio Altomare 1 1 Breast Unit, University Campus Bio-Medico, 00128 Rome, Italy; [email protected] (A.G.); [email protected] (P.O.); [email protected] (V.A.) 2 Ophthalmology Operative Complex Unit, University Campus Bio-Medico, 00128 Rome, Italy; [email protected] (D.G.); [email protected] (S.S.); [email protected] (M.C.) 3 Department of Ophthalmology, University Magna Graecia of Catanzaro, 88100 Catanzaro, Italy; [email protected] 4 Department of Ophthalmology, School of Medicine, Juntendo University, 1130033 Tokyo, Japan; [email protected] (J.S.); [email protected] (T.I.) 5 Department of Ophthalmology, Li Ka Shing Faculty of Medicine, The University of Hong Kong, Hong Kong; [email protected] 6 Research and Development Laboratory for Biochemical, Molecular and Cellular Applications in Ophthalmological Sciences, IRCCS–Fondazione Bietti, 00198 Rome, Italy; [email protected] 7 School of Medicine, Humanitas University, 20089 Milan, Italy; [email protected] * Correspondence: [email protected]; Tel.: +39-06225418893; Fax: +39-9622541456 Abstract: Background: Dry eye syndrome (DES) is strictly connected to systemic and topical sex hor- mones. Breast cancer treatment, the subsequent hormonal therapy, the subsequent hyperandrogenism and the early sudden menopause, may be responsible for ocular surface system failure and its clinical Citation: Grasso, A.; Di Zazzo, A.; manifestation as dry eye disease. -
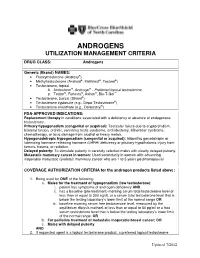
Androgens Utilization Management Criteria
ANDROGENS UTILIZATION MANAGEMENT CRITERIA DRUG CLASS: Androgens Generic (Brand) NAMES: • Fluoxymesterone (Androxy®) • Methyltestosterone (Android®, Methitest®, Testred®) • Testosterone, topical A. Androderm®, Androgel® - Preferred topical testosterone ® ® ® ™ B. Testim , Fortesta , Axiron , Bio-T-Gel • Testosterone, buccal (Striant®) • Testosterone cypionate (e.g., Depo-Testosterone®) • Testosterone enanthate (e.g., Delatestryl®) FDA-APPROVED INDICATIONS: Replacement therapy in conditions associated with a deficiency or absence of endogenous testosterone. Primary hypogonadism (congenital or acquired): Testicular failure due to cryptorchidism, bilateral torsion, orchitis, vanishing testis syndrome, orchidectomy, Klinefelter syndrome, chemotherapy, or toxic damage from alcohol or heavy metals. Hypogonadotropic hypogonadism (congenital or acquired): Idiopathic gonadotropin or luteinizing hormone-releasing hormone (LHRH) deficiency or pituitary-hypothalamic injury from tumors, trauma, or radiation. Delayed puberty: To stimulate puberty in carefully selected males with clearly delayed puberty. Metastatic mammary cancer in women: Used secondarily in women with advancing inoperable metastatic (skeletal) mammary cancer who are 1 to 5 years postmenopausal COVERAGE AUTHORIZATION CRITERIA for the androgen products listed above: 1. Being used for ONE of the following: a. Males for the treatment of hypogonadism (low testosterone): i. patient has symptoms of androgen deficiency AND ii. has a baseline (pre-treatment) morning serum total testosterone level of less than or equal to 300 ng/dL or a serum total testosterone level that is below the testing laboratory’s lower limit of the normal range OR iii. baseline morning serum free testosterone level, measured by the equilibrium dialysis method, of less than or equal to 50 pg/ml or a free serum testosterone level that is below the testing laboratory’s lower limit of the normal range, OR b. -

Serum Androgen Profiles in Women with Premature Ovarian Insufficiency: a Systematic Review and Meta-Analysis
Menopause: The Journal of The North American Menopause Society Vol. 26, No. 1, pp. 78-93 DOI: 10.1097/GME.0000000000001161 ß 2018 The Author(s). Published by Wolters Kluwer Health, Inc. on behalf of The North American Menopause Society. Serum androgen profiles in women with premature ovarian insufficiency: a systematic review and meta-analysis Midhun Soman, MS,1 Li-Cong Huang, MD,1 Wen-Hui Cai, MS,1 Jun-Bi Xu, MS,1 Jun-Yao Chen, MD,1 Ren-Ke He, MS,1 Heng-Chao Ruan, MS,1,2,3 Xiang-Rong Xu, MD,1,2,3 Zhi-Da Qian, MD,1,2,3,4 and Xiao-Ming Zhu, MD, PhD1,2,3 Abstract Objective: This meta-analysis aims to investigate serum androgen profiles (testosterone, dehydroepiandroster- one sulfate, androstenedione, and sex hormone-binding globulin) in women with premature ovarian failure and to establish if there is evidence of diminished androgen levels in these women. Methods: Various Internet sources of PubMed, Cochrane library, and Medline were searched systematically until February, 2018. Out of a pool of 2,461 studies, after applying the inclusion/exclusion criterion, 14, 8, 10, and 9 studies were chosen for testosterone, dehydroepiandrosterone sulfate, androstenedione, and sex hormone-binding globulin, respectively, for this meta-analysis. The effect measure was the standardized mean difference with 95% confidence interval (95% CI) in a random-effects model. Results: The testosterone concentrations in premature ovarian insufficiency were compared with fertile controls: stamdard mean difference (IV, random, 95% CI) À0.73 [À0.99, À0.46], P value < 0.05. The dehydroepiandrosterone sulfate concentrations in premature ovarian insufficiency compared to fertile controls: standard mean difference (IV, random, 95% CI) À0.65 [À0.92, À0.37], P value < 0.05. -

Health Risks Associated with Long-Term Finasteride and Dutasteride Use: It’S Time to Sound the Alarm
Review Article Health promotion, disease prevention, and lifestyle pISSN: 2287-4208 / eISSN: 2287-4690 World J Mens Health 2020 Jul 38(3): 323-337 https://doi.org/10.5534/wjmh.200012 Health Risks Associated with Long-Term Finasteride and Dutasteride Use: It’s Time to Sound the Alarm Abdulmaged M. Traish Department of Urology, Boston University School of Medicine, Boston, MA, USA 5α-dihydrotestosterone (5α-DHT) is the most potent natural androgen. 5α-DHT elicits a multitude of physiological actions, in a host of tissues, including prostate, seminal vesicles, hair follicles, skin, kidney, and lacrimal and meibomian glands. How- ever, the physiological role of 5α-DHT in human physiology, remains questionable and, at best, poorly appreciated. Recent emerging literature supports a role for 5α-DHT in the physiological function of liver, pancreatic β-cell function and survival, ocular function and prevention of dry eye disease and kidney physiological function. Thus, inhibition of 5α-reductases with finasteride or dutasteride to reduce 5α-DHT biosynthesis in the course of treatment of benign prostatic hyperplasia (BPH) or male pattern hair loss, known as androgenetic alopecia (AGA) my induces a novel form of tissue specific androgen deficien- cy and contributes to a host of pathophysiological conditions, that are yet to be fully recognized. Here, we advance the con- cept that blockade of 5α-reductases by finasteride or dutasteride in a mechanism-based, irreversible, inhabitation of 5α-DHT biosynthesis results in a novel state of androgen deficiency, independent of circulating testosterone levels. Finasteride and dutasteride are frequently prescribed for long-term treatment of lower urinary tract symptoms in men with BPH and in men with AGA. -

Reproductive DHEA-S
Reproductive DHEA-S Analyte Information - 1 - DHEA-S Introduction DHEA-S, DHEA sulfate or dehydroepiandrosterone sulfate, it is a metabolite of dehydroepiandrosterone (DHEA) resulting from the addition of a sulfate group. It is the sulfate form of aromatic C19 steroid with 10,13-dimethyl, 3-hydroxy group and 17-ketone. Its chemical name is 3β-hydroxy-5-androsten-17-one sulfate, its summary formula is C19H28O5S and its molecular weight (Mr) is 368.5 Da. The structural formula of DHEA-S is shown in (Fig.1). Fig.1: Structural formula of DHEA-S Other names used for DHEA-S include: Dehydroisoandrosterone sulfate, (3beta)-3- (sulfooxy), androst-5-en-17-one, 3beta-hydroxy-androst-5-en-17-one hydrogen sulfate, Prasterone sulfate and so on. As DHEA-S is very closely connected with DHEA, both hormones are mentioned together in the following text. Biosynthesis DHEA-S is the major C19 steroid and is a precursor in testosterone and estrogen biosynthesis. DHEA-S originates almost exclusively in the zona reticularis of the adrenal cortex (Fig.2). Some may be produced by the testes, none is produced by the ovaries. The adrenal gland is the sole source of this steroid in women, whereas in men the testes secrete 5% of DHEA-S and 10 – 20% of DHEA. The production of DHEA-S and DHEA is regulated by adrenocorticotropin (ACTH). Corticotropin-releasing hormone (CRH) and, to a lesser extent, arginine vasopressin (AVP) stimulate the release of adrenocorticotropin (ACTH) from the anterior pituitary gland (Fig.3). In turn, ACTH stimulates the adrenal cortex to secrete DHEA and DHEA-S, in addition to cortisol. -

Safety Data Sheet
SAFETY DATA SHEET SECTION 1: PRODUCT IDENTIFICATION PRODUCT NAME DHEA (Prasterone) (Micronized) PRODUCT CODE 0733 SUPPLIER MEDISCA Inc. Tel.: 1.800.932.1039 | Fax.: 1.855.850.5855 661 Route 3, Unit C, Plattsburgh, NY, 12901 3955 W. Mesa Vista Ave., Unit A-10, Las Vegas, NV, 89118 6641 N. Belt Line Road, Suite 130, Irving, TX, 75063 MEDISCA Pharmaceutique Inc. Tel.: 1.800.665.6334 | Fax.: 514.338.1693 4509 Rue Dobrin, St. Laurent, QC, H4R 2L8 21300 Gordon Way, Unit 153/158, Richmond, BC V6W 1M2 MEDISCA Australia PTY LTD Tel.: 1.300.786.392 | Fax.: 61.2.9700.9047 Unit 7, Heritage Business Park 5-9 Ricketty Street, Mascot, NSW 2020 EMERGENCY PHONE CHEMTREC Day or Night Within USA and Canada: 1-800-424-9300 NSW Poisons Information Centre: 131 126 USES Adjuvant; Androgen SECTION 2: HAZARDS IDENTIFICATION GHS CLASSIFICATION Toxic to Reproduction (Category 2) PICTOGRAM SIGNAL WORD Warning HAZARD STATEMENT(S) Reproductive effector, prohormone. Suspected of damaging fertility or the unborn child. May cause harm to breast-fed children. Causes serious eye irritation. Causes skin and respiratory irritation. Very toxic to aquatic life with long lasting effects. AUSTRALIA-ONLY HAZARDS Not Applicable. PRECAUTIONARY STATEMENT(S) Prevention Wash thoroughly after handling. Obtain special instructions before use. Do not handle until all safety precautions have been read and understood. Do not breathe dusts or mists. Do not eat, drink or smoke when using this product. Avoid contact during pregnancy/while nursing. Wear protective gloves, protective clothing, eye protection, face protection. Avoid release to the environment. Response IF ON SKIN (HAIR): Wash with plenty of water. -

Androgen Deficiency Guideline Results
Improving testosterone testing in people living with HIV V. Kopanitsa1, S. Flavell2, J. Ashby2, I. Ghosh2, S. Candfield2, U. Srirangalingm2, L. Waters2 1. University College London (UCL) Medical School; 2. Central and North West London NHS Foundation Trust Introduction Aims Symptomatic testosterone (T) deficiency is more common in people living 1. Review local practice in the clinic with HIV (PLWH) than the HIV negative male population; despite this, 2. Introduce a local guideline with investigation and management pathways specific guidelines are lacking. [1,2] for assessing T deficiency in PLWH with a view to earlier diagnosis and more efficient use of resources Patients with T deficiency can experience a number of symptoms such as 3. Re-audit after guideline implementation erectile dysfunction (ED) and reduced libido, and also less specific symptoms including low mood, fatigue and reduced muscle mass [1,2,3]. Total T (free and protein-bound) is the most common measurement reported Methods when a testosterone test is requested. In PLWH, raised sex hormone 1. A retrospective notes review was completed on all patients who had a T binding globulin (SHBG) levels are common, and so calculation of free T test between 01/06/17 and 30/11/17, and 17/09/18 to 14/12/18, before more accurately reflects T levels in this group. SHBG and Albumin tests are and after guideline implementation, respectively. The following outcomes needed for this for this calculation, which is done via an online calculator [4]. from the guideline were assessed: T also varies by circadian rhythm and should be measured at peak time in 2. -

A10 Anabolic Steroids Hardcore Info
CONTENTS GENERAL INFORMATION 3 Anabolic steroids – What are they? 4 How do they Work? – Aromatisation 5 More molecules – More problems 6 The side effects of anabolic steroids 7 Women and anabolic steroids 8 Injecting steroids 9 Abscesses – Needle Exchanges 10 Intramuscular injection 11 Injection sites 12 Oral steroids – Cycles – Stacking 13 Diet 14 Where do steroids come from? Spotting a counterfeit 15 Drug Information – Drug dosage STEROIDS 16 Anadrol – Andriol 17 Anavar – Deca-Durabolin 18 Dynabolon – Durabolin – Dianabol 19 Esiclene – Equipoise 20 Primobolan Depot – Proviron – Primobolan orals – Pronobol 21 Sustanon – Stromba, Strombaject – Testosterone Cypionate Testosterone Enanthate 22 Testosterone Propionate – Testosterone Suspension 23 Trenbolone Acetate – Winstrol OTHER DRUGS 24 Aldactone – Arimidex 25 Clenbuterol – Cytomel 26 Ephedrine Hydrochloride – GHB 27 Growth Hormone 28 Insulin 30 Insulin-Like Growth Factor-1 – Human Chorionic Gonadotrophin 31 Tamoxifen – Nubain – Recreational Drugs 32 Steroids and the Law 34 Glossary ANABOLIC STEROIDS People use anabolic steroids for various reasons, some use them to build muscle for their job, others just want to look good and some use them to help them in sport or body building. Whatever the reason, care needs to be taken so that as little harm is done to the body as possible because despite having muscle building effects they also have serious side effects especially when used incorrectly. WHAT ARE THEY? Anabolic steroids are man made versions of the hormone testosterone. Testosterone is the chemical in men responsible for facial hair, deepening of the voice and sex organ development, basically the masculine things Steroids are in a man. used in medicine to treat anaemia, muscle weakness after These masculine effects surgery etc, vascular are called the androgenic disorders and effects of testosterone. -

Androgen Deficiency Diagnosis and Management
4 Clinical Summary Guide Androgen Deficiency Diagnosis and management Androgen deficiency (AD) * Pituitary disease, thalassaemia, haemochromatosis. • Androgen deficiency is common, affecting 1 in 200 men under ** AD is an uncommon cause of ED. However, all men presenting 60 years with ED should be assessed for AD • The clinical presentation may be subtle and its diagnosis Examination and assessment of clinical features of AD overlooked unless actively considered Pre-pubertal onset – Infancy The GP’s role • Micropenis • GPs are typically the first point of contact for men with • Small testes symptoms of AD • The GP’s role in the management of AD includes clinical Peri-pubertal onset – Adolescence assessment, laboratory investigations, treatment, referral • Late/incomplete sexual and somatic maturation and follow-up • Small testes • Note that it in 2015 the PBS criteria for testosterone • Failure of enlargement of penis and skin of scrotum becoming prescribing changed; the patient must be referred for a thickened/pigmented consultation with an endocrinologist, urologist or member of • Failure of growth of the larynx the Australasian Chapter of Sexual Health Medicine to be eligible for PBS-subsidised testosterone prescriptions • Poor facial, body and pubic hair • Gynecomastia Androgen deficiency and the ageing male • Poor muscle development • Ageing may be associated with a 1% decline per year in serum Post-pubertal onset – Adult total testosterone starting in the late 30s • Regression of some features of virilisation • However, men who -

Male Hypogonadism: Quick Reference for Residents
Male hypogonadism: Quick Reference for Residents Soe Naing, MD, MRCP(UK), FACE Endocrinologist Associate Clinical Professor of Medicine Director of Division of Endocrinology Medical Director of Community Diabetes Care Center UCSF-Fresno Medical Education Program Version: SN/8-21-2017 Male hypogonadism From Harrison's Principles of Internal Medicine, 19e and Up-To-Date accessed on 8-21-2017 Testosterone is FDA-approved as replacement therapy only for men who have low testosterone levels due to disorders of the testicles, pituitary gland, or brain that cause hypogonadism. Examples of these disorders include primary hypogonadism because of genetic problems, or damage from chemotherapy or infection (mump orchitis). However, FDA has become aware that testosterone is being used extensively in attempts to relieve symptoms in men who have low testosterone for no apparent reason other than aging. Some studies reported an increased risk of heart attack, stroke, or death associated with testosterone treatment, while others did not. FDA cautions that prescription testosterone products are approved only for men who have low testosterone levels caused by a medical condition. http://www.fda.gov/Drugs/DrugSafety/ucm436259.htm 2 Hypothalamic-pituitary-testicular axis Schematic representation of the hypothalamic-pituitary- testicular axis. GnRH from the hypothalamus stimulates the gonadotroph cells of the pituitary to secrete LH and FSH. LH stimulates the Leydig cells of the testes to secrete testosterone. The high concentration of testosterone within the testes is essential for spermatogenesis within the seminiferous tubules. FSH stimulates the Sertoli cells within the seminiferous tubules to make inhibin B, which also stimulates spermatogenesis. Testosterone inhibits GnRH secretion, and inhibin B inhibits FSH secretion. -

Pharmacology/Therapeutics II Block III Lectures 2013-14
Pharmacology/Therapeutics II Block III Lectures 2013‐14 66. Hypothalamic/pituitary Hormones ‐ Rana 67. Estrogens and Progesterone I ‐ Rana 68. Estrogens and Progesterone II ‐ Rana 69. Androgens ‐ Rana 70. Thyroid/Anti‐Thyroid Drugs – Patel 71. Calcium Metabolism – Patel 72. Adrenocorticosterioids and Antagonists – Clipstone 73. Diabetes Drugs I – Clipstone 74. Diabetes Drugs II ‐ Clipstone Pharmacology & Therapeutics Neuroendocrine Pharmacology: Hypothalamic and Pituitary Hormones, March 20, 2014 Lecture Ajay Rana, Ph.D. Neuroendocrine Pharmacology: Hypothalamic and Pituitary Hormones Date: Thursday, March 20, 2014-8:30 AM Reading Assignment: Katzung, Chapter 37 Key Concepts and Learning Objectives To review the physiology of neuroendocrine regulation To discuss the use neuroendocrine agents for the treatment of representative neuroendocrine disorders: growth hormone deficiency/excess, infertility, hyperprolactinemia Drugs discussed Growth Hormone Deficiency: . Recombinant hGH . Synthetic GHRH, Recombinant IGF-1 Growth Hormone Excess: . Somatostatin analogue . GH receptor antagonist . Dopamine receptor agonist Infertility and other endocrine related disorders: . Human menopausal and recombinant gonadotropins . GnRH agonists as activators . GnRH agonists as inhibitors . GnRH receptor antagonists Hyperprolactinemia: . Dopamine receptor agonists 1 Pharmacology & Therapeutics Neuroendocrine Pharmacology: Hypothalamic and Pituitary Hormones, March 20, 2014 Lecture Ajay Rana, Ph.D. 1. Overview of Neuroendocrine Systems The neuroendocrine