Excellence in Communication Workbook
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

June 2020 #211
Click here to kill the Virus...the Italian way INSIDE THIS ISSUE: Table of Contents 1 Notams 2 Admin Reports 3-4-5 Covid19 Experience Flying the Line with Covid19 Paul Soderlind Scholarship Winners North Country Don King Atkins Stratocruiser Contributing Stories from the Members Bits and Pieces-June Gars’ Stories From here on out the If you use and depend on the most critical thing is NOT to RNPA Directory FLY THE AIRPLANE. you must keep your mailing address(es) up to date . The ONLY Instead, you MUST place that can be done is to send KEEP YOUR EMAIL UPTO DATE. it to: The only way we will have to The Keeper Of The Data Base: communicate directly with you Howie Leland as a group is through emails. Change yours here ONLY: [email protected] (239) 839-6198 Howie Leland 14541 Eagle Ridge Drive, [email protected] Ft. Myers, FL 33912 "Heard about the RNPA FORUM?" President Reports Gary Pisel HAPPY LOCKDOWN GREETINGS TO ALL MEMBERS Well the past few weeks and months have been a rude awakening for our past lifestyles. Vacations and cruises cancelled, all the major league sports cancelled, the airline industry reduced to the bare minimum. Luckily, I have not heard of many pilots or flight attendants contracting COVID19. Hopefully as we start to reopen the USA things will bounce back. The airlines at present are running at full capacity but with several restrictions. Now is the time to plan ahead. We have a RNPA cruise on Norwegian Cruise Lines next April. Things will be back to the new normal. -

Challenges and Opportunities for the Manmade Fiber Industry Page 8
the experts' magazine No. 34 | october 2020 Challenges and opportunities for the manmade fiber industry page 8 Factory know-how from a single source page 14 // editorial Dear Customers, dear Readers, Do you also greet people with an elbow bump? This form of greeting has meanwhile become a global symbol of our absolute determination to stay in contact with others and be active despite the risk of infection. This resolve is reflected in our own measures for dealing with the coronavirus pandemic as well as the unswerving, long-term master plans of major manmade fiber manufacturers, which are also securing our commercial stability. More on this topic in the interview on the following pages. We are also trying to do an elbow bump greeting with our customer publication here. As we are unable to meet up at our trade fair stand, this magazine provides a safe and socially- distanced tour of our exhibition topics that we had planned to present at the now postponed ITMA Asia. Needless to say, digitalization and automation technologies play important roles, as they will help us through these difficult times – both now and in the future. In this edition, you will also be able to read about sustainability and innovations focusing on clean technologies and ‘zero waste’ for energy-efficient, environmentally-friendly manufacturing. Because it is not just coronavirus that is tangibly changing the world we live in, so too is climate change. At the same time, we are leading the way towards our corporate mission: From Melt to Yarn, Fibers and Nonwovens. Along this stretch of the textile value chain, we have been striving for superlative quality for decades now – for fibers, yarns and hence all your textile products. -

Back in Business: Virginia Businesses Shed Some Restrictions
CIRCULATION 15,000 10,000 Free May 15, 2020 BACK IN BUSINESS: VIRGINIA BUSINESSES SHED SOME RESTRICTIONS ... Some Virginia businesses al- Overnight summer camps will re- main closed. lowed to open gradually as the Private campgrounds may open, governor keeps an eye on data with restrictions on the distance be- tween campsites. trends before deciding on sub- Beaches will remain open only for sequent phases and further eas- fishing and exercise. ing of restrictions Gyms and entertainment and amusement facilities will remain By Stefanie Jackson closed, but gyms may hold outdoor Today begins the first phase of Gov. classes with limitations. Ralph Northam’s plan for Virginia to Childcare facilities will remain open reopen for business. for working families. “We are not flipping a light switch The 10-person limit for gatherings from closed to open. It’s more of a dim- and social distancing guidelines will mer switch,” Northam said last Friday continue, as well as the recommenda- when he unveiled Phase One of the tions to wear face masks in public and three-phase Forward Virginia plan, wash hands frequently. which will gradually ease restrictions The “stay at home” order will be- that were put in place to combat the come a “safer at home” order – espe- COVID-19 pandemic. cially for those who are at risk due to Diners enjoy outdoor seating at the Cape Charles restaurant Ambrogia in May Some businesses will reopen at re- age or underlying health conditions, 2019. Under Gov. Ralph Northam’s plan, restaurants may resume outdoor duced capacity and others will remain Northam said. -
Social Distancing Greeting Posters
Social Distancing Greeting Posters Get Free Printables Every Week at GoZen.com/printables/ greeting! your own own your Make up up Make Greeting with both hands: Do this greeting Create a Cube dance to go along with this greeting. Do it while you greet someone! Add a short song to go along with 1. Print out your cube this greeting. template. Normal Sing it while printer paper will work, doing the yourPick but cardstock will make motions: greetings to try: a sturdier cube. these of favorite 2. Cut along the solid lines. Try using all 3 of these greetings 3. Fold along the dashed in a row: lines, making sure not to forget the tabs. 4. Apply tape or glue to the tabs. Attach the tabs to adjacent faces to construct your cube! Get Free Printables Every Week at GoZen.com/printables/ Foot wave SOCIAL DISTANCING Elbow bump Air high five GREETINGS A-okay Jazz hands Surf’s up Self hug Namaste Heart hands Peace Wink Foot wave SOCIAL DISTANCING Elbow bump Air high five GREETINGS A-okay Jazz hands Surf’s up Self hug Namaste Heart hands Peace Wink own greeting! own Make up your your up Make Greeting Create a with hands: both Do thisDo greeting dance to go Cube along with this greeting. Do it while you greet someone! Add a short song to go 1. Print out your cube along with this template. Normal greeting. Sing printer paper will work, it while doing but cardstock will make of favorite your Pick a sturdier cube. the motions: these greetings try: to 2. -

Media Release Public Health Association of Australia
Media Release Public Health Association of Australia 22 July 2020 It’s time to make the handshake history: but what comes next? The outbreak of COVID-19 has shaken up our world in so many ways. The Public Health Association of Australia (PHAA) is suggesting our most common greeting – the handshake - should be confined to history, in whatever our ‘new normal’ looks like post-pandemic. The first handshakes date back more than 2,000 years to ancient Greece, as a symbol of peace to show neither person was carrying a weapon. ‘Even before the arrival of coronavirus, there’s been a sense that the handshake may have had its day,’ said PHAA CEO Terry Slevin. ‘Most of us have been high-fiving for many years and in more recent times, we’ve seen even US President Obama adopt the uber-cool fist bump. ‘In these health conscious COVID-19 times, handshakes have been replaced by new meet and greet options. Our Prime Minister has led the way with his preferred elbow bump. Others test their balancing skills with a slightly awkward foot tap.’ Mr Slevin says he’s happy to lead the charge, and a national debate, on exactly what greeting Australians should adopt should we decide to retire the not-so-healthy handshake. ‘As we’ve emerged from lockdown and started returning to our workplaces, sporting venues and social meeting places, there’s a distinct nervousness and unease about how we should greet each other. ‘Confining the handshake to history makes good sense but humans like to adhere to social norms and we need to find a new common greeting as a popular substitute. -

OH, Behave! Volume 13, Issue 1
OH, Behave! Volume 13, Issue 1 …”bite size” Early Summer 2019 n e w s f r o m y o u r The Magic of the Greeter Apron R e g i o n 1 0 B e h a v i o r The way we are greeted in the each child an individual greeting ings are endless (see a list of S p e c i a l i s t morning makes a huge differ- even when drop-off gets busy. ideas on page 2), one doesn’t ence in how we begin our day By donning the apron with the need many materials to create an and, essentially, sets the tone choices displayed, the act of apron. A hardware store “tool” for the entire day. Combining welcoming and acknowledging a apron and fabric paints or mark- choice and visuals, the greeter child seems most sincere. ers is all that is required. Aprons apron ensures every child will can also be purchased at craft receive a greeting as they enter Being a “greeter” can be a job stores. Pockets can be useful in the classroom. Whether a child for a child in the class to per- the apron, but are not absolutely Positive teacher- chooses to get a bear hug, a form also. A child-size apron necessary. If the drawing and/or student handshake, or wave hello, these can be used to display a variety painting on an apron is of a con- relationships promote greetings help build and main- of greeting choices. However, if cern, laminating greeting icons is a sense of school tain relationships. -

Unit 3: Language Explorations LANGUAGE CHANGE Introductory
Unit 3: Language Explorations LANGUAGE CHANGE Introductory Reading Pack Contents From Much Ado About English by Richard Watson Todd: 1/1 ‘How old is an earthling?’ 1/2 ‘The Welsh penguin’ 1/3 ‘Wanted: A computer, female, age 1825’ From The Cambridge Encyclopedia of the English Language, edited by David Crystal: 1/5 ‘The Sources of the Lexicon’ 1/6 ‘Etymology’ From The Language Report by Susie Dent: 1/22 ‘Brokeback or Bounceback: How New Words Come About’ 1/23 ‘Bubbling Under: The Words of the Moment’ From Words Words Words by David Crystal: 2/8 ‘Wordchanges’ From Teach Yourself Linguistics by Jean Aitchison: 2/6 ‘Language Change’ III How old is an earthling? ~ The number of new words appearing in English is so great Jl that several dictionary producers publish a whole sup plement every year. Many of these inventions fade away qUickly, but some stay around to become part of generally accepted English. Sometimes we can guess the date at which the word was introduced into English quite accurately. For example, the title Ms (as opposed to Miss or Mrs) originates in the fem inist movement following the Second World War. An edu cated guess might therefore put its first use in the 1960s. This is fairly close for its widespread adoption, although the title was first used in print in 1949. Similarly, is it possible to make an educated guess abo.ut when the 1914-18 world war was first termed the First World War? Clearly, during the actual war itself people did not know that it would be the first of two major conflicts. -

1 Indian Namaste Goes Global in COVID-19
International Journal of Drug Research and Dental Science Volume 3 Issue 1 (Page: 1-3), 2021 ISSN: 2582-0826 Indian Namaste Goes Global In COVID-19 Era Madhusudhan Kempaiah Siddaiah 1* Pallavi Madhusudhan2 1Reader, Department of Pediatric and Preventive Dentistry, The Oxford Dental College, Hosur Main Road, Bommanahalli, Bengaluru, Karnataka, India. 2Department of Biochemistry, Mysore Makkala Koota & Sri Dharmasthala Manjunatheshwara Mahila Maha Vidyalaya, Mysuru, India. E-mail: [email protected] ORCID: https://orcid.org/0000-0002-0658-7581 Letter to the Editor Keywords: Anjali Mudra, Coronavirus, Covid-19, Namaste, Namaskar, Pandemic. To the Editor-in-Chief Coronavirus disease 2019 (COVID-19) pandemic began in China with a bunch of severe pneumonia cases, later identified to be caused by the severe acute respiratory syndrome coronavirus-2 in December 2019. Thailand reported the primary COVID-19 case outside of China on 13th January 2020, Africa reported its first case in Egypt on 14th February 2020 and Nigeria reported its patient of COVID-19 on 27th February 2020. Virtually, all countries within the world are affected.1 Globally, countries and international organizations are putting efforts to halt the transmission of the disease by preventive measures, management protocols, research activities for definitive treatment and vaccines.1 The common principles in preventing and controlling infectious diseases are to eradicate the infection source, to cut off the transmission route, and to shield the susceptible population.2 Physical distancing is one of the measures being used to curtail the transmission of the virus. Transmission of COVID-19 by contact can occur when contaminated hands touch the mucosa of the eyes, nose or mouth. -

Legal-Graphics 10-05 COVID
Days since first COVID-19 Events sign of virus Indonesia North Carolina 24 Pennsylvania 26 Countries Affected Wyoming Madagascar 49 Ecuador Kyrgyzstan Massachusetts India New Hamshire 25 South Carolina 32 Philippines Feb. 18, 2020 Chile North Dakota Montserrat Zimbabwe 56 Country Name 62 Macau Nepal Illinois Ireland 31 Barbados El Salvador Washington 53 Italy Russia Georgia 28 So. Africa Peru Missouri Nebraska Bolivia 13 15 California Worldwide Argentina New Mexico Montana New Caledonia Papau or Coronavirus Deaths Austria Netherlands 17 Minnesota 19 Arizona 24 Kansas 23 13 Gambia Mauritius Taiwan Hong Kong Malaysia Sri Lanka India UK New York 19 New Jersey Tennessee 25 Connecticut 14 Turkey Michigan Mississippi 21 Maine 20 over 2,000 Nicaragua Cape Verde >5,000 Deaths* Wisconsin 13 South Korea Vietnam Australia Cambodia UAE Spain Switzerland Pakistan Oregon 24 Florida 31 Colorado 21 Maryland 25 Kentucky 19 Utah Virginia Vermont 26 Ohio 14 South Dakota Delaware 13 Idaho 12 Montenegro Bermuda or East Timor China France Thailand Japan US Singapore Canada Germany Finland Sweden Belgium Egypt Iran Israel Iraq Brazil Mexico Rhode Island 27 Texas 29 Nevada 27 Hawaii 17 Indiana 17 Oklahoma 15 Iowa Lousiana 13 St. Vincent Arkansas Alaska 15 Alabama 22 St. Maarten Djibouti West Virginia 6 # Number of countries Uganda reporting on same day France ? 11 5 4 8 3 Bangladesh 20 9 7 6 (symbol is linked to page with more detail) 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53 54 55 56 57 58 59 60 61 62 63 64 65 66 67 68 69 70 71 72 73 74 75 76 77 78 79 80 81 82 83 84 85 86 87 88 89 90 91 92 93 94 95 96 97 98 99 100 101 102 103 104 105 106 107 108 109 110 111 112 113 114 115 116 117 118 119 120 121 122 123 124 125 US States Affected Nov. -

Jewish Charities Fear Budget Cuts
Weekly Since 1924 $40 PER YEAR WITHIN MONROE COUNTY, $42 OUTSIDE COUNTY/SEASONAL 70¢ PER ISSUE n VOL. XCVIII, NO. 9 n ROCHESTER, N.Y. n AV 23, 5780 n AUGUST 13, 2020 Is Iran Being Hit by Sabotage? Israel May Not Top Progressive Agendas Now, but Tensions With the Pro-Israel Community Will Persist BY RON KAMPEAS WASHINGTON (JTA) — The Israel issue isn’t necessarily to- ward the top of the progressive to-do lists at the moment, but that doesn’t mean elements of the movement are any less at odds with the pro-Israel com- Iranian President Hassan Rouhani and head of the Atomic Energy munity. Organization of Iran (AEOI) Ali Akbar Salehi near the Bushehr nuclear That was evident in an inter- plant. (Wikimedia Commons) view this week that the Dem- ocratic Socialists of America’s BY ISRAEL KASNETT Iran in recent weeks has led to New York City co-chairwoman, (JNS) — A mysterious string wide speculation over whether Sumathy Kumar, gave with the of fires and explosions at mili- these incidents are mere coin- news site Kings County Politics. Rep. Rashida Tlaib waves as she endorses Democratic presidential hopeful tary and industrial sites across (Sabotage — Page 4) Here’s the passage involving Sen. Bernie Sanders at a campaign rally in Detroit, Oct. 27, 2019. (Jeff Kowalsky/ Israel: AFP via Getty Images) Kings County Politics: I no- Lebanese MP: ‘Hezbollah ticed in the DSA questionnaire this year’s state races that they (BDS) the state of Israel for their given to all local candidates were asked if they support Di- policies regarding Palestinians. -

Recovering Civility During COVID-19
Recovering Civility during COVID-19 Matteo Bonotti · Steven T. Zech Recovering Civility during COVID-19 Matteo Bonotti · Steven T. Zech Recovering Civility during COVID-19 Matteo Bonotti Steven T. Zech Politics and International Relations Politics and International Relations Monash University Monash University Melbourne, Australia Melbourne, Australia ISBN 978-981-33-6705-0 ISBN 978-981-33-6706-7 (eBook) https://doi.org/10.1007/978-981-33-6706-7 © The Editor(s) (if applicable) and The Author(s) 2021. This book is an open access publication. Open Access This book is licensed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license and indicate if changes were made. The images or other third party material in this book are included in the book’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the book’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. The use of general descriptive names, registered names, trademarks, service marks, etc. in this publication does not imply, even in the absence of a specific statement, that such names are exempt from the relevant protective laws and regulations and therefore free for general use. -
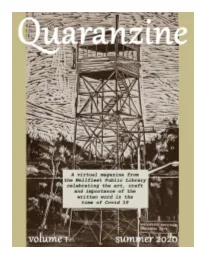
Table of Contents
Table of Contents Robert Cataldo page 3 James Cornell page 5 John DeBruicker page 7 Corey Farrenkopf page 8 Judi Getch Brodman page 9 Barry Hellman page 10 Aylette Jenness page 11 Lauren Kalita page 12 Lucille Lang Day page 15 Roger Marks page 16 Ed Meek page 18 Ed Miller page 19 John Morrissey page 20 Debra Murphy page 21 Candace Perry page 22 Marge Piercy page 24 Guy Rotella page 25 Wilderness Sarchild page 26 John Shuman page 27 Maxine Susman page 29 August 15th, 2020 In setting out to publish our “Quaranzine”, we decided that the library could play a role in the creation of an online literary journal. It is a mixture of literature, technology, and a “place” for community to come together - all the things that make the Wellfleet Library special. We assumed that many of you were writing during this time of isolation; of frustration; of social injustice. When we put out the call for pieces, we did not know what we would receive. We received a bounty. We hope you enjoy our first issue. There will most certainly be more issues to follow. One thing is clear - people have something to say. Jennifer Wertkin Library Director Garden Tomatoes “You can’t buy love or garden tomatoes.” - my mother On the way back from the picnic that afternoon, we had made plans to stop in at Beth Israel Hospital where my older sister Lorena had just given birth to a baby girl. Francis had met my sister on several occasions already and was more than happy to tag along, despite the heat.