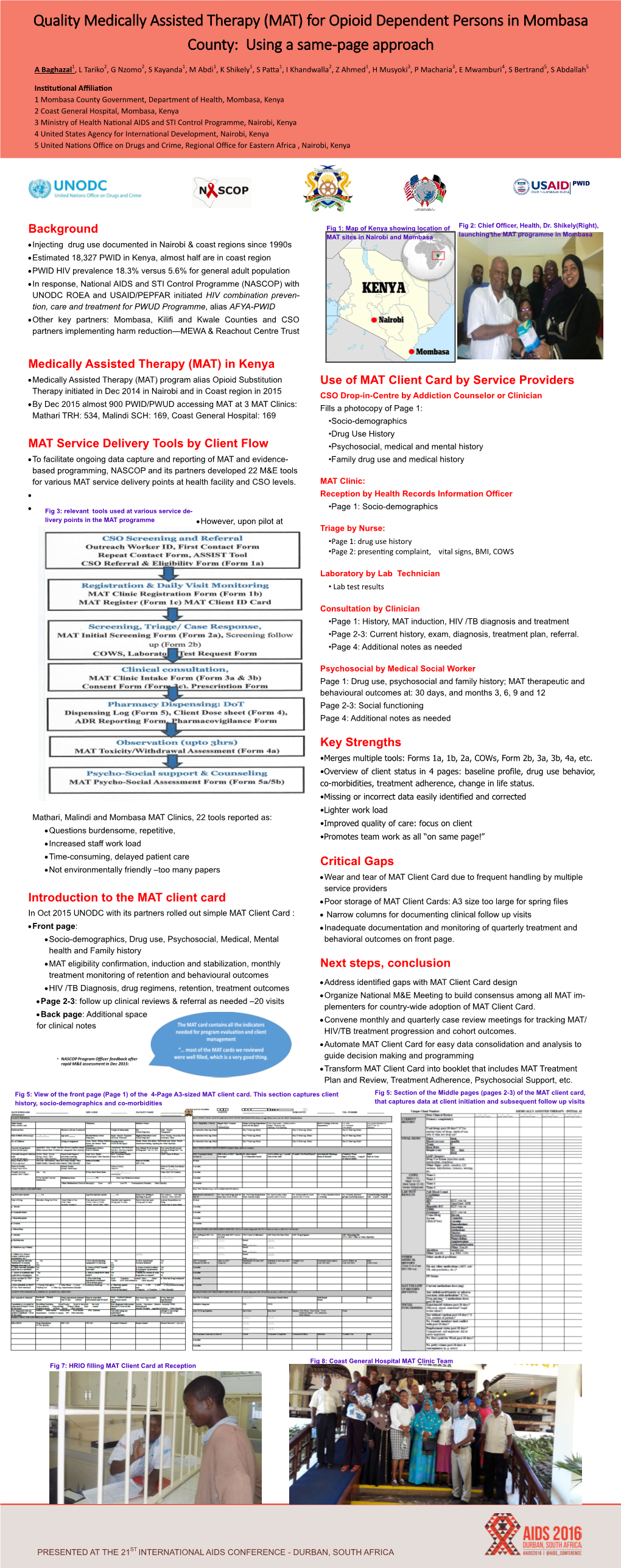
Background Medically Assisted Therapy (MAT) in Kenya MAT
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

County Urban Governance Tools
County Urban Governance Tools This map shows various governance and management approaches counties are using in urban areas Mandera P Turkana Marsabit P West Pokot Wajir ish Elgeyo Samburu Marakwet Busia Trans Nzoia P P Isiolo P tax Bungoma LUFs P Busia Kakamega Baringo Kakamega Uasin P Gishu LUFs Nandi Laikipia Siaya tax P P P Vihiga Meru P Kisumu ga P Nakuru P LUFs LUFs Nyandarua Tharaka Garissa Kericho LUFs Nithi LUFs Nyeri Kirinyaga LUFs Homa Bay Nyamira P Kisii P Muranga Bomet Embu Migori LUFs P Kiambu Nairobi P Narok LUFs P LUFs Kitui Machakos Kisii Tana River Nyamira Makueni Lamu Nairobi P LUFs tax P Kajiado KEY County Budget and Economic Forums (CBEFs) They are meant to serve as the primary institution for ensuring public participation in public finances in order to im- Mom- prove accountability and public participation at the county level. basa Baringo County, Bomet County, Bungoma County, Busia County,Embu County, Elgeyo/ Marakwet County, Homabay County, Kajiado County, Kakamega County, Kericho Count, Kiambu County, Kilifi County, Kirin- yaga County, Kisii County, Kisumu County, Kitui County, Kwale County, Laikipia County, Machakos Coun- LUFs ty, Makueni County, Meru County, Mombasa County, Murang’a County, Nairobi County, Nakuru County, Kilifi Nandi County, Nyandarua County, Nyeri County, Samburu County, Siaya County, TaitaTaveta County, Taita Taveta TharakaNithi County, Trans Nzoia County, Uasin Gishu County Youth Empowerment Programs in urban areas In collaboration with the national government, county governments unveiled -

Second Health Strategic and Investment Plan (Chsip Ii)
MOMBASA COUNTY of HealthDepartment Services SECOND HEALTH STRATEGIC AND INVESTMENT PLAN (CHSIP II) 2018 – 2022 A Healthy and Productive Community Abridged Version August 2018 CONTENTS CONTENTS ii ABBREVIATIONS iii LIST OF FIGURES v LIST OF TABLES 6 Foreword 7 Acknowledgment 8 Executive Summary 9 1 COUNTY INSTITUTIONAL REVIEW 1 1.1 About Mombasa County ........................................................................................................ 1 1.2 Population Demographics...................................................................................................... 3 1.3 County Health Sector............................................................................................................. 3 1.4 Purpose of the Second County Health Sector Strategic and Investment Plan (CHSIP II) 2018-2022 .............................................................................................................................. 4 1.5 County Performance Management Framework ..................................................................... 5 1.6 The Planning Process............................................................................................................. 6 1.7 Mission, Vision and Values ................................................................................................... 7 2 SITUATION ANALYSIS 8 2.1 Summary of County Health Sector Performance 2013/14 – 2017/18 ................................... 8 2.2 Situation Analysis ................................................................................................................. -

Citizens' Perception of Leadership During COVID-19 Times in Mombasa, Kenya
Citizens’ Perception of Leadership during COVID-19 Times in Mombasa, Kenya Fathima Azmiya Badurdeen To cite this version: Fathima Azmiya Badurdeen. Citizens’ Perception of Leadership during COVID-19 Times in Mombasa, Kenya. 2020, https://mambo.hypotheses.org/2853. halshs-03078567 HAL Id: halshs-03078567 https://halshs.archives-ouvertes.fr/halshs-03078567 Submitted on 16 Dec 2020 HAL is a multi-disciplinary open access L’archive ouverte pluridisciplinaire HAL, est archive for the deposit and dissemination of sci- destinée au dépôt et à la diffusion de documents entific research documents, whether they are pub- scientifiques de niveau recherche, publiés ou non, lished or not. The documents may come from émanant des établissements d’enseignement et de teaching and research institutions in France or recherche français ou étrangers, des laboratoires abroad, or from public or private research centers. publics ou privés. Institut français de recherche en Afrique French Institute for Research in Africa MAMBO! XVII (4), 2020 COVID-19 Special Papers Citizens’ Perception of Leadership during COVID-19 Times in Mombasa, Kenya Fathima AZMIYA BADURDEEN Cite: AZMIYA BADURDEEN, Fathima. 2020. Citizens’ Perception of Leadership during COVID-19 Times in Mombasa, Kenya. Mambo! vol. XVII, no. 4. URL: https://mambo.hypotheses.org/2853 The author: Dr. Fathima Azmiya Badurdeen is a lecturer in Development Studies at the Department of Social Sciences, Technical University of Mombasa, working on issues related to youth, gender and violent extremism. The article is an outcome of the research funded by the French Institute for Research in Africa (IFRA) from April to September 2020. Email: [email protected]. -
CONFLICT SNAPSHOT Kenya December 2020 Introduction
Funded by the European Union CONFLICT SNAPSHOT Kenya December 2020 Introduction Kenya is a large culturally and ethnic diverse country, with over 40 different ethnic groups and numerous superimposed conflicts. Ethnic tensions and clashes coupled with political instability that manifests during the election period have been on the rise in the recent past. Recurrent drought that pushes herders into farmlands in search of pasture has led to violent clashes between herders and farmers in Garissa and Tana River counties. Ethnic group affiliation and highly centralised ethnopolitics are the primary identity of many Kenyans, especially during periods of turmoil. According to the Conflict Analysis of Kenya report, Kenyan Muslims have been marginalised within the Kenyan state and feel like they are treated as second-rate citizens. Data collection and analysis Data for the conflict snapshot COVID-19 series in Kenya was airoi gathered from 21-25 September in the following target zones: arissa This coincided with a period of relative calm in terms of ana iver COVID-19 caseloads and containment measures in Kenya, Kilifi as it fell in between the first and second wave of outbreaks omasa and many people believed there would soon be a return to normalcy. This perception may have influenced certain survey wale responses and we expect to see changes in this in the next round of snapshot reports. This report was prepared by the Search for Common Ground Kenya team, with support from Search’s COVID-19 Response Programming Team and Institutional Learning Team. For more information on the data collection methodology and tools used by Search for Common Ground for this research, click here. -

Mombasa County Crime and Violence Report
MOMBASA COUNTY CRIME AND VIOLENCE RAPID ASSESSMENT MOMBASA COUNTY CRIME AND VIOLENCE RAPID ASSESSMENT Cover photo credit: Andrea Albini | Creative Commons 3.0 Design and copy editing: Laura C. Johnson II Contents Foreword .................................................v Acknowledgements .........................................vi Acronyms ................................................vii 1 Introduction .............................................1 Crime and Violence Prevention in Kenya ...............................3 Crime and Violence Prevention Training ...............................4 County-Level Crime and Violence Prevention ..........................4 Framework for Analysis .............................................7 Goals of the Rapid Assessment ......................................9 Methodology . .9 2 Background: Crime and Violence Trends in Kenya ............13 Boda-Boda-Related Crime and Violence .............................14 Alcohol and Drug Abuse ...........................................14 Sexual and Gender-Based Violence ..................................16 Violence against Children ..........................................16 Radicalization and Recruitment into Violent Extremism ..................17 3 Rapid Assessment of Mombasa County .....................19 Overview of County ...............................................19 Cross-Cutting Drivers of Crime and Violence ..........................20 Dynamics of Crime and Violence ....................................23 Security Interventions .............................................40 -

(Nema)Table of Contents
ENVIR ONMENTAL AND SOCIAL IMPACT ASSESSMENT REPORT (ESIA) AND RESETLEMENT ACTION PLAN (RAP) FOR THE PROPSED MALINDI AIRPORT RUNWAY EXPANSION PROJECT TENDER NO. KAA/OT/MLD/1507/2018/2019 NOVEMBER, 2020 KENYA AIRPORTS AUTHORITY ESIA and RAP report for the proposed Extension of Malindi Airport Runway CERTIFICATION This ESIA study report has been prepared in accordance with the Environmental Management and Coordination Act (EMCA) 1999 and the Environmental (Impact Assessment and Audit) Regulations 2003 for submission to the National Environment Management Authority (NEMA). The following experts conducted the study and prepared this report on behalf of Eco-solutions Limited: FOR Eco Solutions Limited, iPlan Consult (Int’l) Limited, P.O. BOX 20492 – 00100, P.O BOX 28634-00100 NAIROBI, KENYA. NAIROBI. TEL: +254 722 273935. TEL: +254 721891005. Email: [email protected] Email: [email protected] Name Designation NEMA Date & Signature REG. NO. 1. SHADRACK K. MBUTA EIA LEAD EXPERT 6315 2. WALLACE ISABOKE EIA LEAD EXPERT 2622 3. CYNTHIA OTARA ASS. EXPERT 11450 The Proponent; Kenya Airports Authority (KAA), P.O. Box 19001-00501, Nairobi. Signature___________________________ Date_____________________________ Designation: Environment Manager Disclaimer: This ESIA Report is confidential to Kenya Airports Authority (KAA), and any use of the materials hereof should be strictly in accordance with the contractual agreement between Eco-solutions and Kenya Airports Authority (KAA). It is, however, subject to conditions spelt out in the Environmental (Impact Assessment and Audit) Regulations, 2003. Eco Solutions Ltd; iPlan Consult (Int’l) Limited November 2020 2 KENYA AIRPORTS AUTHORITY ESIA and RAP report for the proposed Extension of Malindi Airport Runway EXECUTIVE SUMMARY 1. -

Out Patient Facilities for Nhif Supa Cover Baringo County Bomet County Bungoma County Busia County
OUT PATIENT FACILITIES FOR NHIF SUPA COVER BARINGO COUNTY BRANCH No HOSPITAL NAME POSTAL ADDRESS OFFICE 1 TIONYBEI MEDICAL CLINIC 396-30400, KABARNET KABARNET 2 BARINGO DISTRICT HOSPITAL (KABARNET) 21-30400, KABARNET KABARNET 3 REALE MEDICAL CENTRE-KABARNET 4694-30100, ELDORET KABARNET 4 KERIO HOSPITAL LTD 458-30400, KABARNET KABARNET 5 RAVINE GLORY HEALTH CARE SERVICES 612-20103, ELDAMA RAVINE KABARNET 6 ELDAMA RAVINE NURSING HOME 612-20103, ELDAMA RAVINE KABARNET 7 BARNET MEMORIAL MEDICAL CENTRE 490-30400, KABARNET KABARNET BOMET COUNTY BRANCH No HOSPITAL NAME POSTAL ADDRESS OFFICE 1 CHELYMO MEDICAL CENTRE 37-20422 SILIBWET BOMET 2 KAPKOROS HEALTH CENTRE 20400 BOMET BOMET BUNGOMA COUNTY BRANCH No HOSPITAL NAME POSTAL ADDRESS OFFICE 1 CHWELE SUBCOUNTY HOSPITAL 202 - 50202 CHWELE BUNGOMA 2 LUMBOKA MEDICAL SERVICES 1883 - 50200 BUNGOMA BUNGOMA 3 WEBUYE HEALTH CENTRE 25 - WEBUYE BUNGOMA 4 ST JAMES OPTICALS 2141 50200 BUNGOMA 5 NZOIA MEDICAL CENTRE 471 - 50200 BUNGOMA BUNGOMA 6 TRINITY OPTICALS LIMITED PRIVATE BAG BUNGOMA BUNGOMA 7 KHALABA MEDICAL SERVICES 2211- 50200 BUNGOMA BUNGOMA 8 ARARAT MEDICAL CLINIC 332 KIMILILI BUNGOMA 9 SIRISIA SUBDISTRICT HOSPITAL 122 - 50208 SIRISIA BUNGOMA 10 NZOIA MEDICAL CENTRE - CHWELE 471 - 50200 BUNGOMA BUNGOMA 11 OPEN HEART MEDICAL CENTRE 388 - 50202 CHWELE BUNGOMA 12 ICFEM DREAMLAND MISSION HOSPITAL PRIVATE BAG KIMILILI BUNGOMA 13 EMMANUEL MISSION HEALTH CENTRE 53 - 50207 MISIKHU BUNGOMA 14 WEBUYE DISTRICT HOSPITAL 25 - 50205 BUNGOMA 15 ELGON VIEW MEDICAL COTTAGE 1747 - 50200 BUNGOMA BUNGOMA 16 FRIENDS -

County Name County Code Location
COUNTY NAME COUNTY CODE LOCATION MOMBASA COUNTY 001 BANDARI COLLEGE KWALE COUNTY 002 KENYA SCHOOL OF GOVERNMENT MATUGA KILIFI COUNTY 003 PWANI UNIVERSITY TANA RIVER COUNTY 004 MAU MAU MEMORIAL HIGH SCHOOL LAMU COUNTY 005 LAMU FORT HALL TAITA TAVETA 006 TAITA ACADEMY GARISSA COUNTY 007 KENYA NATIONAL LIBRARY WAJIR COUNTY 008 RED CROSS HALL MANDERA COUNTY 009 MANDERA ARIDLANDS MARSABIT COUNTY 010 ST. STEPHENS TRAINING CENTRE ISIOLO COUNTY 011 CATHOLIC MISSION HALL, ISIOLO MERU COUNTY 012 MERU SCHOOL THARAKA-NITHI 013 CHIAKARIGA GIRLS HIGH SCHOOL EMBU COUNTY 014 KANGARU GIRLS HIGH SCHOOL KITUI COUNTY 015 MULTIPURPOSE HALL KITUI MACHAKOS COUNTY 016 MACHAKOS TEACHERS TRAINING COLLEGE MAKUENI COUNTY 017 WOTE TECHNICAL TRAINING INSTITUTE NYANDARUA COUNTY 018 ACK CHURCH HALL, OL KALAU TOWN NYERI COUNTY 019 NYERI PRIMARY SCHOOL KIRINYAGA COUNTY 020 ST.MICHAEL GIRLS BOARDING MURANGA COUNTY 021 MURANG'A UNIVERSITY COLLEGE KIAMBU COUNTY 022 KIAMBU INSTITUTE OF SCIENCE & TECHNOLOGY TURKANA COUNTY 023 LODWAR YOUTH POLYTECHNIC WEST POKOT COUNTY 024 MTELO HALL KAPENGURIA SAMBURU COUNTY 025 ALLAMANO HALL PASTORAL CENTRE, MARALAL TRANSZOIA COUNTY 026 KITALE MUSEUM UASIN GISHU 027 ELDORET POLYTECHNIC ELGEYO MARAKWET 028 IEBC CONSTITUENCY OFFICE - ITEN NANDI COUNTY 029 KAPSABET BOYS HIGH SCHOOL BARINGO COUNTY 030 KENYA SCHOOL OF GOVERNMENT, KABARNET LAIKIPIA COUNTY 031 NANYUKI HIGH SCHOOL NAKURU COUNTY 032 NAKURU HIGH SCHOOL NAROK COUNTY 033 MAASAI MARA UNIVERSITY KAJIADO COUNTY 034 MASAI TECHNICAL TRAINING INSTITUTE KERICHO COUNTY 035 KERICHO TEA SEC. SCHOOL -

Youth, Peace and Security in Kenya by Olawale Ismail
Youth, peace and Security in Kenya by Olawale Ismail Youth, Peace and Security in Kenya Revised Draft 12/12/2017 1 Youth, peace and Security in Kenya by Olawale Ismail 1. Introduction Kenya underscores the spirit and letter of UNSC Resolution 2250 in many ways. Over the last decade, Kenya’s political-security volatility has been well documented by extant research and media reports. Incidence of political and election-related violence, radicalization and violent extremism, inter-ethnic and inter-communal clashes, pastoralist violence, and state-led violence dot Kenya’s peace and security landscape in the last 10 years. While most of these peace and security issues predate the last decade, their scale, spread, intensity and impacts are unprecedented. As in similar contexts, much of research and policy attention have focused mostly on the role of young women and men largely as victims and perpetrators of violence, respectively. However, emerging pointers, as encapsulated in UNSCR 2250, signpost the crucial role and contribution of young people to preventing violence, responding to violence and rebuilding peace, and informed contributions to the security and stability of communities, countries and world at large. Kenya is no different; female and male youth on their own and/or in collaboration with other stakeholders, actively contributes to conflict prevention, reconciliation and peacebuilding in Kenya. Accordingly, this report presents an overview of the contemporary peace and security challenges in Kenya, and the responses of young people in the form of their roles and contributions to peacebuilding efforts. This case-study was commissioned by UNFPA and PBSO for the Progress Study on YPS requested by SCR 2250, with funding support from SIDA. -

Mombasa County
REPUBLIC OF KENYA MOMBASA COUNTY Mombasa Kwale Kili Tana River Lamu Taita Taveta Introduction: The European Union (EU) is undertaking a joint initiative known as Go Blue across all six counties in the Coast Region of Kenya. The EU is working with implementing partners from four Member States agencies - Germany, Italy, Portugal and France, and UN Habitat and UNEP. The implementation is done in close cooperation with the Jumuiya ya Kaunti za Pwani (JKP) and the relevant government ministries at national level. The initiative is under the umbrella of the Blue Economy. The focus is on coastal urban centres for inclusive, integrated, participatory, and sustainable economic growth, including conserving the coastal marine environment and promoting effective and integrated maritime governance. The initiative seeks to create employment with a special emphasis on youth and women. Implementing partners: Germany, implemented by the Deutsche Gesellschaft für Internationale Zusammenarbeit GIZ GmbH; Italy, through the Italian Agency for Development Cooperation (AICS); Portugal through the Camoes Institute; and France, through Expertise France (the French technical cooperation agency). Two UN agencies, UN Habitat and UNEP are partners through a delegated agreement. Germany GIZ Italy (AICS) Portugal Camões France UN-Habitat and UNEP: Expertise Support Areas Support Areas Support Areas Support Areas Skills Small scale fisheries Tourism and Cultural Support Area Innovative Land- Development, and cassava value Heritage Maritime Sea Planning and MSME support chain development, security Management and Aquaculture Technical Assistance to JKP Secretariat European Union Financing: EUR 24,750,000 Location: Mombasa, Kwale, Kilifi, Tana River, Lamu, and Taita Taveta Counties Specific Objectives: Go Blue Growth: To accelerate sustained, inclusive, and sustainable economic Specific 1 urban coastal growth to create jobs with a special focus on women and young objective people. -

INSULT to INJURY the 2014 Lamu and Tana River Attacks and Kenya’S Abusive Response
INSULT TO INJURY The 2014 Lamu and Tana River Attacks and Kenya’s Abusive Response HUMAN RIGHTS WATCH hrw.org www.khrc.or.ke Insult to Injury The 2014 Lamu and Tana River Attacks and Kenya’s Abusive Response Copyright © 2015 Human Rights Watch All rights reserved. Printed in the United States of America ISBN: 978-1-6231-32446 Cover design by Rafael Jimenez Human Rights Watch defends the rights of people worldwide. We scrupulously investigate abuses, expose the facts widely, and pressure those with power to respect rights and secure justice. Human Rights Watch is an independent, international organization that works as part of a vibrant movement to uphold human dignity and advance the cause of human rights for all. Human Rights Watch is an international organization with staff in more than 40 countries, and offices in Amsterdam, Beirut, Berlin, Brussels, Chicago, Geneva, Goma, Johannesburg, London, Los Angeles, Moscow, Nairobi, New York, Paris, San Francisco, Sydney, Tokyo, Toronto, Tunis, Washington DC, and Zurich. For more information, please visit our website: http://www.hrw.org JUNE 2015 978-1-6231-32446 Insult to Injury The 2014 Lamu and Tana River Attacks and Kenya’s Abusive Response Map of Kenya and Coast Region ........................................................................................ i Summary ......................................................................................................................... 1 Recommendations .......................................................................................................... -

Mombasa City Residents' Perception Of
MOMBASA CITY RESIDENTS’ PERCEPTION OF HEALTH RISKS OF CLIMATE CHANGE AND ITS IMPACT ON BAHAVIOUR CHANGE Fredrick Okoth Okaka: [email protected] Department of Geography, Moi University, P.O. Box 3900 Eldoret, Kenya. ABSTRACT Climate change has proved to have adverse consequences on human health as well as exacerbates health risks. These effects on human health are diverse in nature and range from direct effects due to extreme weather events such as heat waves, floods and storms, to indirect effects such as those caused by water and food shortages. However, there have been relatively few studies on public awareness, understanding and concern on the health threat of climate change. Mombasa City has been identified as highly vulnerable concerning adverse effects of climate change due to its low altitude and high temperatures. This paper examines Mombasa City residents’ perception of health risks of climate change and its impact on their behavior change. This study was a cross-sectional survey of respondents from three residential areas in Mombasa City, Kenya. A total of 300 households were selected through random and systematic sampling, however, of the 300 households selected, the researchers were able to retrieve 290 properly completed questionnaires. About 10 (3%) respondents were not aware of climate change and thus were left out of subsequent analysis. The questionnaire was supplemented with 9 focus group discussions (FGDs) and 9 key informant interviews (KIIs). Personal perceived susceptibility to the health threats of climate change was explored with the Health Belief Model (HBM) as a conceptual frame and analyzed through logistic regressions. The study found that over 90% of the respondents perceived that climate change poses a risk to their health.