CGRP Signaling Via CALCRL Increases Chemotherapy Resistance and Stem Cell Properties in Acute Myeloid Leukemia
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Mutant RAMP2 Causes Primary Open-Angle Glaucoma Via the CRLR-Camp Axis
© American College of Medical Genetics and Genomics ARTICLE Mutant RAMP2 causes primary open-angle glaucoma via the CRLR-cAMP axis Bo Gong, PhD1,2, Houbin Zhang, PhD1, Lulin Huang, PhD1, Yuhong Chen, MD3, Yi Shi, PhD1, Pancy Oi-Sin Tam, MS4, Xianjun Zhu, PhD1, Yi Huang, MD1,5, Bo Lei, PhD6, Periasamy Sundaresan, PhD7, Xi Li, MS1, Linxin Jiang, MS1, Jialiang Yang, MS1, Ying Lin, MS1, Fang Lu, PhD1, Lijia Chen, MRCSEd (Ophth), PhD4, Yuanfeng Li, MS1, Christopher Kai-Shun Leung, MD4, Xiaoxin Guo, MS1, Shanshan Zhang, MS1, Guo Huang, MS1, Yaqi Wu, MS1, Tongdan Zhou, MS1, Ping Shuai, PhD1, Clement Chee-Yung Tham, FRCOphth4, Nicole Weisschuh, PhD8, Subbaiah Ramasamy Krishnadas, MD7, Christian Mardin, MD9, André Reis, PhD10, Jiyun Yang, MD1, Lin Zhang, PhD1,3, Yu Zhou, PhD1, Ziyan Wang, PhD1, Chao Qu, MD11, Peter X. Shaw, PhD12, Chi-Pui Pang, DPhil4, Xinghuai Sun, MD3, Weiquan Zhu, MD5, Dean Yaw Li, MD5, Francesca Pasutto, PhD10 and Zhenglin Yang, MD, PhD1,2 Purpose: Primary open-angle glaucoma (POAG) is the leading 4763 POAG patients, whereas no variants were detected in any cause of irreversible blindness worldwide and mutations in known exon of RAMP2 in 10,953 control individuals. Mutant RAMP2s genes can only explain 5–6% of POAG. This study was conducted aggregated in transfected cells and resulted in damage to the AM- to identify novel POAG-causing genes and explore the pathogenesis RAMP2/CRLR-cAMP signaling pathway. Ablation of one Ramp2 of this disease. allele led to cAMP reduction and retinal ganglion cell death in mice. Methods: Exome sequencing was performed in a Han Chinese Conclusion: This study demonstrated that disruption of RAMP2/ cohort comprising 398 sporadic cases with POAG and 2010 CRLR-cAMP axis could cause POAG and identified a potential controls, followed by replication studies by Sanger sequencing. -

Pharmacokinetics, Pharmacodynamics and Drug
pharmaceutics Review Pharmacokinetics, Pharmacodynamics and Drug–Drug Interactions of New Anti-Migraine Drugs—Lasmiditan, Gepants, and Calcitonin-Gene-Related Peptide (CGRP) Receptor Monoclonal Antibodies Danuta Szkutnik-Fiedler Department of Clinical Pharmacy and Biopharmacy, Pozna´nUniversity of Medical Sciences, Sw.´ Marii Magdaleny 14 St., 61-861 Pozna´n,Poland; [email protected] Received: 28 October 2020; Accepted: 30 November 2020; Published: 3 December 2020 Abstract: In the last few years, there have been significant advances in migraine management and prevention. Lasmiditan, ubrogepant, rimegepant and monoclonal antibodies (erenumab, fremanezumab, galcanezumab, and eptinezumab) are new drugs that were launched on the US pharmaceutical market; some of them also in Europe. This publication reviews the available worldwide references on the safety of these anti-migraine drugs with a focus on the possible drug–drug (DDI) or drug–food interactions. As is known, bioavailability of a drug and, hence, its pharmacological efficacy depend on its pharmacokinetics and pharmacodynamics, which may be altered by drug interactions. This paper discusses the interactions of gepants and lasmiditan with, i.a., serotonergic drugs, CYP3A4 inhibitors, and inducers or breast cancer resistant protein (BCRP) and P-glycoprotein (P-gp) inhibitors. In the case of monoclonal antibodies, the issue of pharmacodynamic interactions related to the modulation of the immune system functions was addressed. It also focuses on the effect of monoclonal antibodies on expression of class Fc gamma receptors (FcγR). Keywords: migraine; lasmiditan; gepants; monoclonal antibodies; drug–drug interactions 1. Introduction Migraine is a chronic neurological disorder characterized by a repetitive, usually unilateral, pulsating headache with attacks typically lasting from 4 to 72 h. -

Current and Prospective Pharmacological Targets in Relation to Antimigraine Action
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Erasmus University Digital Repository Naunyn-Schmiedeberg’s Arch Pharmacol (2008) 378:371–394 DOI 10.1007/s00210-008-0322-7 REVIEW Current and prospective pharmacological targets in relation to antimigraine action Suneet Mehrotra & Saurabh Gupta & Kayi Y. Chan & Carlos M. Villalón & David Centurión & Pramod R. Saxena & Antoinette MaassenVanDenBrink Received: 8 January 2008 /Accepted: 6 June 2008 /Published online: 15 July 2008 # The Author(s) 2008 Abstract Migraine is a recurrent incapacitating neuro- (CGRP1 and CGRP2), adenosine (A1,A2,andA3), glutamate vascular disorder characterized by unilateral and throbbing (NMDA, AMPA, kainate, and metabotropic), dopamine, headaches associated with photophobia, phonophobia, endothelin, and female hormone (estrogen and progesterone) nausea, and vomiting. Current specific drugs used in the receptors. In addition, we have considered some other acute treatment of migraine interact with vascular receptors, targets, including gamma-aminobutyric acid, angiotensin, a fact that has raised concerns about their cardiovascular bradykinin, histamine, and ionotropic receptors, in relation to safety. In the past, α-adrenoceptor agonists (ergotamine, antimigraine therapy. Finally, the cardiovascular safety of dihydroergotamine, isometheptene) were used. The last two current and prospective antimigraine therapies is touched decades have witnessed the advent of 5-HT1B/1D receptor upon. agonists (sumatriptan and second-generation triptans), which have a well-established efficacy in the acute Keywords 5-HT. Antimigraine drugs . CGRP. treatment of migraine. Moreover, current prophylactic Noradrenaline . Migraine . Receptors treatments of migraine include 5-HT2 receptor antagonists, Ca2+ channel blockers, and β-adrenoceptor antagonists. Despite the progress in migraine research and in view of its Introduction complex etiology, this disease still remains underdiagnosed, and available therapies are underused. -

Single-Cell RNA Sequencing Demonstrates the Molecular and Cellular Reprogramming of Metastatic Lung Adenocarcinoma
ARTICLE https://doi.org/10.1038/s41467-020-16164-1 OPEN Single-cell RNA sequencing demonstrates the molecular and cellular reprogramming of metastatic lung adenocarcinoma Nayoung Kim 1,2,3,13, Hong Kwan Kim4,13, Kyungjong Lee 5,13, Yourae Hong 1,6, Jong Ho Cho4, Jung Won Choi7, Jung-Il Lee7, Yeon-Lim Suh8,BoMiKu9, Hye Hyeon Eum 1,2,3, Soyean Choi 1, Yoon-La Choi6,10,11, Je-Gun Joung1, Woong-Yang Park 1,2,6, Hyun Ae Jung12, Jong-Mu Sun12, Se-Hoon Lee12, ✉ ✉ Jin Seok Ahn12, Keunchil Park12, Myung-Ju Ahn 12 & Hae-Ock Lee 1,2,3,6 1234567890():,; Advanced metastatic cancer poses utmost clinical challenges and may present molecular and cellular features distinct from an early-stage cancer. Herein, we present single-cell tran- scriptome profiling of metastatic lung adenocarcinoma, the most prevalent histological lung cancer type diagnosed at stage IV in over 40% of all cases. From 208,506 cells populating the normal tissues or early to metastatic stage cancer in 44 patients, we identify a cancer cell subtype deviating from the normal differentiation trajectory and dominating the metastatic stage. In all stages, the stromal and immune cell dynamics reveal ontological and functional changes that create a pro-tumoral and immunosuppressive microenvironment. Normal resident myeloid cell populations are gradually replaced with monocyte-derived macrophages and dendritic cells, along with T-cell exhaustion. This extensive single-cell analysis enhances our understanding of molecular and cellular dynamics in metastatic lung cancer and reveals potential diagnostic and therapeutic targets in cancer-microenvironment interactions. 1 Samsung Genome Institute, Samsung Medical Center, Seoul 06351, Korea. -
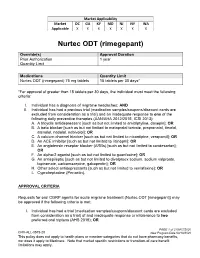
Nurtec ODT (Rimegepant)
Market Applicability Market DC GA KY MD NJ NY WA Applicable X X X X X X X Nurtec ODT (rimegepant) Override(s) Approval Duration Prior Authorization 1 year Quantity Limit Medications Quantity Limit Nurtec ODT (rimegepant) 75 mg tablets 15 tablets per 30 days* *For approval of greater than 15 tablets per 30 days, the individual must meet the following criteria: I. Individual has a diagnosis of migraine headaches; AND II. Individual has had a previous trial (medication samples/coupons/discount cards are excluded from consideration as a trial) and an inadequate response to one of the following daily preventive therapies (AAN/AHA 2012/2015, ICSI 2013): A. A tricyclic antidepressant [such as but not limited to amitriptyline, doxepin]; OR B. A beta blocker [such as but not limited to metoprolol tartrate, propranolol, timolol, atenolol, nadolol, nebivolol]; OR C. A calcium channel blocker [such as but not limited to nicardipine, verapamil]; OR D. An ACE inhibitor [such as but not limited to lisinopril]; OR E. An angiotensin receptor blocker (ARBs) [such as but not limited to candesartan]; OR F. An alpha-2 agonist [such as but not limited to guanfacine]; OR G. An antiepileptic [such as but not limited to divalproex sodium, sodium valproate, topiramate, carbamazepine, gabapentin]; OR H. Other select antidepressants [such as but not limited to venlafaxine]; OR I. Cyproheptadine (Periactin). APPROVAL CRITERIA Requests for oral CGRP agents for acute migraine treatment (Nurtec ODT [rimegepant]) may be approved if the following criteria is met: I. Individual has had a trial (medication samples/coupons/discount cards are excluded from consideration as a trial) of and inadequate response or intolerance to two preferred oral triptans (AHS 2019); OR PAGE 1 of 2 08/07/2020 CRX-ALL-0575-20 New Program Date 03/19/2020 This policy does not apply to health plans or member categories that do not have pharmacy benefits, nor does it apply to Medicare. -
Amitriptyline-Mediated Cognitive Enhancement in Aged 36Tg Alzheimer’S Disease Mice Is Associated with Neurogenesis and Neurotrophic Activity
Amitriptyline-Mediated Cognitive Enhancement in Aged 36Tg Alzheimer’s Disease Mice Is Associated with Neurogenesis and Neurotrophic Activity Wayne Chadwick1, Nick Mitchell2, Jenna Caroll3, Yu Zhou1, Sung-Soo Park1, Liyun Wang1, Kevin G. Becker4, Yongqing Zhang4, Elin Lehrmann4, William H. Wood III4, Bronwen Martin5, Stuart Maudsley1* 1 Receptor Pharmacology Unit, National Institute on Aging, National Institutes of Health, Baltimore, Maryland, United States of America, 2 Laboratory of Neurosciences, National Institute on Aging, National Institutes of Health, Baltimore, Maryland, United States of America, 3 Center for Neurodegenerative Disease Research, University of Pennsylvania, Philadelphia, Pennsylvania, United States of America, 4 Genomics Unit, Research Resources Branch, National Institute on Aging, National Institutes of Health, Baltimore, Maryland, United States of America, 5 Metabolism Unit, National Institute on Aging, National Institutes of Health, Baltimore, Maryland, United States of America Abstract Approximately 35 million people worldwide suffer from Alzheimer’s disease (AD). Existing therapeutics, while moderately effective, are currently unable to stem the widespread rise in AD prevalence. AD is associated with an increase in amyloid beta (Ab) oligomers and hyperphosphorylated tau, along with cognitive impairment and neurodegeneration. Several antidepressants have shown promise in improving cognition and alleviating oxidative stress in AD but have failed as long- term therapeutics. In this study, amitriptyline, an FDA-approved tricyclic antidepressant, was administered orally to aged and cognitively impaired transgenic AD mice (36TgAD). After amitriptyline treatment, cognitive behavior testing demonstrated that there was a significant improvement in both long- and short-term memory retention. Amitriptyline treatment also caused a significant potentiation of non-toxic Ab monomer with a concomitant decrease in cytotoxic dimer Ab load, compared to vehicle-treated 36TgAD controls. -

Constitutive Activation of G Protein-Coupled Receptors and Diseases: Insights Into Mechanisms of Activation and Therapeutics
Pharmacology & Therapeutics 120 (2008) 129–148 Contents lists available at ScienceDirect Pharmacology & Therapeutics journal homepage: www.elsevier.com/locate/pharmthera Associate editor: S. Enna Constitutive activation of G protein-coupled receptors and diseases: Insights into mechanisms of activation and therapeutics Ya-Xiong Tao ⁎ Department of Anatomy, Physiology and Pharmacology, 212 Greene Hall, College of Veterinary Medicine, Auburn University, Auburn, AL 36849, USA article info abstract The existence of constitutive activity for G protein-coupled receptors (GPCRs) was first described in 1980s. In Keywords: 1991, the first naturally occurring constitutively active mutations in GPCRs that cause diseases were reported G protein-coupled receptor Disease in rhodopsin. Since then, numerous constitutively active mutations that cause human diseases were reported Constitutively active mutation in several additional receptors. More recently, loss of constitutive activity was postulated to also cause Inverse agonist diseases. Animal models expressing some of these mutants confirmed the roles of these mutations in the Mechanism of activation pathogenesis of the diseases. Detailed functional studies of these naturally occurring mutations, combined Transgenic model with homology modeling using rhodopsin crystal structure as the template, lead to important insights into the mechanism of activation in the absence of crystal structure of GPCRs in active state. Search for inverse Abbreviations: agonists on these receptors will be critical for correcting the diseases cause by activating mutations in GPCRs. ADRP, autosomal dominant retinitis pigmentosa Theoretically, these inverse agonists are better therapeutics than neutral antagonists in treating genetic AgRP, Agouti-related protein AR, adrenergic receptor diseases caused by constitutively activating mutations in GPCRs. CAM, constitutively active mutant © 2008 Elsevier Inc. -

Gene Standard Deviation MTOR 0.12553731 PRPF38A
BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) Gut Gene Standard Deviation MTOR 0.12553731 PRPF38A 0.141472605 EIF2B4 0.154700091 DDX50 0.156333027 SMC3 0.161420017 NFAT5 0.166316903 MAP2K1 0.166585267 KDM1A 0.16904912 RPS6KB1 0.170330192 FCF1 0.170391706 MAP3K7 0.170660513 EIF4E2 0.171572093 TCEB1 0.175363093 CNOT10 0.178975095 SMAD1 0.179164705 NAA15 0.179904998 SETD2 0.180182498 HDAC3 0.183971158 AMMECR1L 0.184195031 CHD4 0.186678211 SF3A3 0.186697697 CNOT4 0.189434633 MTMR14 0.189734199 SMAD4 0.192451524 TLK2 0.192702667 DLG1 0.19336621 COG7 0.193422331 SP1 0.194364189 PPP3R1 0.196430217 ERBB2IP 0.201473001 RAF1 0.206887192 CUL1 0.207514271 VEZF1 0.207579584 SMAD3 0.208159809 TFDP1 0.208834504 VAV2 0.210269344 ADAM17 0.210687138 SMURF2 0.211437666 MRPS5 0.212428684 TMUB2 0.212560675 SRPK2 0.216217428 MAP2K4 0.216345366 VHL 0.219735582 SMURF1 0.221242495 PLCG1 0.221688351 EP300 0.221792349 Sundar R, et al. Gut 2020;0:1–10. doi: 10.1136/gutjnl-2020-320805 BMJ Publishing Group Limited (BMJ) disclaims all liability and responsibility arising from any reliance Supplemental material placed on this supplemental material which has been supplied by the author(s) Gut MGAT5 0.222050228 CDC42 0.2230598 DICER1 0.225358787 RBX1 0.228272533 ZFYVE16 0.22831803 PTEN 0.228595789 PDCD10 0.228799406 NF2 0.23091035 TP53 0.232683696 RB1 0.232729172 TCF20 0.2346075 PPP2CB 0.235117302 AGK 0.235416298 -
Neurotransmitter and Neuropeptide Regulation of Mast Cell Function
Xu et al. Journal of Neuroinflammation (2020) 17:356 https://doi.org/10.1186/s12974-020-02029-3 REVIEW Open Access Neurotransmitter and neuropeptide regulation of mast cell function: a systematic review Huaping Xu1, Xiaoyun Shi2, Xin Li3, Jiexin Zou4, Chunyan Zhou5, Wenfeng Liu5, Huming Shao5, Hongbing Chen5 and Linbo Shi4* Abstract The existence of the neural control of mast cell functions has long been proposed. Mast cells (MCs) are localized in association with the peripheral nervous system (PNS) and the brain, where they are closely aligned, anatomically and functionally, with neurons and neuronal processes throughout the body. They express receptors for and are regulated by various neurotransmitters, neuropeptides, and other neuromodulators. Consequently, modulation provided by these neurotransmitters and neuromodulators allows neural control of MC functions and involvement in the pathogenesis of mast cell–related disease states. Recently, the roles of individual neurotransmitters and neuropeptides in regulating mast cell actions have been investigated extensively. This review offers a systematic review of recent advances in our understanding of the contributions of neurotransmitters and neuropeptides to mast cell activation and the pathological implications of this regulation on mast cell–related disease states, though the full extent to which such control influences health and disease is still unclear, and a complete understanding of the mechanisms underlying the control is lacking. Future validation of animal and in vitro models also is needed, which incorporates the integration of microenvironment-specific influences and the complex, multifaceted cross-talk between mast cells and various neural signals. Moreover, new biological agents directed against neurotransmitter receptors on mast cells that can be used for therapeutic intervention need to be more specific, which will reduce their ability to support inflammatory responses and enhance their potential roles in protecting against mast cell–related pathogenesis. -

I AMYLIN MEDIATES BRAINSTEM
AMYLIN MEDIATES BRAINSTEM CONTROL OF HEART RATE IN THE DIVING REFLEX A Dissertation Submitted to The Temple University Graduate Board In Partial Fulfillment of the Requirements for the Degree of Doctor of Philosophy By Fan Yang May, 2012 Examination committee members: Dr. Nae J Dun (advisor), Dept. of Pharmacology, Temple University Dr. Alan Cowan, Dept. of Pharmacology, Temple University Dr. Lee-Yuan Liu-Chen, Dept. of Pharmacology, Temple University Dr. Gabriela Cristina Brailoiu, Dept. of Pharmacology, Temple University Dr. Parkson Lee-Gau Chong, Dept. of Biochemistry, Temple University Dr. Hreday Sapru (external examiner), Depts. of Neurosciences, Neurosurgery & Pharmacology/Physiology, UMDNJ-NJMS. i © 2012 By Fan Yang All Rights Reserved ii ABSTRACT AMYLIN’S ROLE AS A NEUROPEPTIDE IN THE BRAINSTEM Fan Yang Doctor of Philosophy Temple University, 2012 Doctoral Advisory Committee Chair: Nae J Dun, Ph.D. Amylin, or islet amyloid polypeptide is a 37-amino acid member of the calcitonin peptide family. Amylin role in the brainstem and its function in regulating heart rates is unknown. The diving reflex is a powerful autonomic reflex, however no neuropeptides have been described to modulate its function. In this thesis study, amylin expression in the brainstem involving pathways between the trigeminal ganglion and the nucleus ambiguus was visualized and characterized using immunohistochemistry. Its functional role in slowing heart rate and also its involvement in the diving reflex were elucidated using stereotaxic microinjection, whole-cel patch-clamp, and a rat diving model. Immunohistochemical and tract tracing studies in rats revealed amylin expression in trigeminal ganglion cells, which also contained vesicular glutamate transporter 2 positive. -

G Protein-Coupled Receptors: What a Difference a ‘Partner’ Makes
Int. J. Mol. Sci. 2014, 15, 1112-1142; doi:10.3390/ijms15011112 OPEN ACCESS International Journal of Molecular Sciences ISSN 1422-0067 www.mdpi.com/journal/ijms Review G Protein-Coupled Receptors: What a Difference a ‘Partner’ Makes Benoît T. Roux 1 and Graeme S. Cottrell 2,* 1 Department of Pharmacy and Pharmacology, University of Bath, Bath BA2 7AY, UK; E-Mail: [email protected] 2 Reading School of Pharmacy, University of Reading, Reading RG6 6UB, UK * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +44-118-378-7027; Fax: +44-118-378-4703. Received: 4 December 2013; in revised form: 20 December 2013 / Accepted: 8 January 2014 / Published: 16 January 2014 Abstract: G protein-coupled receptors (GPCRs) are important cell signaling mediators, involved in essential physiological processes. GPCRs respond to a wide variety of ligands from light to large macromolecules, including hormones and small peptides. Unfortunately, mutations and dysregulation of GPCRs that induce a loss of function or alter expression can lead to disorders that are sometimes lethal. Therefore, the expression, trafficking, signaling and desensitization of GPCRs must be tightly regulated by different cellular systems to prevent disease. Although there is substantial knowledge regarding the mechanisms that regulate the desensitization and down-regulation of GPCRs, less is known about the mechanisms that regulate the trafficking and cell-surface expression of newly synthesized GPCRs. More recently, there is accumulating evidence that suggests certain GPCRs are able to interact with specific proteins that can completely change their fate and function. These interactions add on another level of regulation and flexibility between different tissue/cell-types. -

Supplementary Table S4. FGA Co-Expressed Gene List in LUAD
Supplementary Table S4. FGA co-expressed gene list in LUAD tumors Symbol R Locus Description FGG 0.919 4q28 fibrinogen gamma chain FGL1 0.635 8p22 fibrinogen-like 1 SLC7A2 0.536 8p22 solute carrier family 7 (cationic amino acid transporter, y+ system), member 2 DUSP4 0.521 8p12-p11 dual specificity phosphatase 4 HAL 0.51 12q22-q24.1histidine ammonia-lyase PDE4D 0.499 5q12 phosphodiesterase 4D, cAMP-specific FURIN 0.497 15q26.1 furin (paired basic amino acid cleaving enzyme) CPS1 0.49 2q35 carbamoyl-phosphate synthase 1, mitochondrial TESC 0.478 12q24.22 tescalcin INHA 0.465 2q35 inhibin, alpha S100P 0.461 4p16 S100 calcium binding protein P VPS37A 0.447 8p22 vacuolar protein sorting 37 homolog A (S. cerevisiae) SLC16A14 0.447 2q36.3 solute carrier family 16, member 14 PPARGC1A 0.443 4p15.1 peroxisome proliferator-activated receptor gamma, coactivator 1 alpha SIK1 0.435 21q22.3 salt-inducible kinase 1 IRS2 0.434 13q34 insulin receptor substrate 2 RND1 0.433 12q12 Rho family GTPase 1 HGD 0.433 3q13.33 homogentisate 1,2-dioxygenase PTP4A1 0.432 6q12 protein tyrosine phosphatase type IVA, member 1 C8orf4 0.428 8p11.2 chromosome 8 open reading frame 4 DDC 0.427 7p12.2 dopa decarboxylase (aromatic L-amino acid decarboxylase) TACC2 0.427 10q26 transforming, acidic coiled-coil containing protein 2 MUC13 0.422 3q21.2 mucin 13, cell surface associated C5 0.412 9q33-q34 complement component 5 NR4A2 0.412 2q22-q23 nuclear receptor subfamily 4, group A, member 2 EYS 0.411 6q12 eyes shut homolog (Drosophila) GPX2 0.406 14q24.1 glutathione peroxidase