Effects of Antidepressants
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Still the Leading Antidepressant After 40
BRITISH JOURNAL OF PSYCHIATRY "2001), 178, 129^144 REVIEW ARTICLE Amitriptyline vv.therest:stilltheleading METHOD Inclusion criteria antidepressant after 40 years of randomised All RCTs comparing amitriptyline with any y other tricyclic,heterocyclic or SSRI were in- controlled trials cluded. Crossover studies were excluded. Studies adopting any criteria to define CORRADO BARBUI and MATTHEW HOTOPF patients suffering from depression were included; a concurrent diagnosis of another psychiatric disorder was not considered an exclusion criterion. Trials in patients with depression with a concomitant medical ill- Background Tricyclic antidepressants Amitriptyline is one of the first `reference' ness were not included in this review. have similar efficacy and slightly lower tricyclic antidepressants TCAs). Over the past 40 years a number of newer tricyclics, tolerability than selective serotonin Search strategy heterocyclics and selective serotonin re- Relevant studies were located by searching reuptakeinhibitorsreuptake inhibitors SSRIs).However, uptake inhibitors SSRIs) have been intro- the Cochrane Collaboration Depression, there are no systematic reviews assessing duced Garattini et aletal,1998). Despite Anxiety and Neurosis Controlled Trials several large systematic reviews comparing amitriptyline, the reference tricyclic drug, Register CCDANCTR). This specialised tricyclics and SSRIs there is no clear agree- vv. other tricyclics and SSRIs directly. register is regularly updated by electronic ment over first-line treatment of depression Medline,Embase,PsycINFO,LILACS, SongSong et aletal,1993; Anderson & Tomenson, Aims ToreviewTo review the tolerability and Psyndex,CINAHL,SIGLE) and non-electro- 1995; Montgomery & Kasper,1995; efficacy of amitriptyline inthe nicnicliterature searches. The register was HotopfHotopf et aletal,1996; Canadian Coordinating management of depression. searched using the following terms: Office for Health Technology Assessment, AMITRIPTYLIN**AMITRIPTYLIN oror AMITRILAMITRIL oror ELA-ELA- 19971997aa). -
Unlicensed Medicines List for Suffolk D&T
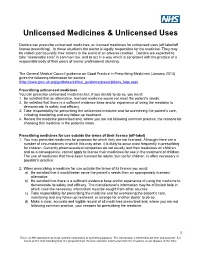
Unlicensed Medicines & Unlicensed Uses Doctors can prescribe unlicensed medicines, or licensed medicines for unlicensed uses (off-label/off license prescribing). In these situations the doctor is legally responsible for the medicine. They may be called upon to justify their actions in the event of an adverse reaction. Doctors are expected to take “reasonable care” in common law, and to act in a way which is consistent with the practice of a responsible body of their peers of similar professional standing. The General Medical Council guidance on Good Practice in Prescribing Medicines (January 2013) gives the following information for doctors (http://www.gmc-uk.org/guidance/ethical_guidance/prescriptions_faqs.asp) Prescribing unlicensed medicines You can prescribe unlicensed medicines but, if you decide to do so, you must: 1. Be satisfied that an alternative, licensed medicine would not meet the patient's needs. 2. Be satisfied that there is a sufficient evidence base and/or experience of using the medicine to demonstrate its safety and efficacy. 3. Take responsibility for prescribing the unlicensed medicine and for overseeing the patient's care, including monitoring and any follow up treatment. 4. Record the medicine prescribed and, where you are not following common practice, the reasons for choosing this medicine in the patient's notes. Prescribing medicines for use outside the terms of their licence (off-label) 1. You may prescribe medicines for purposes for which they are not licensed. Although there are a number of circumstances in which this may arise, it is likely to occur most frequently in prescribing for children. Currently pharmaceutical companies do not usually test their medicines on children and as a consequence, cannot apply to license their medicines for use in the treatment of children. -

Neuroenhancement in Healthy Adults, Part I: Pharmaceutical
l Rese ca arc ni h li & C f B o i o l e Journal of a t h n Fond et al., J Clinic Res Bioeth 2015, 6:2 r i c u s o J DOI: 10.4172/2155-9627.1000213 ISSN: 2155-9627 Clinical Research & Bioethics Review Article Open Access Neuroenhancement in Healthy Adults, Part I: Pharmaceutical Cognitive Enhancement: A Systematic Review Fond G1,2*, Micoulaud-Franchi JA3, Macgregor A2, Richieri R3,4, Miot S5,6, Lopez R2, Abbar M7, Lancon C3 and Repantis D8 1Université Paris Est-Créteil, Psychiatry and Addiction Pole University Hospitals Henri Mondor, Inserm U955, Eq 15 Psychiatric Genetics, DHU Pe-psy, FondaMental Foundation, Scientific Cooperation Foundation Mental Health, National Network of Schizophrenia Expert Centers, F-94000, France 2Inserm 1061, University Psychiatry Service, University of Montpellier 1, CHU Montpellier F-34000, France 3POLE Academic Psychiatry, CHU Sainte-Marguerite, F-13274 Marseille, Cedex 09, France 4 Public Health Laboratory, Faculty of Medicine, EA 3279, F-13385 Marseille, Cedex 05, France 5Inserm U1061, Idiopathic Hypersomnia Narcolepsy National Reference Centre, Unit of sleep disorders, University of Montpellier 1, CHU Montpellier F-34000, Paris, France 6Inserm U952, CNRS UMR 7224, Pierre and Marie Curie University, F-75000, Paris, France 7CHU Carémeau, University of Nîmes, Nîmes, F-31000, France 8Department of Psychiatry, Charité-Universitätsmedizin Berlin, Campus Benjamin Franklin, Eschenallee 3, 14050 Berlin, Germany *Corresponding author: Dr. Guillaume Fond, Pole de Psychiatrie, Hôpital A. Chenevier, 40 rue de Mesly, Créteil F-94010, France, Tel: (33)178682372; Fax: (33)178682381; E-mail: [email protected] Received date: January 06, 2015, Accepted date: February 23, 2015, Published date: February 28, 2015 Copyright: © 2015 Fond G, et al. -

Treatment of Relapsing Malaria with Specific Antimalarial Drugs In
Sept., 1947 J TREATMENT OF RELAPSING MALARIA: DESHMUKH 511 up to the expectation. But it soon became Articles clear that they did not control relapse, and Original also that they carry with them a danger of toxicity. Arsenic is notorious for causing to TREATMENT of relapsing malaria damage liver, kidneys and brain. When pregnancy complicates malaria, the use of WITH SPECIFIC ANTIMALARIAL quinine and arsenic may be particularly risky DRUGS IN COMBINATION WITH and one is on the horns of a dilemma as regards PENICILLIN the satisfactory treatment in such circumstances. The writer's experience of arsenicals in By P. L. DESHMUKH, m.d. (Bom.), malaria has been borne out other workers F.C.P.S. by D.T.M.\& II. (Lond.), and their findings in large-scale experiments Poona Sassoon Hospitals, given below will help to dislodge from the minds It must be admitted that even with quinine of the clinicians any lingering faith in arsenic and the synthetic antimalarial drugs like as an ideal antimalarial drug. atabrine, mepacrine, etc. (henceforth called Professor Blacklock (1944) has pointed out specific antimalarials ' for the sake of after long studies at the Liverpool school that tee brevity) treatment of malaria is still very unsatis- though the immediate effects of arsenic in factory. The recognized failure of the specific relapsing malaria were striking, the ultimate antimalarials singly or in combination to control results were disappointing in that practically relapses materially is a matter of great all cases relapsed even after full arsenical concern. A great variation is observed in the treatment. Thus, arsenicals though immediately mterval that may before the occurrence effective against vivax parasites do not eliminate a elapse y relapse. -

Still the Leading Antidepressant After 40 Years of Randomised Controlle
BRITISH JOURNAL OF PSYCHIATRY "2001), 178, 129^144 REVIEW ARTICLE Amitriptyline vv.therest:stilltheleading METHOD Inclusion criteria antidepressant after 40 years of randomised All RCTs comparing amitriptyline with any y other tricyclic,heterocyclic or SSRI were in- controlled trials cluded. Crossover studies were excluded. Studies adopting any criteria to define CORRADO BARBUI and MATTHEW HOTOPF patients suffering from depression were included; a concurrent diagnosis of another psychiatric disorder was not considered an exclusion criterion. Trials in patients with depression with a concomitant medical ill- Background Tricyclic antidepressants Amitriptyline is one of the first `reference' ness were not included in this review. have similar efficacy and slightly lower tricyclic antidepressants TCAs). Over the past 40 years a number of newer tricyclics, tolerability than selective serotonin Search strategy heterocyclics and selective serotonin re- Relevant studies were located by searching reuptakeinhibitorsreuptake inhibitors SSRIs).However, uptake inhibitors SSRIs) have been intro- the Cochrane Collaboration Depression, there are no systematic reviews assessing duced Garattini et aletal,1998). Despite Anxiety and Neurosis Controlled Trials several large systematic reviews comparing amitriptyline, the reference tricyclic drug, Register CCDANCTR). This specialised tricyclics and SSRIs there is no clear agree- vv. other tricyclics and SSRIs directly. register is regularly updated by electronic ment over first-line treatment of depression Medline,Embase,PsycINFO,LILACS, SongSong et aletal,1993; Anderson & Tomenson, Aims ToreviewTo review the tolerability and Psyndex,CINAHL,SIGLE) and non-electro- 1995; Montgomery & Kasper,1995; efficacy of amitriptyline inthe nicnicliterature searches. The register was HotopfHotopf et aletal,1996; Canadian Coordinating management of depression. searched using the following terms: Office for Health Technology Assessment, AMITRIPTYLIN**AMITRIPTYLIN oror AMITRILAMITRIL oror ELA-ELA- 19971997aa). -

Traxoprodil, a Selective Antagonist of the NR2B Subunit of the NMDA
Metab Brain Dis (2016) 31:803–814 DOI 10.1007/s11011-016-9810-5 ORIGINAL ARTICLE Traxoprodil, a selective antagonist of the NR2B subunit of the NMDA receptor, potentiates the antidepressant-like effects of certain antidepressant drugs in the forced swim test in mice Ewa Poleszak1 & Weronika Stasiuk 2 & Aleksandra Szopa1 & Elżbieta Wyska3 & Anna Serefko1 & Anna Oniszczuk4 & Sylwia Wośko 1 & Katarzyna Świąder1 & Piotr Wlaź5 Received: 25 November 2015 /Accepted: 17 February 2016 /Published online: 29 February 2016 # The Author(s) 2016. This article is published with open access at Springerlink.com Abstract One of the newest substances, whose antidepres- these changes were not due to the severity of locomotor ac- sant activity was shown is traxoprodil, which is a selective tivity. The observed effect of traxoprodil is only partially as- antagonist of the NR2B subunit of the NMDA receptor. The sociated with serotonergic system and is independent of the main goal of the present study was to evaluate the effect of effect on the 5-HT1A and 5-HT2 serotonin receptors. The re- traxoprodil on animals’ behavior using the forced swim test sults of an attempt to assess the nature of the interaction be- (FST), as well as the effect of traxoprodil (10 mg/kg) on the tween traxoprodil and the tested drugs show that in the case of activity of antidepressants, such as imipramine (15 mg/kg), joint administration of traxoprodil and fluoxetine, imip- fluoxetine (5 mg/kg), escitalopram (2 mg/kg) and reboxetine ramine or escitalopram, there were interactions in the (2.5 mg/kg). Serotonergic lesion and experiment using the pharmacokinetic phase. -

Tcas Versus Placebo - New Studies in the Guideline Update
TCAs versus placebo - new studies in the guideline update Comparisons Included in this Clinical Question Amitriptyline vs placebo Clomipramine vs placebo Dosulepin (dothiepin) vs placebo AMSTERDAM2003A LARSEN1989 FERGUSON1994B BAKISH1992B PECKNOLD1976B ITIL1993 BAKISH1992C RAMPELLO1991 MINDHAM1991 BREMNER1995 THOMPSON2001B CLAGHORN1983 CLAGHORN1983B FEIGHNER1979 GELENBERG1990 GEORGOTAS1982A GOLDBERG1980 HICKS1988 HOLLYMAN1988 HORMAZABAL1985 HOSCHL1989 KLIESER1988 LAAKMAN1995 LAPIERRE1991 LYDIARD1997 MYNORSWALLIS1995 MYNORSWALLIS1997 REIMHERR1990 RICKELS1982D RICKELS1985 RICKELS1991 ROFFMAN1982 ROWAN1982 SMITH1990 SPRING1992 STASSEN1993 WILCOX1994 16 Imipramine vs placebo BARGESCHAAPVELD2002 BEASLEY1991B BOYER1996A BYERLEY1988 CASSANO1986 CASSANO1996 CLAGHORN1996A COHN1984 COHN1985 COHN1990A COHN1992 COHN1996 DOMINGUEZ1981 DOMINGUEZ1985 DUNBAR1991 ELKIN1989 ENTSUAH1994 ESCOBAR1980 FABRE1980 FABRE1992 FABRE1996 FEIGER1996A FEIGHNER1980 FEIGHNER1982 FEIGHNER1983A FEIGHNER1983B FEIGHNER1989 FEIGHNER1989A FEIGHNER1989B FEIGHNER1989C FEIGHNER1992B FEIGHNER1993 FONTAINE1994 GELENBERG2002 GERNER1980B HAYES1983 ITIL1983A KASPER1995B KELLAMS1979 LAIRD1993 LAPIERRE1987 LECRUBIER1997B LIPMAN1986 LYDIARD1989 MARCH1990 17 MARKOWITZ1985 MENDELS1986 MERIDETH1983 Nortriptyline vs placebo NANDI1976 GEORGOTAS1986A NORTON1984 KATZ1990 PEDERSEN2002 NAIR1995 PESELOW1989 WHITE1984A PESELOW1989B PHILIPP1999 QUITKIN1989 RICKELS1981 RICKELS1982A RICKELS1987 SCHWEIZER1994 SCHWEIZER1998 SHRIVASTAVA1992 SILVERSTONE1994 SMALL1981 UCHA1990 VERSIANI1989 VERSIANI1990 -

Light Sensitive Eruptions Treated with Atabrine and Chloroquine John M
LIGHT SENSITIVE ERUPTIONS TREATED WITH ATABRINE AND CHLOROQUINE JOHN M. KNOX, M.D.,JOHNH. LAMB,Ml)., BEDFORDSHELMIRE, M.D.,AND ROBERT J. MORGAN, M.D. In April 1951 a 50-year-old female, a Red Cross worker recently returned from India, came to one of us (J. M. K.) at Keesler Air Force Base, Biloxi, Mississippi. While in India she had taken atabrine for its antimalarial action. During the period that her skin was yellowed by atabrine pigmentation she had noticed a conspicuous decrease in the severity of a long-standing light-sensitive eruption, prurigo aestivale. The annoying disease was beginning to reappear arid she preferred a return of the yellow discoloration to the eruption. Her response tG atabrine was so noteworthy that later a man 28 years of age with a plaque-like, light-sensitive eruption of the face was given a similar therapeutic trial with the same success. The improvement noted in these two cases, plus the appearance of reports by Page (la) and others (ib, c, d) on atabrine in discoid lupus erythematosus encouraged a clinical evaluation of this drug for the treatment of light-sensitive eruptions. Black (2), in a report of the use of mepacrine in lupus erythematosus, tested four patients with actinic dermatitis with this preparation. No description of the types of dermatitis was recorded. Two female patients were cleared; they had had the disease each summer for 11 and 30 years respectively. The condition of the other two patients (who were males) was unaltered by this drug. DISCUSSION Figure 1 gives a summary of the 18 cases of various types of solar dermatitis. -

Resume of Scientific Contributions to Psychopharmacology And
RESUME OF SCIENTIFIC CONTRIBUTIONS TO PSYCHOPHARMACOLOGY AND BIOLOGICAL PSYCHIATRY While Fridolin Sulser was a visiting scientist from Switzerland in the Laboratory of Chemical Pharmacology at the National Institutes of Health in Bethesda, Maryland, he and B.B. Brodie utilized the reserpine-like syndrome as a "model depression" and in due course discovered the secondary amine desmethyl-imipramine (DM1) formed in vivo by oxidative N-demethylation of imipramine (1,2).DMI turned out to be the first selective inhibitor of the high affinity uptake of norepinephrine and triggered the development of many secondary amines of tricyclic antidepressants as therapeutic agents (e.g. desipramine, nortriptyline, protriptyline maprotiline, oxaprotiline, and more recently reboxetine). These drugs provided more selective pharmacologic tools to dissect the role of central noradrenergic mechanisms (3). During the early 1970s, Fridolin Sulser and his associates discovered that treatment with antidepressants on a clinically relevant time basis (including tricyclics, 4- Fridolin Sulser, M.D. Curriculum Vitae MAO inhibitors, some atypical antidepressants and electroconvulsive treatment) reduces selectively the responsiveness of the norepinephrine (NE) beta adrenoceptor coupled adenylate cyclase system in limbic and cortical structures of the rat brain (4,5). This deamplification of the central beta adrenoceptor system is often linked to a down- regulation of the Brnax value of beta adrenoceptors, without changes in the KD. These findings shifted the research emphasis on the mode of action of antidepressant treatments and on the pathophysiology of affective disorders from acute presynaptic to delayed post-synaptic receptor - second messenger mediated events and emphasized the role of adaptive processes at the level of signal transduction and opened the gateway for subsequent studies on changes of programs of gene expression. -

有限公司 API Antineoplastic Agents
® 伊域化學藥業(香港)有限公司 YICK-VIC CHEMICALS & PHARMACEUTICALS (HK) LTD Rm 1006, 10/F, Hewlett Centre, Tel: (852) 25412772 (4 lines) No. 52-54, Hoi Yuen Road, Fax: (852) 25423444 / 25420530 / 21912858 Kwun Tong, E-mail: [email protected] YICK -VIC 伊域 Kowloon, Hong Kong. Site: http://www.yickvic.com API Antineoplastic Agents Product Highlight The following is a selection of products we have sourced and supplied to our customers globally. For detailed specifications, certificates of analysis, supply position, and tailored pricing, please contact us at [email protected] . For any unlisted products that you require, feel free to contact us for support. We can source or custom manufacture at your specification. Product Code CAS Product Name PH-3107DA 522-17-8 (-)-DEGUELIN PH-4360CF 989-51-5 (-)-EPIGALLOCATECHIN GALLATE MIS-6071 32981-86-5 10-DEACETYLBACCATIN III (REFERENCE GRADE) MIS-5741 78432-77-6 10-DEACETYLPACLITAXEL (REFERENCE GRADE) PH-0441BA 19685-09-7 10-HYDROXYCAMPTOTHECIN 64439-81-2 (UNSPECIFIED ISOMER) PH-0441BC 19685-09-7 10-HYDROXYCAMPTOTHECIN (REFERENCE GRADE) 64439-81-2 (UNSPECIFIED ISOMER) PH-3394A 533-67-5 2-DEOXY-D-RIBOSE PH-1956DA 951-78-0 2'-DEOXYURIDINE PH-0865F 38390-45-3 3',4'-ANHYDROVINBLASTINE MIS-10676 75567-37-2 3-INGENYL ANGELATE (REFERENCE GRADE) 849146-39-0 Copyright © 2020 YICK-VIC CHEMICALS & PHARMACEUTICALS (HK) LTD. All rights reserved. Page 1 of 57 Product Code CAS Product Name PH-1578EK 2498-50-2 4-AMINOBENZAMIDINE DIHYDROCHLORIDE PH-1541D 23363-35-1 4'-DEMETHYLEPIPODOPHYLLOTOXIN-9 BETA-GLUCOPYRANOSIDE PH-4586B 1716-12-7 -

Mepacrine Hydrochloride/Metronidazole
Mepacrine Hydrochloride/Metronidazole 837 mothorax but the treatment is associated with pain and a high Metronidazole Hydrochloride (BANM, USAN, rINNM) lung cancer, although all 4 were in women who were smokers. frequency of toxic effects. Subsequent follow-up4 to 1984, covering a period of 15 to 25 Hidrocloruro de metronidazol; Métronidazole, Chlorhydrate de; Preparations years, still showed an excess of lung cancer cases even after al- Metronidazoli Hydrochloridum; SC-32642. lowing for smoking status. However, this follow-up also contin- Proprietary Preparations (details are given in Part 3) Метронидазола Гидрохлорид ued to show no significant increase overall in cancer-related India: Maladin. 5 C6H9N3O3,HCl = 207.6. morbidity or mortality. Follow-up of the patients from the sec- CAS — 69198-10-3. ond study for 11 to 15 years to 1984 also showed no increase in ATC — A01AB17; D06BX01; G01AF01; J01XD01; the overall incidence of cancers nor did it confirm any increase Methyl Benzoquate (BAN) P01AB01. in lung cancer. ATC Vet — QA01AB17; QD06BX01; QG01AF01; Risks to the fetus are discussed under Pregnancy in Precautions, Nequinate (USAN, pINN); AY-20385; ICI-55052; Néquinate; Ne- QJ01XD01; QP51AA01. below. quinato; Nequinatum. Methyl 7-benzyloxy-6-butyl-1,4-dihydro- 1. Bendesky A, et al. Is metronidazole carcinogenic? Mutat Res 4-oxoquinoline-3-carboxylate. Incompatibility. Solutions of metronidazole hydrochloride have a low pH, usually of less than 2.0, before dilution and neu- 2002; 511: 133–44. Нехинат 2. Beard CM, et al. Lack of evidence for cancer due to use of met- tralisation for intravenous use. These undiluted solutions react ronidazole. N Engl J Med 1979; 301: 519–22. -

OUH Formulary Approved for Use in Breast Surgery
Oxford University Hospitals NHS Foundation Trust Formulary FORMULARY (Y): the medicine can be used as per its licence. RESTRICTED FORMULARY (R): the medicine can be used as per the agreed restriction. NON-FORMULARY (NF): the medicine is not on the formulary and should not be used unless exceptional approval has been obtained from MMTC. UNLICENSED MEDICINE – RESTRICTED FORMULARY (UNR): the medicine is unlicensed and can be used as per the agreed restriction. SPECIAL MEDICINE – RESTRICTED FORMULARY (SR): the medicine is a “special” (unlicensed) and can be used as per the agreed restriction. EXTEMPORANEOUS PREPARATION – RESTRICTED FORMULARY (EXTR): the extemporaneous preparation (unlicensed) can be prepared and used as per the agreed restriction. UNLICENSED MEDICINE – NON-FORMULARY (UNNF): the medicine is unlicensed and is not on the formulary. It should not be used unless exceptional approval has been obtained from MMTC. SPECIAL MEDICINE – NON-FORMULARY (SNF): the medicine is a “special” (unlicensed) and is not on the formulary. It should not be used unless exceptional approval has been obtained from MMTC. EXTEMPORANEOUS PREPARATION – NON-FORMULARY (EXTNF): the extemporaneous preparation (unlicensed) cannot be prepared and used unless exceptional approval has been obtained from MMTC. CLINICAL TRIALS (C): the medicine is clinical trial material and is not for clinical use. NICE TECHNOLOGY APPRAISAL (NICETA): the medicine has received a positive appraisal from NICE. It will be available on the formulary from the day the Technology Appraisal is published. Prescribers who wish to treat patients who meet NICE criteria, will have access to these medicines from this date. However, these medicines will not be part of routine practice until a NICE TA Implementation Plan has been presented and approved by MMTC (when the drug will be given a Restricted formulary status).