Vaccine Ordering Open
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Parish Profile
PPaarriisshh PPrrooffiillee Polbeth Harwood linked with West Kirk of Calder “Growing in faith and sharing our faith in God with the world around us to make way for Jesus in our community” Polbeth Harwood Church Chapelton Terrace Polbeth EH55 8SH West Kirk of Calder West End West Calder EH55 8EN Introduction The history of West Kirk goes as far back as Reformation times when the community of West Calder grew up around its kirk. The current traditionally Victorian church building was first open for worship in 1880 replacing the original kirk, the ruins of which still stand just behind the main street in the village. Polbeth Harwood congregation have recently celebrated 50 years of witness and worship in their more modern suite of sanctuary, hall and rooms –all paid for by community funding - in a position designed to be a focus of community life in the village. The linkage between the two churches was formed in 2003 and both Sessions are now actively discussing a closer working relationship with the exciting possibility of even closer involvement under the visionary leadership of a new minister. Whilst the West Kirk congregation are proud of their long past history, the Sessions hold the view that together the congregations are stronger and, with faith, more able to meet the challenges facing the Church and where and how God wants us to serve him in the 21st century. We seek a minister who can encourage us, nourish our faith and lead us in the direction God has mapped out for us as his servants. The two churches are only over a mile apart, both situated on A71. -
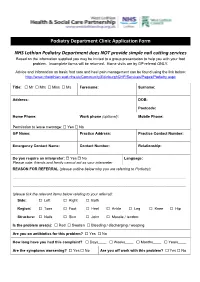
Podiatry Department Clinic Application Form NHS Lothian
Podiatry Department Clinic Application Form NHS Lothian Podiatry Department does NOT provide simple nail cutting services Based on the information supplied you may be invited to a group presentation to help you with your foot problem. Incomplete forms will be returned. Home visits are by GP referral ONLY. Advice and information on basic foot care and heel pain management can be found using the link below: http://www.nhslothian.scot.nhs.uk/Community/EdinburghCHP/Services/Pages/Podiatry.aspx Title: Mr Mrs Miss Ms Forename: Surname: Address: DOB: Postcode: Home Phone: Work phone (optional): Mobile Phone: Permission to leave message: Yes No GP Name: Practice Address: Practice Contact Number: Emergency Contact Name: Contact Number: Relationship: Do you require an interpreter: Yes No Language: Please note: friends and family cannot act as your interpreter REASON FOR REFERRAL (please outline below why you are referring to Podiatry): ......................................................................................................................................................................... ......................................................................................................................................................................... (please tick the relevant items below relating to your referral): Side: Left Right Both Region: Toes Foot Heel Ankle Leg Knee Hip Structure: Nails Skin Joint Muscle / tendon: Is the problem area(s): Red Swollen Bleeding / discharging / weeping Are you on -

NHS Lothian Sustainable Development Framework and Action Plan
In the face of climate change, the biggest threat to global health of the 21st century, we need to reassess and adapt to the challenge as an organisation and NHS Lothian as individuals within the organisation. Sustainable Development Framework and Action Plan This means understanding the impacts of climate change on health and illness, recognising that the NHS needs to be sustainable for future generations and Our Vision understanding the interdependence and opportunity of sustainability goals Our vision is to be a lead organisation in sustainable health care with all our such as those set out by the United Nations (UN). staff empowered to put sustainable healthcare at the heart of their practice. We will work with our partners and the communities we serve to put in place work practices, procurement systems and preventative interventions to minimise our environmental impact, protect the natural environment and enhance social value so that we are a sustainable service promoting good health and enhancing quality of life. Goals / strategic objectives 1. NHS Lothian will have zero carbon emissions by 2045 2. NHS Lothian will contribute to enhancing our natural environment 3. NHS Lothian will promote climate resilience and ensure that its services are The social, financial and environmental resources of the NHS are limited and adapted to climate change need to be used and managed sustainably. Environmental sustainability, good 4. NHS Lothian will ensure that sustainable development is embedded in all financial management and better, more equal health need to be driven forward its activities including governance and decision making, clinical practice, hand in hand. -

Hub South East Scotland Territory Annual Report 2016-2017
Hub South East Scotland Territory Annual Report 2016-2017 ‰ Hub South East: Your Development Partner of Choice Our achievements : 2010 onwards HUB PROJECTS VALUE OF VALUE IN SOUTH EAST SCOTLAND PROPORTION of CONSTRUCTION WORK PACKAGES AWARDED to £563m SCOTTISH SMEs £ 349 197m OPEN and OPERATIONAL NEW JOBS % £185m IN CONSTRUCTION created 87 £181m IN DEVELOPMENT GRADUATE & TRAINING EDUCATIONAL SUPPORT New and existing Site, School School and FE 290APPRENTICESHIP and FE Visits Work Placements and trainee places + + 27,000 3,300 Professional Employment persons days 110 including GRADUATES Figures correct at end July 2017 ‰ 2 ‰ Foreword – Chairs 4 ‰ Territory Programme Director’s Report 7 ‰ Hub South East Chief Executive’s Report 10 ‰ Projects Completed 13 ‰ Contents Under Construction 23 ‰ In Development 33 ‰ Strategic Support Services 39 ‰ Performance 43 ‰ Added Value through Hub South East 50 ‰ Abstract of Accounts 53 ‰ ‰ 3 ‰ Foreword Welcome to the 2016/17 Annual Report for the South East Territory, The Territory’s Strategic vision is to work together to provide enhanced local services covering the reporting period August 2016 to July 2017. and achieve tangible benefits for partners and communities in the Lothians and Borders and we have been making real headway in delivering it. This is our seventh year in operation, and we have continued to work together to improve local services by delivering modern, high quality This year in the South East Territory, we handed over our biggest completed project, community infrastructure across the Territory. Phase 1 of the development of the Royal Edinburgh Hospital campus (P18) and broke ground on our highest value revenue funded project at the East Lothian With eight projects on site and more in development, we are sustaining a Community Hospital (P28) - the largest project to date in the Hub programme across good level of activity. -

Foi202000130010
The First Minister’s 2019 Christmas Card Project will benefit the following charities: Marine Conservation Society Glasgow & Clyde Rape Crisis Friends of Victoria & Whyteman’s Brae Hospitals Celebrated and named as one of the 100 Greatest Singers of All Time by Rolling Stone Magazine, Annie Lennox’s iconic musical career spans over four decades. Her collaboration with partner Dave Stewart formed Eurythmics in the early ‘80s. Lennox has also enjoyed a widely acclaimed solo career, selling over 83 million albums worldwide altogether. In 2012, Annie Lennox was awarded the Order of the British Empire for her work towards the eradication of AIDS and poverty in Africa. She is a Royal Academician, a respected social activist and philanthropist, and the first female Chancellor of Glasgow Caledonian University. Her work in the visual arts has included an exhibition at the Victoria and Albert Museum, London; ‘The House of Annie Lennox’ which travelled to Manchester, Aberdeen; and The National Portrait Gallery of Edinburgh. Her installation ‘Now I Let You Go’… is currently exhibited at Massachusetts Museum of Contemporary Art. Annie has been awarded the Royal Scottish Geographical Society’s ‘Livingstone Medal’ and, in 2017, her philanthropic work was honoured with the George Harrison Global Citizen Award, and a second prestigious German Sustainability Award. Merry Christmas and a Happy New Year Nollaig Chridheil agus Bliadhna Mhath Ùr Season’s Greetings Beannachdan aig àm na Nollaige The Rt Hon Nicola Sturgeon MSP and Mr Peter Murrell Bute ButeHouse, -

Description of Proposal Applicant Or Agent Details
West Lothian Civic Centre Howden South Road Howden Livingston EH54 6FF Tel: 01506 280000 (for general enquiries) Email: [email protected] Applications cannot be validated until all the necessary documentation has been submitted and the required fee has been paid. Thank you for completing this application form: ONLINE REFERENCE 100349510-001 The online reference is the unique reference for your online form only. The Planning Authority will allocate an Application Number when your form is validated. Please quote this reference if you need to contact the planning Authority about this application. Description of Proposal Please describe accurately the work proposed: * (Max 500 characters) Alter and Extend House to form single storey extension to rear of house Has the work already been started and/ or completed? * No Yes - Started Yes – Completed Applicant or Agent Details Are you an applicant or an agent? * (An agent is an architect, consultant or someone else acting on behalf of the applicant in connection with this application) Applicant Agent Page 1 of 5 Applicant Details Please enter Applicant details Mr Title: You must enter a Building Name or Number, or both: * Other Title: Building Name: Ben 1 First Name: * Building Number: Address 1 Robertson 1 Langside Crescent Last Name: * (Street): * Polbeth Company/Organisation Address 2: West Calder Telephone Number: * Town/City: * United Kingdom Extension Number: Country: * EH558UW Mobile Number: Postcode: * Fax Number: Email Address: * Site Address Details Planning Authority: West -

Lothian Health & Social Care Partnership Shadow Board- MA * Minutes of 6 November 2014 1.12
BOARD MEETING DATE: WEDNESDAY 4 FEBRUARY 2015 TIME: 9:30 A.M. - 12:00 P.M. VENUE: BOARDROOM, WAVERLEY GATE, 2-4 WATERLOO PLACE, EDINBURGH EH1 3EG Members are reminded that they should declare any financial and non-financial interests they have in the items of business for consideration, identifying the relevant agenda item and the nature of their interest. It is also a member’s duty under the Code of Conduct to ensure that any changes in circumstances are reported to the Corporate Services Manager within one month of them changing. AGENDA Agenda Lead Item Member Welcome to Members of the Public and the Press Apologies for Absence 1. Items for Approval 1.1. Minutes of the Board Meeting held on 3 December 2014 BH * 1.2. Minutes of the Special Board Meeting held on 14 January 2015 BH * 1.3. Running Action Note BH * 1.4. Performance Management AMcM * 1.5. Corporate Risk Register DF * 1.6. Committee Memberships BH * 1.7. Audit & Risk Committee - Minutes of 8 December 2014 JB * 1.8. Healthcare Governance Committee - Minutes of 25 November 2014 MB * 1.9. Finance & Resources Committee - Minutes of 12 November 2014 GW * 1.10. Strategic Planning Committee - Minutes of 13 November & 11 BH * December 2014 1.11. East Lothian Health & Social Care Partnership Shadow Board- MA * Minutes of 6 November 2014 1.12. Edinburgh Health & Social Care Partnership Shadow Board - RH * Minutes of 18 July 2014 1.13. Midlothian Health & Social Care Partnership Shadow Board Minutes PJ * of 23 October 2014 1.14. West Lothian Health & Care Partnership-Committee Sub - FT * Minutes of 18 December 2014 1.15. -

Lothian NHS Board Waverley Gate 2-4 Waterloo Place Edinburgh EH1 3EG
Lothian NHS Board Waverley Gate 2-4 Waterloo Place Edinburgh EH1 3EG Telephone: 0131 536 9000 www.nhslothian.scot.nhs.uk www.nhslothian.scot.nhs.uk Date: 13/05/2020 Your Ref: Our Ref: 4385 Enquiries to : Richard Mutch Extension: 35687 Direct Line: 0131 465 5687 [email protected] [email protected] Dear FREEDOM OF INFORMATION – GP SYSTEMS I write in response to your request for information in relation to GP Systems within Lothian. I have been provided with information to help answer your request by the eHealth Department of NHS Lothian. Question: I would like to make a request for a list of GP practices within your health board area and the clinical system they use. Answer: Practice Clinical System Tyne Medical Practice ,Haddington- CEN Vision North Berwick Group Practice -CEN Vision The Orchard Medical Practice ,Haddington- CEN Vision Lammermuir Medical Practice, Haddington -CEN Vision Gullane MP - CEN Vision Whitesands Medical Practice,Dunbar-CEN Vision Lauderdale Medical Practice,Dunbar -CEN Vision Cromwell Harbour Medical Practice,Dunbar -CEN Vision East Linton EMIS Tranent MP - CEN Vision Prestonpans -CEN Vision The Riverside Medical Practice -CEN Vision Harbours Medical Practice -CEN Vision Inveresk Medical Practice -CEN Vision Ormiston MP-CEN Vision Craigmillar - CEN Vision GP Systems - May 2020 Durham Road -CEN Vision Baronscourt -CEN Vision Annandale Medical Practice,Bellevue MC- CEN Vision Hopetoun , Bellevue MC -CEN Vision Summerside -CEN Vision Victoria -CEN Vision Mill Lane -CEN Vision Southfield -
![Scottish Record Society. [Publications]](https://docslib.b-cdn.net/cover/5606/scottish-record-society-publications-815606.webp)
Scottish Record Society. [Publications]
00 HANDBOUND AT THE L'.VU'ERSITY OF TORONTO PRESS (SCOTTISH RECORD SOCIETY, ^5^ THE Commissariot IRecorb of EMnbutGb. REGISTER OF TESTAMENTS. PART III. VOLUMES 81 TO iji—iyoi-iSoo. EDITED BY FRANCIS J. GRANT, W.S., ROTHESAY HERALD AND LYON CLEKK. EDINBURGH : PRINTED FOR THE SOCIETY BY JAMES SKINNER & COMPANY. 1899. EDINBURGH '. PRINTED BY JAMES SKINNER AND COMPANY. PREFATORY NOTE. This volume completes the Index to this Commissariot, so far as it is proposed by the Society to print the same. It includes all Testaments recorded before 31st December 1800. The remainder of the Record down to 31st December 1829 is in the General Register House, but from that date to the present day it will be found at the Commissary Office. The Register for the Eighteenth Century shows a considerable falling away in the number of Testaments recorded, due to some extent to the Local Registers being more taken advantage of On the other hand, a number of Testaments of Scotsmen dying in England, the Colonies, and abroad are to be found. The Register for the years following on the Union of the Parliaments is one of melancholy interest, containing as it does, to a certain extent, the death-roll of the ill-fated Darien Expedition. The ships of the Scottish Indian and African Company mentioned in " " " " the Record are the Caledonia," Rising Sun," Unicorn," Speedy " " " Return," Olive Branch," Duke of Hamilton (Walter Duncan, Skipper), " " " " Dolphin," St. Andrew," Hope," and Endeavour." ®Ij^ C0mmtssari0t ^ttoxi oi ®5tnburglj. REGISTER OF TESTAMENTS. THIRD SECTION—1701-180O. ••' Abdy, Sir Anthony Thomas, of Albyns, in Essex, Bart. -

East Lothian Shifting the Balance of Care
East Lothian Shifting the Balance of Care Commercial in Confidence Not disclosable under Freedom of Information (Scotland) Act Welcome Alison MacDonald Chief Officer East Lothian Health and Social Care Partnership Commercial in Confidence Not disclosable under Freedom of Information (Scotland) Act Healthcare Vision Support Needed for Healthcare • Dunbar • Musselburgh • North Berwick • Tranent Commercial in Confidence Not disclosable under Freedom of Information (Scotland) Act Community Hospital Commercial in Confidence Not disclosable under Freedom of Information (Scotland) Act Consultation East Lothian IJB Strategic Plan 2019 – 2022 The Community View Commercial in Confidence Not disclosable under Freedom of Information (Scotland) Act Andrew Milne Project Director NHS Lothian Commercial in Confidence Not disclosable under Freedom of Information (Scotland) Act Considerations The Strategic Plan Service and Community Needs Multi Agency Working Capital Investment Property Transactions Governance and Funding Commercial in Confidence Not disclosable under Freedom of Information (Scotland) Act The Business Case Strategic Assessment - Submitted Initial Agreement Outline Business Case Full Business Case Commercial in Confidence Not disclosable under Freedom of Information (Scotland) Act Governance Project Board Lothian Capital Investment Group Health and Social Care Partnership NHS Lothian Finances & Resources NHS Lothian Board Scottish Government Commercial in Confidence Not disclosable under Freedom of Information (Scotland) Act Approach Feasibility -

Search Sheet Details Search Sheet Midlothian 264764
21/05/2019 ScotLIS - Search Sheet Midlothian 264764 Search sheet details Number: 1 Description: (I.) ground, delineated red on plan, lying to south of ?q21?nWESTWOOD VIEW?z, WEST CALDER and (II.) 1/2 pro indiviso of common access area hatched green on plan, both part of subjects referred to in Disp. to John Kirk and another, recorded 26 Jan. 1993 From: From CSS 227972 Burdens: Disp. 9 Jul. 1964 Disp. 19 Apr. 1990 Disp. 26 Jan. 1993<BR><BR><BR><BR> Search sheet Midlothian 264764 Deed Date Notes reference 03 Dec. 2014 05563 (No. 66) DISP. by JOHN KIRK and MARGARET KIRK, spouses, formerly 95 Harburn Drive, West Calder now 21 Westwood View, aforesaid, - TO Trustee of said JOHN KIRK AND MARGARET KIRK, survivor and survivors, - of (I.) ground, delineated red on plan, lying to south of 21 WESTWOOD VIEW, WEST CALDER and (II.) 1/2 pro indiviso of common access area hatched green on plan, both part of subjects referred to in Disp. to John Kirk and another, recorded 26 Jan. 1993, containing real burdens and servitude rights affecting subjects herein disponed and subjects in said Disp. (under exception of subjects herein disponed). Dated 28 Nov. 2014. - C. G. & O. C. PLAN. (From CSS 227972) | 02944 (No.40) 24 Apr.2015 DEED OF SERVITUDE containing GRANT by ANDREW GRAHAM and ROBERT GRAHAM, both Gavieside Farm, West Calder , Proprietors of access road coloured blue on Plan, part of farms and lands of POLBETH, in Parish of West Calder, referred to in Disp. to Julia Neill Walker or Watt, recorded 9 Jul. -

Out in the Open Citation for Published Version: Moore, D 2012, out in the Open: Paraffin Harvester
Edinburgh Research Explorer Out In The Open Citation for published version: Moore, D 2012, Out In The Open: Paraffin Harvester. in Out in the Open: public Art in West Lothian. 1 edn, vol. 1, West Lothian Council Community Arts, Scotland, pp. Images pages pp. 11 and 48. Works cited pp. 18 and 43, Quotatation p. 33. Feature p. 49 and Acknowlegements p. 95. <http://lmmscache1.server.westlothian.gov.uk/media/downloaddoc/1799441/2195888/Out_in_the_Open_Pu blic_Art_book> Link: Link to publication record in Edinburgh Research Explorer Document Version: Publisher's PDF, also known as Version of record Published In: Out in the Open Publisher Rights Statement: © Moore, D. (2012). Out In The Open: Paraffin Harvester. In Out in the Open. West Lothian Council, Scotland. General rights Copyright for the publications made accessible via the Edinburgh Research Explorer is retained by the author(s) and / or other copyright owners and it is a condition of accessing these publications that users recognise and abide by the legal requirements associated with these rights. Take down policy The University of Edinburgh has made every reasonable effort to ensure that Edinburgh Research Explorer content complies with UK legislation. If you believe that the public display of this file breaches copyright please contact [email protected] providing details, and we will remove access to the work immediately and investigate your claim. Download date: 10. Oct. 2021 PUBLIC ART IN Firth of Forth M9 Harperrig VISITING PUBLIC ART IN WEST LOTHIAN Reservoir WEST LOTHIAN Rd 4 Each public art piece in this publication tells a story about the place in which it 3 A706 Grange A803 Blackness stands.