Internal Medicine Covid-19 Newsletter
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Real Womens Health
healthfeature All about YOUBy combining conventional medicine with alternative therapies, many women have discovered a better way to manage major life stages such as childbirth and menopause. By HEATHER MILLAR hen it comes to taking care, we author of Women’s Bodies, Women’s Wisdom intervention that western medicine can offer, women are renowned for putting (Bantam, 2006), it’s only when we make our we can achieve the best outcome for ourselves. Wourselves last. But according to health a priority that we can take responsibility “Our own body is the best health system Dr Christiane Northrup, a holistic physician for our bodies. By listening to our intuition, we have,” says Dr Northrup, “if we know how trained in obstetrics and gynaecology, and and combining that with the best advice and to listen to it.” ClubMag 77 feature FROM BIRTH TO LIFE It was intuition that led Lindy Schneider to make the choice to have a natural birth at home. “I had a deep sense of knowing that a home birth was right for me,” says Lindy, 37, from Warburton in Victoria. “I use natural therapies and am proactive about health-related issues, so this naturally carried into decisions regarding pregnancy and birth.” At first, her partner Tex wasn’t so sure – he was conscious of ensuring the safety of Lindy AGE: PHOTOLIBRARY AGE: WOMEN M and the baby should anything go wrong. So I early on, the couple looked at the family birth AND STDS centre of a major public hospital. However, Sexually transmitted diseases are an area for after they started birth classes and began to concern for both men and women. -

Dental White Paper
Institute for Science in Medicine WHITE PAPER THE ANTI-FLUORIDATIONIST THREAT TO PUBLIC HEALTH PREPARED BY JOHN E. DODES, DDS, FISM AND MICHAEL W. EASLEY, DDS, MPH, FISM APRIL 2012 Institute for Science in Medicine (ISM) is an international, educational and public-policy or- ganization comprised of health care professionals, scientists, and researchers who agree that the best science available should be used to determine health policy and to establish a standard of care that both protects and promotes the public health. We necessarily oppose policies which erode a science-based standard of care and thereby significantly expose the public to fraudulent, worthless, or harmful medical practices and products. Copyright 2012 by Institute for Science in Medicine. Permission to reproduce in its entirety is hereby granted, provided that it is not altered, not distributed for commercial purposes, and this notice is in- cluded. All other rights are reserved. White Paper: The Anti-Fluoridationist Threat to Public Health Declared by the Centers for Disease Control and Prevention to be one of the ten greatest public- health achievements of the Twentieth Century,1 community water fluoridation has been under attack by a small band of critics since its inception. The scientific consensus over fluoridation’s health benefits, safety, social justice, and economies has been firmly established over six decades of widespread use in the United States and elsewhere. Nevertheless, anti-science critics have never relented in their opposition — recycling previously disproven charges of harm, inventing new ones out of whole cloth, misrepresenting scientific facts and research, exaggerating risks, understating benefits, inappropriately invoking the precautionary principle, and accusing public health officials of corruption, conspiracy, and ‘mass medication’ of whole populations. -

Successful Pregnancy Following Diagnosis of Infertility and Miscarriage: a Chiropractic Case Report
CASE STUDY Successful Pregnancy Following Diagnosis of Infertility And Miscarriage: A Chiropractic Case Report Leslie Bedell, DC ABSTRACT for 30 days, and then one visit per week for an additional 30 Objective: This case describes the chiropractic care of a woman days. Other therapies used included: craniosacral therapy, re- with a history of infertility and miscarriage. laxation exercises, stretching and audio tapes. After 60 days of Clinical Features: A 27 year old female presented for care, a normal ovulatory cycle occurred, and she became preg- chiropactic care to improve her overall health, in the hope that nant after her second normal cycle. she may ultimately be able to have a child. In the previous year Conclusion: This case report of a woman with a history of in- she had suffered 2 miscarriages, and had been anovulatory for fertility and miscarriage contributes to the growing body of lit- 9 months. She was under medical treatment for infertility and erature on the response to chiropractic care among infertile ulcerative colitis, and followed a restrictive diet. Prior to at- women. The article discusses the impact of stress on a woman’s tempting to become pregnant, she had been on the birth control nervous system, and the possible associated changes in repro- pill for 7 years. ductive health. Further research is called for to evaluate the Chiropractic Care and Outcome: Examination protocols of safety, cost, and effectiveness of chiropractic care in women’s Torque Release Technique™ (TRT) were utilized to detect ver- health. tebral subluxations. Adjustments were applied with the Inte- Key words: chiropractic, Torque Release Technique (TRT), grator instrument; the initial visit schedule was twice weekly vertebral subluxation, infertility, miscarriage Introduction “Risk of infertility increased in females who reported ex- Currently, infertility is one of the greatest concerns of child posures to textile dyes, dry cleaning chemicals, noise, lead, -bearing women in the Western world. -

Download File
Page 1 “A lie can travel halfway around the world while the truth is putting on its shoes.” Mark Twain’s quote is more relevant than ever in times of online communication, where information or misinformation, bundled in bits and bytes, streams around the earth within seconds. SUMMARY This UNICEF working paper aims to track and analyse online anti-vaccination sentiment in social media networks by examining conversations across social media in English, Russian, Romanian and Polish. The findings support the assumption that parents actively use social networks and blogs to inform their decisions on vaccinating their children. The paper proposes a research model that detects and clusters commonly-used keywords and intensity of user interaction. The end goal is the development of targeted and efficient engagement strategies for health and communication experts in the field as well as for partner organisations. DISCLAIMER UNICEF working papers aim to facilitate greater exchange of knowledge and stimulate analytical discussion on an issue. This text has not been edited to official publications standards. Extracts from this paper may be freely reproduced with due acknowledgement. For the purposes of this research, no personal data has been extracted and stored for data collection and analysis. Page 2 CONTENT 1. Rationale 4 2. Introduction 5 2.1 Social Media: the conversation shift 5 2.2 Social Media: Fertile ground for anti- 5 vaccination sentiment 2.3 Social Media Monitoring 7 2.4 Influencers 8 3. Research Objectives 9 4. Methodology 11 4.1 Descriptive and Explorative Research Design 11 4.2 Data Collection 12 4.3 Limitations 13 4.4 Ethical Considerations 13 5. -

Possible Dangers of Mandated COVID-19 Vaccination: a Special Interview with Barbara Loe Fisher by Dr
Possible Dangers of Mandated COVID-19 Vaccination: A Special Interview With Barbara Loe Fisher By Dr. Joseph Mercola Dr. Mercola Welcome everyone, Dr. Mercola, helping you take control of your health and today we're joined with a veteran, the famous Barbara Loe Fisher, who is the co-founder of the National Vaccine Information Center (NVIC), which is one of the best organizations out there, certainly one of the oldest providing objective, non-biased information about vaccines to help people make an informed choice about whether or not they want to participate in the vaccine program. Welcome and thank you for joining us today because we've got loads of information to discuss since the last time we talked. Barbara Loe Fisher: That's so true. Dr. Mercola [Crosstalk 00:00:38]. Barbara Loe Fisher: In a way, it's a culmination what's happened this year of everything we have been talking about for the last decade. I know back in 1993, I started to predict that the day would come when Americans would not be able to participate in society without showing proof they've been vaccinated with whatever the government says they have to be vaccinated with, and I think we're most definitely heading that way right now. It's been unprecedented what's happened in this country, and really around the world since January. Dr. Mercola A very clever and sophisticated strategy to implement that goal, for sure, and most of us or many of us believe it was planned for certain. I think that is probably the main topic of discussion, and there's so many other things that we can go on and tangents to it, but it's this mandatory vaccination. -

Complaint for Permanent Injunction and Other Equitable Relief
Case: 1:16-cv-04282 Document #: 2 Filed: 04/13/16 Page 1 of 22 PageID #:2 UNITED STATES DISTRICT COURT NORTHERN DISTRICT OF ILLINOIS EASTERN DIVISION FEDERAL TRADE COMMISSION, Case No. 16 CV 4282 Plaintiff, v. COMPLAINT FOR MERCOLA.COM, LLC, a limited liability PERMANENT company, INJUNCTION AND OTHER EQUITABLE RELIEF MERCOLA.COM HEALTH RESOURCES, LLC, a limited liability company, and DR. JOSEPH MERCOLA, individually and as an owner, officer, and director of MERCOLA.COM, LLC, and MERCOLA.COM HEALTH RESOURCES, LLC, Defendants. Plaintiff, the Federal Trade Commission (“FTC”), for its Complaint alleges: 1. The FTC brings this action under Section 13(b) of the Federal Trade Commission Act (“FTC Act”), 15 U.S.C. § 53(b), to obtain a permanent injunction, rescission or reformation of contracts, restitution, the refund of monies paid, disgorgement of ill-gotten monies, and other equitable relief for Defendants’ acts or practices in violation of Sections 5(a) and 12 of the FTC Act, 15 U.S.C. § 45(a) and 52, in connection with the labeling, advertising, marketing, distribution, and sale of Mercola brand indoor tanning systems. 1 Case: 1:16-cv-04282 Document #: 2 Filed: 04/13/16 Page 2 of 22 PageID #:3 JURISDICTION AND VENUE 2. This Court has subject matter jurisdiction pursuant to 28 U.S.C. §§ 1331, 1337(a), and 1345, and 15 U.S.C. §§ 45(a) and 53(b). 3. Venue is proper in this district under 28 U.S.C. § 1391(b)(1), (b)(2), (b)(3), (c)(1), (c)(2), and (d), and 15 U.S.C. -
SAYER JI! 3 EXPERT TALK TRANSCRIPTS from HEALTHMEANS CONTENTS
LET’S “TALK” WITH SAYER JI! 3 EXPERT TALK TRANSCRIPTS from HEALTHMEANS CONTENTS Enjoy learning from these expert Transcending the Detox/ We’re happy that you’re taking talk transcripts pulled Retox Cycle through time to learn about living a from the thousands of talks Radical Nourishment healthier and happier life, and we in our HealthMeans library! Deanna Minich, PhD, CNS, IFMCP hope you’ll make us a regular part with Sayer Ji of that journey! If you’re already a member of Click here to watch this interview! HealthMeans, you can access From the entire HealthMeans the video interviews of these Evidence-Based Medicine team, thank you for downloading talks below: Proves the Power of the these transcripts—we hope you If you’re not yet a member, Mind and Soul learn a lot from them! Alicia Lynn Diaz, MA, AHP be sure to sign up to access with Sayer Ji these interviews! Click here to watch this interview! Food as Medicine Carrie Diulus, MD and Mark Hyman, MD with Sayer Ji Click here to watch this interview! Transcending the Detox/ Retox Cycle through Radical Nourishment Deanna Minich, PhD, CNS, IFMCP with Sayer Ji Click here to watch this interview! The purpose of this presentation is to convey information. It is not intended to diagnose, treat, or cure your condition or to be a substitute for advice from your physician or other healthcare professional. Dr. Minich: Hello, everyone! This different things. You mentioned to Dr. Minich: So GreenMedInfo came is Deanna Minich, host of The me that your father’s a toxicologist. -
Vaccinereport En
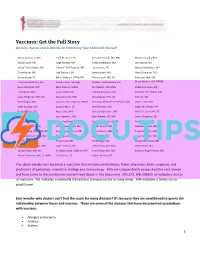
Vaccines: Get the Full Story Doctors, Nurses and Scientists on Protecting Your Child and Yourself Nicola Antonucci, MD Todd M. Elsner, DC Alexander Kotok, MD, PhD Máximo Sandín, PhD David Ayoub, MD Jorge Esteves, MD Eneko Landaburu, MD Len Saputo, MD Nancy Turner Banks, MD Edward "Ted" Fogarty, MD Luc Lemaire, DC Michael Schachter, MD Timur Baruti, MD Jack Forbush, DO Janet Levatin, MD Viera Scheibner, PhD Danny Beard, DC Milani Gabriele, CRNA, RN Thomas Levy, MD, JD Penelope Shar, MD Françoise Berthoud, MD Sheila Gibson, MD, BSc Stephen L'Hommedieu, DC Bruce Shelton, MD, MD(H) Russell Blaylock, MD Mike Godfrey, MBBS Paul Maher, MD, MPH Debbi Silverman, MD Fred Bloem, MD Isaac Golden, ND Andrew Maniotis, PhD Kenneth “KP” Stoller, MD Laura Bridgman, FNP, ND Gary Goldman, PhD Steve Marini, PhD, DC Terri Su, MD Kelly Brogan, MD Garry Gordon, MD, DO, MD(H) Juan Manuel Martínez Méndez, MD Didier Tarte, MD Sarah Buckley, MD Doug Graham, DC Sue McIntosh, MD Leigh Ann Tatnall, RN Rashid Buttar, DO Boyd Haley, PhD Richard Moskowitz, MD Adiel Tel‐Oren, MD, DC Harold Buttram, MD Gayl Hamilton, MD Sheri Nakken, RN, MA Sherri Tenpenny, DO Lisa Cantrell, RN Linda Hegstrand, MD, PhD Christiane Northrup, MD Renee Tocco, DC Lua Català Ferrer, MD James Howenstine, MD Amber Passini, MD Demetra Vagias, MD, ND Jennifer Craig, PhD, BSN, MA Suzanne Humphries, MD Ronald Peters, MD, MPH Franco Verzella, MD Robert Davidson, MD, PhD Belén Igual Diaz, MD Jean Pilette, MD Julian Whitaker, MD Ana de Leo, MD Philip Incao, MD Pat Rattigan, ND Ronald Whitmont, MD Carlos de Quero Kops, MD Joyce Johnson, ND Zoltan Rona, MD, MSc Betty Wood, MD Carolyn Dean, MD, ND A. -

The Truth About COVID-19 Exposing the Great Reset, Lockdowns, Vaccine Passports, and the New Normal Dr
Also by Dr. Joseph Mercola EMF*D: 5G, Wi-Fi and Cell Phones: Hidden Harms and How to Protect Yourself (2020) KetoFast: Rejuvenate Your Health With a Step-by-Step Guide to Timing Your Ketogenic Meals (2019) Fat for Fuel: A Revolutionary Diet to Combat Cancer, Boost Brain Power, and Increase Your Energy (2017) Effortless Healing: 9 Simple Ways to Sidestep Illness, Shed Excess Weight, and Help Your Body Fix Itself (2015) The Great Bird Flu Hoax: The Truth They Don’t Want You to Know About the ‘Next Big Pandemic’ (2006, with Pam Killeen) The No-Grain Diet: Conquer Carbohydrate Addiction and Stay Slim for Life (2003, with Alison Rose Levy) Dark Deception: Discover the Truth About the Benefits of Sunlight Exposure (2008, with Jeffry Herman) Generation XL: Raising Healthy, Intelligent Kids in a High-Tech, Junk-Food World (2007, with Ben Lerner) Healthy Recipes for Your Nutritional Type (2007, with Kendra Degen Pearsall) Take Control of Your Health (2007, with Kendra Degen Pearsall) Sweet Deception: Why Splenda®, NutraSweet®, and the FDA May Be Hazardous to Your Health (2006, with Kendra Degen Pearsall) Also by Ronnie Cummins Grassroots Rising: A Call to Action on Climate, Farming, Food, and a Green New Deal Genetically Engineered Food a Self-Defense Guide for Consumers (2000, with Ben Lilliston) Children of the World (1990, a five-book series) The Truth About COVID-19 Exposing The Great Reset, Lockdowns, Vaccine Passports, and the New Normal Dr. Joseph Mercola Ronnie Cummins Foreword by Robert F. Kennedy Jr. Chelsea Green Publishing White River Junction, Vermont London, UK Copyright © 2021 by Florida Health Publishing, LLC. -

International Journal of Human Nutrition and Functional Medicine
International Journal of Human Nutrition and Functional Medicine International Journal of Human Nutrition and Functional Medicine ® www.IntJHumNutrFunctMed.org (ISSN 2378-4881) is published and © copyrighted by the International College of Human Nutrition and Functional Medicine ® www.ICHNFM.ORG North America • Latinoamerica • Europe International Journal of Human Nutrition and Functional Medicine (ISSN 2378-4881) www.ICHNFM.org Photo of town center and Roman aqueduct in Segovia Spain © 2016 by Dr Vasquez Expert Perspectives • Clinical Nutrition • Research Methodology • Publication Analysis How to Understand, Refute, and Plan Studies Using Vitamin D Alex Vasquez DO ND DC FACN Defining the problems field into which they enter; one can be amused by the 1. The (primary) problem: Most doctors and researchers prospect of a researcher placed in a position of have zero expert-level training in Nutrition (let alone authority to shape and define the direction of a field Clinical Nutrition, Therapeutic/Interventional which he/she has never studied, ie, many researchers Nutrition, Functional Nutrition) and therefore the quite obviously wear no clothes. studies they design using vitamin D are methodologically flawed, as described below. Guidelines for vitamin D clinical trials were broadly 2. The (secondary) problem: Too many studies using published in 2004 and 2005 vitamin D (cholecalciferol) have used vitamin D in 1) In 2004 and 2005, I was the principal author on several doses that are inadequate, 2) for durations that are publications published in peer-reviewed journals, and in inadequate, and thus these studies are therapeutically each of these I listed criteria for the design and therefore underpowered, tending to lead to lackluster or evaluation of studies using vitamin D; I will list these negative (inefficacious) results, thereby leading to the publications here with hyperlinks to their full text and false conclusion that vitamin D is ineffective when in then describe these criteria with any updates. -

Health Hunter Continued from Page 2 Associates at the Harvard Medical School and Brigham and Women's Steps to Healing Hospital Showed a Relationship Be 1
More support for antioxidants in Medical ignorance heart disease prevention The greatest single achievement of Richard Lewis science in this most scientifically productive of centuries is the wo articles in recent issues of from heart disease the help they discovery that we are profoundly T deserve-a proved, successful The Journal of the American ignorant; we know very little about MedicalAssociation (JAMA) gave a treatment." The information about nature and understand even less . .. big boost to the use of antioxidant vitamin E wasn't accepted by the I wish there were someformal course nutrients for controlling and pre mainstream physicians. in medical school on Medical venting coronary heart disease But times are changing and Ignorance; textbooks as well, (CHD). nutrition is finding its way into the although they would have to be very standard medical journals and even hgavy volumes. The antioxidani theory into the clinical offices of standard Lewis Thomas, President Emeritus, holds that antioxidant physicians. Sloan-Kettering, physiCian, nutrients protect the low In one such article appearing in philosopher, author density lipoproteins the July 12 issue of JAMA, the researchers concluded by writing, (WL) from oxidation. Ann Kerwin, Ph.D. and Marlys "It appears that reductions in serum Witte, M.D. are doing just what Dr. The antioxidant nutrients are total cholesterol levels are not likely Thomas wanted-teaching a course vitamins A, C, E, and beta carotene to bring cultures with a high CHD in medical ignorance at the Uni and the trace mineral selenium, along risk, such as the United States and versity of Arizona College of with magnesium and zinc. -

CORPORATE OFFICE Level 1 32 Oxford Terrace Telephone: 0064 3 364 4160 Christchurch Central Fax: 0064 3 364 4165 CHRISTCHURCH 8011 [email protected]
CORPORATE OFFICE Level 1 32 Oxford Terrace Telephone: 0064 3 364 4160 Christchurch Central Fax: 0064 3 364 4165 CHRISTCHURCH 8011 [email protected] 15 June 2021 9(2)(a) RE Official Information Act request CDHB 10600 I refer to your email dated 6 May 2021 requesting the following information under the Official Information Act from Canterbury DHB regarding vaccine misinformation. Specifically: • Since February 1 2021, copies of any reports, documents, memoranda, and correspondence, both internal and external, regarding misinformation about Covid-19 vaccines/vaccination, including any reports of examples of misinformation, any official reaction to such examples or the problem of misinformation as a whole, and the possible impact of such misinformation. Please refer to Appendix 1 (attached) for correspondence (both internal and external) regarding misinformation about Covid-19 vaccines/vaccination. Note: we have redacted information under the following sections of the Official Information Act. Section 9(2)(a) – “….to protect the privacy of natural persons, including those deceased”. Section 9(2)(b)(ii) “…to protect the commercial position of the person who supplied the information, or who is the subject of the information”. Section 9(2)(g)(i) “… to maintain the effective conduct of public affairs through the free and frank expression of opinions.” We have also removed information we believe to be ‘Out of scope’ of your request. I trust this satisfies your interest in this matter. You may, under section 28(3) of the Official Information Act, seek a review of our decision to withhold information by the Ombudsman. Information about how to make a complaint is available at www.ombudsman.parliament.nz; or Freephone 0800 802 602.