Cellular and Humoral Immune Alterations in Thymectomized Patients for Thymoma
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Pseudoischemic Electrocardiogram in Myasthenia Gravis with Thymoma Published Online in Wiley Interscience
Address for correspondence: Nicola Mumoli, MD CaseShort Communication Livorno Hospital Department of Internal Medicine Viale Alfieri 36 Pseudoischemic Electrocardiogram in 57100 Livorno, Italy Myasthenia Gravis with Thymoma: [email protected] Reversibility After Thymectomy Patrizio Chiavistelli, MD, Marco Cei, MD, Giovanni Carmignani, MD, Carlo Bartolomei, MD Nicola Mumoli, MD Department of Internal Medicine, Livorno Hospital, Livorno, Italy Abnormal ST T-wave changes can be found at presentation in various noncoronary disorders; misinterpretation of these patterns as ischemic heart disease can lead to erroneous diagnosis and treatment. Here we present a case of myasthenia gravis (MG) with thymoma, in which the resting electrocardiogram (ECG) led to a misleading diagnosis of myocardial ischemia. After thymectomy, the ECG resumed a normal pattern. Myasthenia gravis is not usually considered in the differential diagnosis of conditions associated with an abnormal ECG. The combination of dysphagia, dyspnoea, ECG changes, and creatine kinase (CK) elevations may easily bring to mind an erroneous and possibly deleterious diagnosis of myocardial ischemia. Introduction did not seek medical attention. At the beginning of the The resting 12-lead electrocardiogram (ECG) remains at current year, he reported a flu-like illness, with spontaneous the center of the diagnostic pathways of acute coronary recovery, but shortly afterward he experienced dyspnea, syndromes (ACSs), either with1 or without ST segment dysphagia, and weight loss (37 kg). One month before elevation,2 because it serves as an invaluable tool for admission, he underwent fiberoptic endoscopy of the nose, both diagnosis and risk stratification. Nevertheless, as is pharynx, and larynx because of dysphonia, without any universally accepted, the predictive value of any diagnostic evidence of an active disease. -

Studies of Thymic Function with Emphasis on the Role of the Thymus in Oncogenesist
[CANCER RESEARCH 26 Part I, 551-574, April 1966] Studies of Thymic Function with Emphasis on the Role of the Thymus in Oncogenesist LLOYDW. LAW National Cancer Institute, Bethesda, Maryland This presentation will be concerned with 2 general topics: organ to other sites occurs with a selective seeding in spleen (a) our present knowledge of thymic structure and function, lymph nodes, and other lymphoid organs. but particularly the latter, as revealed by the results of recent For a more detailed discussion of the ontogeny of the thymus experiments in several species of animals following early thymic and its microscopic anatomy, the reader is referred to the studies ablation, and (b) consideration of the precise role of the thymus in of Smith (97) and of Ruth et al. (92). the initiation and suppression of neoplastic growths. Pertaining to Thymic Structure and Function Origin and Early Structure of the Thymus In most species the thymus is located in the upper anterior The thymus is a compound organ consisting of 3 quite different part of the chest. Exceptions are the chicken and guinea pig. cell systems: (a) lymphoid cells, (b) reticulum cells, and (c) The absolute size varies from species to species but the absolute e[)ithehal cells. The latter 2 may be referred to as the epithelial size of thymic lobules appears to be remarkably uniform in the reticulum cell complex. The thymus in mammals arises as various species, suggesting that there may be a critical limit for paired structures from the endoderm of the 3rd and 4th branchial the size of a thymic lobule. -

Analysis of the Role of Thyroidectomy and Thymectomy in the Surgical Treatment of Secondary Hyperparathyroidism
Am J Otolaryngol 40 (2019) 67–69 Contents lists available at ScienceDirect Am J Otolaryngol journal homepage: www.elsevier.com/locate/amjoto Analysis of the role of thyroidectomy and thymectomy in the surgical ☆ treatment of secondary hyperparathyroidism T Mateus R. Soares, Graziela V. Cavalcanti, Ricardo Iwakura, Leandro J. Lucca, Elen A. Romão, ⁎ Luiz C. Conti de Freitas Division of Head and Neck Surgery, Department of Ophthalmology, Otolaryngology, Head and Neck Surgery, Ribeirao Preto Medical School, University of Sao Paulo, Brazil ARTICLE INFO ABSTRACT Keywords: Purpose: Parathyroidectomy can be subtotal or total with an autograft for the treatment of renal hyperpar- Parathyroidectomy athyroidism. In both cases, it may be extended with bilateral thymectomy and total or partial thyroidectomy. Hyperparathyroidism Thymectomy may be recommended in combination with parathyroidectomy in order to prevent mediastinal Thymectomy recurrence. Also, the occurrence of thyroid disease observed in patients with hyperparathyroidism is poorly Thyroidectomy understood and the incidence of cancer is controversial. The aim of the present study was to report the ex- perience of a single center in the surgical treatment of renal hyperparathyroidism and to analyse the role of thyroid and thymus surgery in association with parathyroidectomy. Materials and methods: We analysed parathyroid surgery data, considering patient demographics, such as age and gender, and surgical procedure data, such as type of hyperparathyroidism, associated thyroid or thymus surgery, surgical duration and mediastinal recurrence. Histopathological results of thyroid and thymus samples were also analysed. Results: Medical records of 109 patients who underwent parathyroidectomy for secondary hyperparathyroidism were reviewed. On average, thymectomy did not have impact on time of parathyroidectomy (p = 0.62) even when thyroidectomy was included (p = 0.91). -
Psi Technical Specs V31.Pdf
AHRQ Quality Indicators Patient Safety Indicators: Technical Specifications Department of Health and Human Services Agency for Healthcare Research and Quality http://www.qualityindicators.ahrq.gov March 2003 Version 3.1 (March 12, 2007) AHRQ Quality Indicators Web Site: http://www.qualityindicators.ahrq.gov Table of Contents About the Patient Safety Indicators ............................................................................................................... 1 Patient Safety Indicators – Detailed Definitions ............................................................................................ 3 Complications of Anesthesia (PSI 1) ............................................................................................................ 3 Death in Low-Mortality DRGs (PSI 2) ........................................................................................................... 5 Decubitus Ulcer (PSI 3) ................................................................................................................................. 7 Failure to Rescue (PSI 4) .............................................................................................................................. 9 Foreign Body Left during Procedure, Secondary Diagnosis Field (PSI 5 and 21)...................................... 17 Iatrogenic Pneumothorax, Secondary Diagnosis Field (PSI 6 and 22)....................................................... 18 Selected Infections Due to Medical Care, Secondary Diagnosis Field (PSI 7 and 23) ............................. -

Icd-9-Cm (2010)
ICD-9-CM (2010) PROCEDURE CODE LONG DESCRIPTION SHORT DESCRIPTION 0001 Therapeutic ultrasound of vessels of head and neck Ther ult head & neck ves 0002 Therapeutic ultrasound of heart Ther ultrasound of heart 0003 Therapeutic ultrasound of peripheral vascular vessels Ther ult peripheral ves 0009 Other therapeutic ultrasound Other therapeutic ultsnd 0010 Implantation of chemotherapeutic agent Implant chemothera agent 0011 Infusion of drotrecogin alfa (activated) Infus drotrecogin alfa 0012 Administration of inhaled nitric oxide Adm inhal nitric oxide 0013 Injection or infusion of nesiritide Inject/infus nesiritide 0014 Injection or infusion of oxazolidinone class of antibiotics Injection oxazolidinone 0015 High-dose infusion interleukin-2 [IL-2] High-dose infusion IL-2 0016 Pressurized treatment of venous bypass graft [conduit] with pharmaceutical substance Pressurized treat graft 0017 Infusion of vasopressor agent Infusion of vasopressor 0018 Infusion of immunosuppressive antibody therapy Infus immunosup antibody 0019 Disruption of blood brain barrier via infusion [BBBD] BBBD via infusion 0021 Intravascular imaging of extracranial cerebral vessels IVUS extracran cereb ves 0022 Intravascular imaging of intrathoracic vessels IVUS intrathoracic ves 0023 Intravascular imaging of peripheral vessels IVUS peripheral vessels 0024 Intravascular imaging of coronary vessels IVUS coronary vessels 0025 Intravascular imaging of renal vessels IVUS renal vessels 0028 Intravascular imaging, other specified vessel(s) Intravascul imaging NEC 0029 Intravascular -

Unthsc Unthsc
Institutional Animal Care and Use Committee Title: Analgesics and Anesthesia in Laboratory Animals at UNTHSC UNTHSC Document #: 035 Version #: 02 Approved by IACUC Date: August 22, 2017 A. BACKGROUND INFORMATION a. In general, procedures which cause pain in humans should be expected to cause pain in animals. b. Appropriate analgesics must be used unless withholding such agents is scientifically justified in the animal use protocol. B. RESPONSIBILITIES a. It is the responsibility of the Principal Investigator (PI): i. To list appropriate analgesics when performing potentially painful procedures on animals. The PI must consult with the Attending Veterinarian for information on which analgesic(s) to use if the PI is unsure. ii. To procure the analgesics listed on an approved protocol unless arrangements are made with DLAM (Department of Laboratory Animal Medicine) ahead of time. Some analgesics are controlled substances and will require a DEA license. It is the responsibility of the PI to have this license. b. It is the responsibility of the Principal Investigator and other research personnel who will administer analgesics to have completed the applicable CITI training module. c. It is the responsibility of the Principal Investigator or designated lab staff and/or students to administer the analgesics listed in the approved protocol unless arrangements are made ahead of time for DLAM staff to do so. d. It is the responsibility of IACUC to assure that this SOP is followed. C. PROCEDURES a. Determining which procedures require analgesia and which ones may be useful, several factors should be considered: i. The invasiveness of the procedure that was performed: 1. -

The American Association of Endocrine Surgeons Guidelines for Definitive Management of Primary Hyperparathyroidism
Supplementary Online Content Wilhelm SM, Wang TS, Ruan DT, et al. The American Association of Endocrine Surgeons guidelines for definitive management of primary hyperparathyroidism. JAMA Surg. Published online August 10, 2016. doi:10.1001/jamasurg.2016.2310. eAppendix. The American Association of Endocrine Surgeons (AAES) Guidelines for Definitive Management of Primary Hyperparathyroidism eTable 1. Table of Contents: The American Association of Endocrine Surgeons (AAES) Guidelines for Definitive Management of Primary Hyperparathyroidism eTable 2. Common Secondary Causes of Elevated PTH Levels eTable 3. Selected Results of the Two Most Commonly Utilized IPM Protocols eTable 4. Parathyroid Carcinoma in Large Retrospective Series This supplementary material has been provided by the authors to give readers additional information about their work. © 2016 American Medical Association. All rights reserved. 1 Downloaded From: https://jamanetwork.com/ on 09/28/2021 eAppendix. The American Association of Endocrine Surgeons (AAES) Guidelines for Definitive Management of Primary Hyperparathyroidism ABSTRACT Importance Primary hyperparathyroidism (pHPT) is a common clinical problem for which the only definitive management is surgery. Surgical management has evolved considerably during the last several decades. Objective To develop evidence-based guidelines to enhance the appropriate, safe, and effective practice of parathyroidectomy. Evidence Review A multidisciplinary panel used PubMed to reviewed the medical literature from January 1, 1985, to July 1, 2015. Levels of evidence were determined using the American College of Physicians grading system, and recommendations were discussed until consensus. Findings Initial evaluation should include 25-hydroxyvitamin D measurement, 24-hour urine calcium measurement, dual-energy x-ray absorptiometry, and supplementation for vitamin D deficiency. Parathyroidectomy is indicated for all symptomatic patients, should be considered for most asymptomatic patients, and is more cost-effective than observation or pharmacologic therapy. -

Transcervical Thymectomy
Original Article Page 1 of 5 Transcervical thymectomy Marcin Zieliński1, Mariusz Rybak1*, Katarzyna Solarczyk-Bombik1, Michal Wilkojc1, Wojciech Czajkowski1, Sylweriusz Kosinski2, Edward Fryzlewicz2, Tomasz Nabialek2, Malgorzata Szolkowska3, Juliusz Pankowski4 1Department of the Thoracic Surgery, 2Department the Anesthesiology and Intensive Care, Pulmonary Hospital, Zakopane, Poland; 3Department of Pathology of the Tuberculosis Institute, Warsaw, Poland; 4Department of Pathology, Pulmonary Hospital, Zakopane, Poland Contributions: (I) Conception and design: M Zieliński; (II) Administrative support: None; (III) Provision of study materials or patients: None; (IV) Collection and assembly of data: All authors; (V) Data analysis and interpretation: None; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Marcin Zieliński, MD, PhD. Department of Thoracic Surgery, Pulmonary Hospital, Ul. Gładkie 1, 34 500 Zakopane, Poland. Email: [email protected]. Background: The aim of this article is to describe the technique of minimally invasive extended thymectomy performed through the transcervical video-thoracoscopic (VATS) approach with elevation of the sternum for the thymic tumors with/without myasthenia gravis (MG). Methods: The operation is done through the collar incision in the neck of a length of 4–8 cm. To facilitate an access to the mediastinum a one-tooth hook connected to the Zakopane bar (Aesculap-Chifa, Nowy Tomysl, Poland) is inserted under the sternal notch for elevation of the sternum. Careful anatomical dissection of the structures of the lower neck region is done with preservation from injury of the thyroid gland, the parathyroid glands and both laryngeal recurrent nerves. The thymus gland is resected en-bloc with the surrounding fatty tissue of the lower neck and the anterior superior mediastinum. -
Transmittal 1269 Date: JUNE 15, 2007 Change Request 5643
Department of Health & CMS Manual System Human Services (DHHS) Pub 100-04 Medicare Claims Processing Centers for Medicare & Medicaid Services (CMS) Transmittal 1269 Date: JUNE 15, 2007 Change Request 5643 SUBJECT: Medicare Contractor Annual Update of the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) I. SUMMARY OF CHANGES: This instruction is CMS’ annual reminder to the Medicare contractors of the ICD-9-CM update that is effective for the dates of service on and after October 1, 2007. NEW / REVISED MATERIAL EFFECTIVE DATE: October 1, 2007 IMPLEMENTATION DATE: October 1, 2007 Disclaimer for manual changes only: The revision date and transmittal number apply only to red italicized material. Any other material was previously published and remains unchanged. However, if this revision contains a table of contents, you will receive the new/revised information only, and not the entire table of contents. II. CHANGES IN MANUAL INSTRUCTIONS: (N/A if manual is not updated) R=REVISED, N=NEW, D=DELETED-Only One Per Row. R/N/D Chapter / Section / Subsection / Title N/A III. FUNDING: No additional funding will be provided by CMS; Contractor activities are to be carried out within their FY 2007 operating budgets. IV. ATTACHMENTS: Recurring Update Notification *Unless otherwise specified, the effective date is the date of service. Attachment – Recurring Update Notification Pub. 100-04 Transmittal: 1269 Date: June 15, 2007 Change Request: 5643 SUBJECT: Medicare Contractor Annual Update of the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) Effective Date: October 1, 2007 Implementation Date: October 1, 2007 I. -

Robotic Thoracic Surgery
AME Surgery Series 6A005 Robotic Thoracic Surgery: 6A005 A Collection of Clinical Pearls A Collection of Clinical Pearls Surgery: Thoracic Robotic Honorary Editors: Andrea Imperatori James D. Luketich Santiago Horgan Editors: Qingquan Luo Brian E. Louie Giuseppe Marulli Associate Editors: Calvin S.H. Ng Benjamin Wei Joel Dunning www.amegroups.com Editors: Qingquan Luo Qingquan Editors: Giuseppe Marulli Giuseppe E. Louie Brian AME Surgery Series 6A005 Robotic Thoracic Surgery: A Collection of Clinical Pearls Honorary Editor: Andrea Imperatori James D. Luketich Santiago Horgan Editors: Qingquan Luo Brian E. Louie Giuseppe Marulli Associate Editors: Calvin S.H. Ng Benjamin Wei Joel Dunning AME Publishing Company Room C 16F, Kings Wing Plaza 1, NO. 3 on Kwan Street, Shatin, NT, Hong Kong Information on this title: www.amegroups.com For more information, contact [email protected] Copyright © AME Publishing Company. All rights reserved. This publication is in copyright. Subject to statutory exception and to the provisions of relevant collective licensing agreements, no reproduction of any part may take place without the written permission of AME Publishing Company. First published in 2018 Printed in China by AME Publishing Company Editors: Qingquan Luo, Brian E. Louie, Giuseppe Marulli Cover Image lllustrator: Anthony P. Yim, HongKong, China Robotic Thoracic Surgery: A Collection of Clinical Pearls (Hard Cover) ISBN: 978-988-78920-3-8 AME Publishing Company, Hong Kong AME Publishing Company has no responsibility for the persistence or accuracy of URLs for external or third-party internet websites referred to in this publication, and does not guarantee that any content on such websites is, or will remain, accurate or appropriate. -

Multimodal Treatment of Sporadic and Inherited Neuroendocrine Tumors of the Thymus
Multimodal treatment of sporadic and inherited neuroendocrine tumors of the thymus Nils Habbe, MD, Jens Waldmann, MD, Detlef K. Bartsch, MD, Volker Fendrich, MD, Matthias Rothmund, MD, and Peter Langer, MD, Marburg, Germany Background. Neuroendocrine tumors of the thymus (NETT) are a rare tumor entity of the anterior mediastinum. They belong to the category of foregut carcinoids and are often associated with the multiple endocrine neoplasia type 1 (MEN1) syndrome. Approximately 180 cases have been reported since their first description. NETT reveal an aggressive behavior leading to rapid local invasion and metastatic spread. An aggressive surgical approach may achieve long-term survival. Methods. Patients presenting from 1990 to 2005 at the Department of Surgery and the Department of Gastroenterology of the Philipps-University Marburg with neuroendocrine tumors were enrolled in a prospective database with a follow-up until 2005. Fifty MEN1-patients were enrolled in a study and screening program. These databases were retrospectively reviewed identifying all patients with NETT. The clinical features, therapeutical approaches and the outcome were analyzed. Results. Six patients were found with NETT, 4 patients suffered from metastases at the time of presentation. All patients were male, with a median age of 41.3 years at presentation. Four out of these 6 patients revealed MEN1 syndrome. All patients underwent tumor resection via sternotomy. Three patients underwent parathyreoidectomy and transcervical thymectomy before the NETT was diagnosed. Median survival was 53 months (range, 24--109). Conclusion. Given a frequent association between MEN1 and NETT, all patients with NETT should be screened for MEN1. Since transcervical thymectomy does not prevent all MEN1 patients from developing NETT, existing surveillance guidelines for MEN1 should consider CT scan of the thorax on a regular basis. -
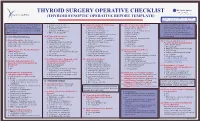
Thyroid Surgery Operative Checklist
THYROID SURGERY OPERATIVE CHECKLIST (THYROID SYNOPTIC OPERATIVE REPORT TEMPLATE) Electronic version available on the BC SON website: http://www.bccancer.bc.ca/HPI/SON/ For a case that requires concurrent thyroid c. Benign- Goiter or Cyst 10. Adjunctive Surgical Techniques/ 14. Site of Gross Residual Cancer f. Visualized abnormal/enlarged and parathyroid surgery, please answer d. Benign- Graves Disease or Technology Utilized Present After Operation (indicate if biopsied/confirmed by questions 1 – 23 (below) and then complete Hyperthyroidism (Select all that apply) (Select all that apply) frozen section) and partially removed the Parathyroid Surgery Operative Checklist e. Inadequate FNA Biopsy(s) a. Monopolar electrocautery a. Right recurrent laryngeal nerve g. Visualized abnormal/enlarged (back of card). f. Other (please specify) b. Bipolar electrocautery b. Right esophagus (indicate if biopsied/confirmed by c. Electrothermal vessel sealing device c. Right trachea frozen section) and autotransplanted TM A. PREOPERATIVE DETAILS 6. If Thyroid Reoperation (Ligasure or equivalent) d. Right larynx h. Not identified (Select All That Apply) d. Ultrasonic vessel sealing device e. Left recurrent laryngeal nerve 1. Clinical Preamble - Dictate as a. Not applicable (Harmonic ScalpelTM or equivalent) f. Left esophagus 20. Destination and Marking of appropriate. May include details such as b. Completion thyroid lobectomy e. Recurrent laryngeal nerve g. Left trachea Parathyroid Autotransplantation patient marking, antibiotics, DVT, c. Removal central neck cancer monitoring h. Left larynx (Select all that apply) prophylaxis, etc. recurrence or persistence f. Loupes (magnifying glasses) i. Other (please specify) a. Not applicable d. Removal lateral neck cancer g. Robotics b. Right sternocleidomastoid muscle 2. Preoperative Fine Needle Aspiration recurrence or persistence h.