Dictionary of Rheumatology
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Births, Marriages, and Deaths
DEC. 31, 1955 MEDICAL NEWS MEDICALBRrsIJOURNAL. 1631 Lead Glazes.-For some years now the pottery industry British Journal of Ophthalmology.-The new issue (Vol. 19, has been forbidden to use any but leadless or "low- No. 12) is now available. The contents include: solubility" glazes, because of the risk of lead poisoning. EXPERIENCE IN CLINIcAL EXAMINATION OP CORNEAL SENsITiVrry. CORNEAL SENSITIVITY AND THE NASO-LACRIMAL REFLEX AFTER RETROBULBAR However, in some teaching establishments raw lead glazes or ANAES rHESIA. Jorn Boberg-Ans. glazes containing a high percentage of soluble lead are still UVEITIS. A CLINICAL AND STATISTICAL SURVEY. George Bennett. INVESTIGATION OF THE CARBONIC ANHYDRASE CONTENT OF THE CORNEA OF used. The Ministry of Education has now issued a memo- THE RABBIT. J. Gloster. randum to local education authorities and school governors HYALURONIDASE IN OCULAR TISSUES. I. SENSITIVE BIOLOGICAL ASSAY FOR SMALL CONCENTRATIONS OF HYALURONIDASE. CT. Mayer. (No. 517, dated November 9, 1955) with the object of INCLUSION BODIES IN TRACHOMA. A. J. Dark. restricting the use of raw lead glazes in such schools. The TETRACYCLINE IN TRACHOMA. L. P. Agarwal and S. R. K. Malik. APPL IANCES: SIMPLE PUPILLOMETER. A. Arnaud Reid. memorandum also includes a list of precautions to be ob- LARGE CONCAVE MIRROR FOR INDIRECT OPHTHALMOSCOPY. H. Neame. served when handling potentially dangerous glazes. Issued monthly; annual subscription £4 4s.; single copy Awards for Research on Ageing.-Candidates wishing to 8s. 6d.; obtainable from the Publishing Manager, B.M.A. House, enter for the 1955-6 Ciba Foundation Awards for research Tavistock Square, London, W.C.1. -

Severe Septicaemia in a Patient with Polychondritis and Sweet's
81 LETTERS Ann Rheum Dis: first published as 10.1136/ard.62.1.88 on 1 January 2003. Downloaded from Severe septicaemia in a patient with polychondritis and Sweet’s syndrome after initiation of treatment with infliximab F G Matzkies, B Manger, M Schmitt-Haendle, T Nagel, H-G Kraetsch, J R Kalden, H Schulze-Koops ............................................................................................................................. Ann Rheum Dis 2003;62:81–82 D Sweet first described an acute febrile neutrophilic dermatosis in 1964 characterised by acute onset, fever, Rleucocytosis, and erythematous plaques.1 Skin biopsy specimens show infiltrates consisting of mononuclear cells and neutrophils with leucocytoclasis, but without signs of vasculi- tis. Sweet’s syndrome is frequently associated with solid malig- nancies or haemoproliferative disorders, but associations with chronic autoimmune connective tissue disorders have also been reported.2 The aetiology of Sweet’s syndrome is unknown, but evidence suggests that an immunological reaction of unknown specificity is the underlying mechanism. CASE REPORT A 51 year old white man with relapsing polychondritis (first diagnosed in 1997) was admitted to our hospital in June 2001 with a five week history of general malaise, fever, recurrent arthritis, and complaints of morning stiffness. Besides Figure 1 autoimmune polychondritis, he had insulin dependent Manifestation of Sweet’s syndrome in a patient with relapsing polychondritis. diabetes mellitus that was diagnosed in 1989. On admission, he presented with multiple small to medium, sharply demarked, raised erythematous plaques on both fore- dose of glucocorticoids (80 mg) and a second application of http://ard.bmj.com/ arms and lower legs, multiple acne-like pustules on the face, infliximab (3 mg/kg body weight) were given. -

Prescription Pattern of Primary Osteoarthritis in Tertiary Medical
Published online: 2020-04-21 Running title: Primary Osteoarthritis Nitte University Journal of Health Science Original Article Prescription Pattern of Primary Osteoarthritis in Tertiary Medical Centre Sowmya Sham Kanneppady1, Sham Kishor Kanneppady2, Vijaya Raghavan3, Aung Myo Oo4, Ohn Mar Lwin5 1Senior Lecturer and Head, Department of Pharmacology, Faculty of Medicine, Lincoln University College, Selangor Darul Ehsan, Malaysia, 2Senior Lecturer, School of Dentistry, International Medical University, Kuala Lumpur, Malaysia, 3Head of the Department of Pharmacology, KVG Medical College and Hospital, Kurunjibag, Sullia, Karnataka, India. 4Assistant Professor, Department of Biochemistry, Faculty of Medicine, Lincoln University College, Selangor Darul Ehsan, Malaysia, 5Post graduate student, Department of Physiology, Faculty of Medicine, University Malaya, Kuala Lumpur, Malaysia. *Corresponding Author : Sowmya Sham Kanneppady, Senior Lecturer and Head,Department of Pharmacology, Faculty of Medicine, Lincoln University College, No. 2, Jalan Stadium, SS 7/15, Kelana Jaya, 47301, Petaling Jaya, Selangor Darul Ehsan, Malaysia. E-mail : [email protected]. Received : 12.10.2017 Abstract Review Completed : 05.12.2017 Objectives: Osteoarthritis (OA) is one of the commonest joint/musculoskeletal disorders, Accepted : 06.12.2017 affecting the middle aged and elderly, although younger people may be affected as a result of injury or overuse. The study aimed to analyze the data, evaluate the prescription pattern and Keywords: Osteoarthritis, anti- rationality of the use of drugs in the treatment of primary OA with due emphasis on the inflammatory agents, prevalence available treatment regimens. Materials and methods: Medical case records of patients suffering from primary OA attending Access this article online the department of Orthopedics of a tertiary medical centre were the source of data. -

Acute < 6 Weeks Subacute ~ 6 Weeks Chronic >
Pain Articular Non-articular Localized Generalized . Regional Pain Disorders . Myalgias without Weakness Soft Tissue Rheumatism (ex., fibromyalgia, polymyalgia (ex., soft tissue rheumatism rheumatica) tendonitis, tenosynovitis, bursitis, fasciitis) . Myalgia with Weakness (ex., Inflammatory muscle disease) Clinical Features of Arthritis Monoarthritis Oligoarthritis Polyarthritis (one joint) (two to five joints) (> five joints) Acute < 6 weeks Subacute ~ 6 weeks Chronic > 6 weeks Inflammatory Noninflammatory Differential Diagnosis of Arthritis Differential Diagnosis of Arthritis Acute Monarthritis Acute Polyarthritis Inflammatory Inflammatory . Infection . Viral - gonococcal (GC) - hepatitis - nonGC - parvovirus . Crystal deposition - HIV - gout . Rheumatic fever - calcium . GC - pyrophosphate dihydrate (CPPD) . CTD (connective tissue diseases) - hydroxylapatite (HA) - RA . Spondyloarthropathies - systemic lupus erythematosus (SLE) - reactive . Sarcoidosis - psoriatic . - inflammatory bowel disease (IBD) Spondyloarthropathies - reactive - Reiters . - psoriatic Early RA - IBD - Reiters Non-inflammatory . Subacute bacterial endocarditis (SBE) . Trauma . Hemophilia Non-inflammatory . Avascular Necrosis . Hypertrophic osteoarthropathy . Internal derangement Chronic Monarthritis Chronic Polyarthritis Inflammatory Inflammatory . Chronic Infection . Bony erosions - fungal, - RA/Juvenile rheumatoid arthritis (JRA ) - tuberculosis (TB) - Crystal deposition . Rheumatoid arthritis (RA) - Infection (15%) - Erosive OA (rare) Non-inflammatory - Spondyloarthropathies -

Characterising the Risk of Major Bleeding in Patients With
EU PE&PV Research Network under the Framework Service Contract (nr. EMA/2015/27/PH) Study Protocol Characterising the risk of major bleeding in patients with Non-Valvular Atrial Fibrillation: non-interventional study of patients taking Direct Oral Anticoagulants in the EU Version 3.0 1 June 2018 EU PAS Register No: 16014 EMA/2015/27/PH EUPAS16014 Version 3.0 1 June 2018 1 TABLE OF CONTENTS 1 Title ........................................................................................................................................... 5 2 Marketing authorization holder ................................................................................................. 5 3 Responsible parties ................................................................................................................... 5 4 Abstract ..................................................................................................................................... 6 5 Amendments and updates ......................................................................................................... 7 6 Milestones ................................................................................................................................. 8 7 Rationale and background ......................................................................................................... 9 8 Research question and objectives .............................................................................................. 9 9 Research methods .................................................................................................................... -

Axial Spondyloarthritis
Central JSM Arthritis Review Article *Corresponding author Mali Jurkowski, Department of Internal Medicine, Temple University Hospital, 3401 North Broad Street, Axial Spondyloarthritis: Clinical Philadelphia, PA 19140, USA Submitted: 07 December 2020 Features, Classification, and Accepted: 31 January 2021 Published: 03 February 2021 ISSN: 2475-9155 Treatment Copyright Mali Jurkowski1*, Stephanie Jeong1 and Lawrence H Brent2 © 2021 Jurkowski M, et al. 1Department of Internal Medicine, Temple University Hospital, USA OPEN ACCESS 2Section of Rheumatology, Department of Medicine, Lewis Katz School of Medicine at Temple University, USA Keywords ABBREVIATIONS • Spondyloarthritis • Ankylosing spondylitis HLA-B27: human leukocyte antigen-B27; SpA: • HLA-B27 spondyloarthritis; AS: ankylosing spondylitis; nr-axSpA: non- • Classification criteria radiographic axial spondyloarthritis; ReA: reactive arthritis; PsA: psoriatic arthritis; IBD-SpA: disease associated spondyloarthritis; ASAS: Assessment of of rheumatoid arthritis [6]. AS affects men more than women SpondyloArthritis international Society; NSAIDs:inflammatory nonsteroidal bowel 79.6%, whereas nr-axSpA affects men and women equally 72.4% CASPAR: [7], independent of HLA-B27. This article will discuss the clinical for Psoriatic Arthritis; DMARDs: disease modifying anti- and diagnostic features of SpA, compare the classification criteria, rheumaticanti-inflammatory drugs; CD:drugs; Crohn’s disease; ClassificationUC: ulcerative Criteriacolitis; and provide updates regarding treatment options, including the ESR: erythrocyte sedimentation rate; CRP: C-reactive protein; developmentCLINICAL FEATURESof biologics and targeted synthetic agents. TNFi: X-ray: plain radiography; MRI: magnetic resonance imaging; CT: computed Inflammatory back pain tomography;tumor US: necrosis ultrasonography; factor-α wb-MRI:inhibitors; ESSG: European Spondyloarthropathy Study Group; IL-17i: whole-body MRI; JAKi: PDE4i: Inflammatory back pain is the hallmark of SpA, present in 70- 80% of patients [8]. -

Marble Bone Disease: a Rare Bone Disorder
Open Access Case Report DOI: 10.7759/cureus.339 Marble Bone Disease: A Rare Bone Disorder Eswaran Arumugam 1 , Maheswari Harinathbabu 2 , Ranjani Thillaigovindan 1 , Geetha Prabhu 1 1. Prosthodontics, Thai Moogambigai Dental College and Hospital 2. Oral Medicine and Radiology, Siva Multi Speciality Dental Clinic Corresponding author: Eswaran Arumugam, [email protected] Abstract Osteopetrosis, or marble bone disease, is a rare skeletal disorder due to a defective function of the osteoclasts. This defect renders bones more susceptible to osteomyelitis due to decreased vascularity. This disorder is inherited as autosomal dominant and autosomal recessive. Healthcare professionals should urge these patients to maintain their oral health as well as general health, as this condition makes these patients more susceptible to frequent infections and fractures. This case report emphasizes the signs and symptoms of marble bone disease and presents clinical and radiographic findings. Categories: Physical Medicine & Rehabilitation, Miscellaneous Keywords: osteopetrosis, marble bone disease, autosomal recessive, dense sclerotic bone Introduction Osteopetrosis (literally "stone bone," also known as marble bone disease or Albers-Schonberg disease) is an extremely rare inherited disorder where the bones harden and become denser. The disorder can cause osteosclerosis. The estimated prevalence of osteopetrosis is 1 in 100,000 to 500,000. It presents in two major clinical forms-a benign autosomal dominant form and a malignant autosomal recessive form. The autosomal dominant adult (benign) form is associated with few, if any, symptoms, and the autosomal recessive infantile (malignant) form is typically fatal during infancy or early childhood if untreated [1]. A rarer autosomal recessive (intermediate) form presents during childhood with some signs and symptoms of malignant osteopetrosis. -

Experiences of Rare Diseases: an Insight from Patients and Families
Experiences of Rare Diseases: An Insight from Patients and Families Unit 4D, Leroy House 436 Essex Road London N1 3QP tel: 02077043141 fax: 02073591447 [email protected] www.raredisease.org.uk By Lauren Limb, Stephen Nutt and Alev Sen - December 2010 Web and press design www.raredisease.org.uk WordsAndPeople.com About Rare Disease UK Rare Disease UK (RDUK) is the national alliance for people with rare diseases and all who support them. Our membership is open to all and includes patient organisations, clinicians, researchers, academics, industry and individuals with an interest in rare diseases. RDUK was established by Genetic RDUK is campaigning for a Alliance UK, the national charity strategy for integrated service of over 130 patient organisations delivery for rare diseases. This supporting all those affected by would coordinate: genetic conditions, in conjunction with other key stakeholders | Research in November 2008 following the European Commission’s | Prevention and diagnosis Communication on Rare Diseases: | Treatment and care Europe’s Challenges. | Information Subsequently RDUK successfully | Commissioning and planning campaigned for the adoption of the Council of the European into one cohesive strategy for all Union’s Recommendation on patients affected by rare disease in an action in the field of rare the UK. As well as securing better diseases. The Recommendation outcomes for patients, a strategy was adopted unanimously by each would enable the most effective Member State of the EU (including use of NHS resources. the -

Hypophosphatasia: Current Literature for Pathophysiology, Clinical Manifestations, Diagnosis, and Treatment
Open Access Review Article DOI: 10.7759/cureus.8594 Hypophosphatasia: Current Literature for Pathophysiology, Clinical Manifestations, Diagnosis, and Treatment Abdulai Bangura 1 , Lisa Wright 2 , Thomas Shuler 2 1. Department of Research, Trinity School of Medicine, Ratho Mill, VCT 2. Department of Orthopaedics, Carilion Clinic, Roanoke, USA Corresponding author: Abdulai Bangura, [email protected] Abstract Hypophosphatasia (HPP) is a rare inherited bone disorder identified by impaired bone mineralization. There are seven subtypes of HPP mainly characterized by their age of onset. These subtypes consist of perinatal (prenatal) benign, perinatal lethal, infantile, childhood, adult, odontohypophosphatasia, and pseudohypophosphatasia. Due to limited awareness of the condition, either misdiagnosis or delayed diagnosis is common. Furthermore, the condition is frequently treated with contraindicated drugs. This literature illustrates the most recent findings on the etiology, pathophysiology, clinical manifestations, diagnosing, and treatment for HPP and its subtypes. The etiology of the disease consists of loss-of-function mutations of the ALPL gene on chromosome one, which encodes for tissue nonspecific isoenzyme of alkaline phosphatase (TNAP). A decrease of TNAP reduces inorganic phosphate (Pi) for bone mineralization and allows for an increase in inorganic pyrophosphate (PPi) and phosphorylated osteopontin (p-OPN), which further reduces bone mineralization. The combination of these processes softens bone and mediates a clinical presentation similar to rickets/osteomalacia. HPP has an additional wide range of clinical features depending on its subtype. Although a concrete diagnostic guideline has not yet been established, many studies have supported a similar method of identifying HPP. Clinical features, radiological findings, and/or biomarker levels of the disorder should raise suspicion and encourage the inclusion of HPP as a differential diagnosis. -
PMBJP Product.Pdf
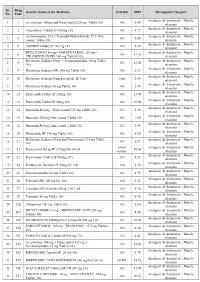
Sr. Drug Generic Name of the Medicine Unit Size MRP Therapeutic Category No. Code Analgesic & Antipyretic / Muscle 1 1 Aceclofenac 100mg and Paracetamol 325 mg Tablet 10's 10's 8.00 relaxants Analgesic & Antipyretic / Muscle 2 2 Aceclofenac Tablets IP 100mg 10's 10's 4.37 relaxants Acetaminophen 325 + Tramadol Hydrochloride 37.5 film Analgesic & Antipyretic / Muscle 3 4 10's 8.00 coated Tablet 10's relaxants Analgesic & Antipyretic / Muscle 4 5 ASPIRIN Tablets IP 150 mg 14's 14's 2.70 relaxants DICLOFENAC 50 mg+ PARACETAMOL 325 mg+ Analgesic & Antipyretic / Muscle 5 6 10's 11.30 CHLORZOXAZONE 500 mg Tablets 10's relaxants Diclofenac Sodium 50mg + Serratiopeptidase 10mg Tablet Analgesic & Antipyretic / Muscle 6 8 10's 12.00 10's relaxants Analgesic & Antipyretic / Muscle 7 9 Diclofenac Sodium (SR) 100 mg Tablet 10's 10's 6.12 relaxants Analgesic & Antipyretic / Muscle 8 10 Diclofenac Sodium 25mg per ml Inj. IP 3 ml 3 ml 2.00 relaxants Analgesic & Antipyretic / Muscle 9 11 Diclofenac Sodium 50 mg Tablet 10's 10's 2.90 relaxants Analgesic & Antipyretic / Muscle 10 12 Etoricoxilb Tablets IP 120mg 10's 10's 33.00 relaxants Analgesic & Antipyretic / Muscle 11 13 Etoricoxilb Tablets IP 90mg 10's 10's 25.00 relaxants Analgesic & Antipyretic / Muscle 12 14 Ibuprofen 400 mg + Paracetamol 325 mg Tablet 10's 15's 5.50 relaxants Analgesic & Antipyretic / Muscle 13 15 Ibuprofen 200 mg film coated Tablet 10's 10's 1.80 relaxants Analgesic & Antipyretic / Muscle 14 16 Ibuprofen 400 mg film coated Tablet 10's 15's 3.50 relaxants Analgesic & Antipyretic -

Osteomalacia and Osteoporosis D
Postgrad. med.J. (August 1968) 44, 621-625. Postgrad Med J: first published as 10.1136/pgmj.44.514.621 on 1 August 1968. Downloaded from Osteomalacia and osteoporosis D. B. MORGAN Department of Clinical Investigation, University ofLeeds OSTEOMALACIA and osteoporosis are still some- in osteomalacia is an increase in the alkaline times confused because both diseases lead to a phosphatase activity in the blood (SAP); there deficiency of calcium which can be detected on may also be a low serum phosphorus or a low radiographs of the skeleton. serum calcium. This lack of calcium is the only feature Our experience with the biopsy of bone is that common to the two diseases which are in all a large excess of uncalcified bone tissue (osteoid), other ways easily distinguishable. which is the classic histological feature of osteo- malacia, is only found in patients with the other Osteomalacia typical features of the disease, in particular the Osteomalacia will be discussed first, because it clinical ones (Morgan et al., 1967a). Whether or is a clearly defined disease which can be cured. not more subtle histological techniques will detect Osteomalacia is the result of an imbalance be- earlier stages of the disease remains to be seen. tween the supply of and the demand for vitamin Bone pains, muscle weakness, Looser's zones, D. The the following description of disease is raised SAP and low serum phosphate are the Protected by copyright. based on our experience of twenty-two patients most reliable aids to the diagnosis of osteomalacia, with osteomalacia after gastrectomy; there is no and approximately in that order. -

A Resident's Guide to Pediatric Rheumatology
A RESIDENT’S GUIDE TO PEDIATRIC RHEUMATOLOGY 4th Revised Edition - 2019 A RESIDENT’S GUIDE TO PEDIATRIC RHEUMATOLOGY This guide is intended to provide a brief introduction to basic topics in pediatric rheumatology. Each topic is accompanied by at least one up-to-date reference that will allow you to explore the topic in greater depth. In addition, a list of several excellent textbooks and other resources for you to use to expand your knowledge is found in the Appendix. We are interested in your feedback on the guide! If you have comments or questions, please feel free to contact us via email at [email protected]. Supervising Editors: Dr. Ronald M. Laxer, SickKids Hospital, University of Toronto Dr. Tania Cellucci, McMaster Children’s Hospital, McMaster University Dr. Evelyn Rozenblyum, St. Michael’s Hospital, University of Toronto Section Editors: Dr. Michelle Batthish, McMaster Children’s Hospital, McMaster University Dr. Roberta Berard, Children’s Hospital – London Health Sciences Centre, Western University Dr. Liane Heale, McMaster Children’s Hospital, McMaster University Dr. Clare Hutchinson, North York General Hospital, University of Toronto Dr. Mehul Jariwala, Royal University Hospital, University of Saskatchewan Dr. Lillian Lim, Stollery Children’s Hospital, University of Alberta Dr. Nadia Luca, Alberta Children’s Hospital, University of Calgary Dr. Dax Rumsey, Stollery Children’s Hospital, University of Alberta Dr. Gordon Soon, North York General Hospital and SickKids Hospital Northern Clinic in Sudbury, University