Conflict of Interest Learner Outcome Objectives
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Episode 35 - Pediatric Orthopedics - Emergencymedicinecases.Com
EPISODE 35 - PEDIATRIC ORTHOPEDICS - EMERGENCYMEDICINECASES.COM KNEE INJURIES: Check the X-ray for a Segond fracture, a vertically oriented In general, children’s ligaments are avulsion fracture off the lateral stronger than their bones, thus proximal tibia. This is highly fractures are more likely than associated with ACL and meniscal sprains. Have a low threshold for tears. (See page 4 for a picture.) imaging if suspicious. Management of ACL tears: The same ACL-injury mechanism (sudden deceleration - pain management in acute phase of distal leg with forward and (NSAIDs, tylenol, morphine) rotatory movement) will cause a - short term immobilization (splint EPISODE 35: tibial spine fracture in a as needed, +/-crutches), but PEDIATRIC ORTHOPEDICS younger child, and an ACL tear in atrophy of quadriceps occurs WITH DR. SANJAY MEHTA & a teenager or adult. (See page 4 for quickly, so start range of motion in DR. JONATHAN PIRIE a photo of a tibial spine fracture.) 2–3 days. Some experts Patellar subluxations: the child Lachman test for ACL tear recommend weight bearing as may feel a “pop”, from the kneecap involves pulling the proximal tibia tolerated immediately. subluxing, and feel unstable on the anteriorly while holding the knee in - Surgical repair is delayed until leg. First time patella dislocations flexion. It has good sensitivity (>80% range of motion has recovered. and non-displaced fractures do and specificity of 95%) (1). The Refer to outpatient orthopedics. need knee immobilization, pivot shift test (valgus force and with weight bearing as tolerated. internal rotation to extended leg, Displaced fractures or fractures with which is then flexed to feel Additional X-ray views: an impaired extensor mechanism subluxation) is also sensitive for ACL - patellar injury requires a “skyline need urgent orthopedic tear. -

Ottawa Knee Rule: Investigating Use and Application in a Tertiary Teaching Hospital
Open Access Original Article DOI: 10.7759/cureus.8812 Ottawa Knee Rule: Investigating Use and Application in a Tertiary Teaching Hospital Abubakr Mohamed 1 , Elkhidir Babikir 1 , Mohamed Kamal Elbashir Mustafa 2 1. Emergency Medicine, University Hospital Galway, Galway, IRL 2. Vascular Surgery, University Hospital Galway, Galway, IRL Corresponding author: Abubakr Mohamed, [email protected] Abstract Background Knee injuries are encountered commonly in the emergency departments (EDs) in Ireland. Validated clinical decision rules such as Ottawa knee rule (OKR) can be used in acute knee injury settings to reduce the number of unnecessary radiography. Clinical judgment can be used to distinguish between suspected fractures and non-fractures in many cases; however, radiography is still routinely requested. Objectives We evaluated the OKRs in a high-volume tertiary teaching hospital in Ireland to determine whether the rule could be safely used to decide whether patients with acute blunt knee trauma should undergo radiography. Methods This was an observational study conducted in the ED over a three-month period in a tertiary referral hospital. A total of 110 patients with acute knee injuries were examined using OKR. Inclusion criteria included patients with acute knee injuries due to blunt trauma or twisting injury and patients with lacerations or contusions. Open fractures and fractures due to penetrating injury were excluded from the study. Results Fractures were seen in 12 (13.2%) of the 110 patents who met the inclusion criteria. The OKR predicted all 12 fractures. Sensitivity was 100%, and specificity was 39%. Conclusions Received 06/04/2020 Review began 06/18/2020 The OKR is highly sensitive for fracture in this setting and can be safely used to decide whether Review ended 06/21/2020 patients with acute blunt knee trauma should undergo radiography. -
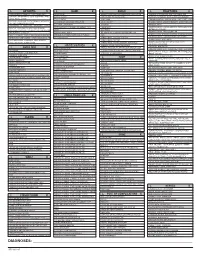
ICD-10 Diagnoses on Router
L ARTHRITIS R L HAND R L ANKLE R L FRACTURES R OSTEOARTHRITIS: PRIMARY, 2°, POST TRAUMA, POST _____ CONTUSION ACHILLES TEN DYSFUNCTION/TENDINITIS/RUPTURE FLXR TEN CLAVICLE: STERNAL END, SHAFT, ACROMIAL END CRYSTALLINE ARTHRITIS: GOUT: IDIOPATHIC, LEAD, CRUSH INJURY AMPUTATION TRAUMATIC LEVEL SCAPULA: ACROMION, BODY, CORACOID, GLENOID DRUG, RENAL, OTHER DUPUYTREN’S CONTUSION PROXIMAL HUMERUS: SURGICAL NECK 2 PART 3 PART 4 PART CRYSTALLINE ARTHRITIS: PSEUDOGOUT: HYDROXY LACERATION: DESCRIBE STRUCTURE CRUSH INJURY PROXIMAL HUMERUS: GREATER TUBEROSITY, LESSER TUBEROSITY DEP DIS, CHONDROCALCINOSIS LIGAMENT DISORDERS EFFUSION HUMERAL SHAFT INFLAMMATORY: RA: SEROPOSITIVE, SERONEGATIVE, JUVENILE OSTEOARTHRITIS PRIMARY/SECONDARY TYPE _____ LOOSE BODY HUMERUS DISTAL: SUPRACONDYLAR INTERCONDYLAR REACTIVE: SECONDARY TO: INFECTION ELSEWHERE, EXTENSION OR NONE INTESTINAL BYPASS, POST DYSENTERIC, POST IMMUNIZATION PAIN OCD TALUS HUMERUS DISTAL: TRANSCONDYLAR NEUROPATHIC CHARCOT SPRAIN HAND: JOINT? OSTEOARTHRITIS PRIMARY/SECONDARY TYPE _____ HUMERUS DISTAL: EPICONDYLE LATERAL OR MEDIAL AVULSION INFECT: PYOGENIC: STAPH, STREP, PNEUMO, OTHER BACT TENDON RUPTURES: EXTENSOR OR FLEXOR PAIN HUMERUS DISTAL: CONDYLE MEDIAL OR LATERAL INFECTIOUS: NONPYOGENIC: LYME, GONOCOCCAL, TB TENOSYNOVITIS SPRAIN, ANKLE, CALCANEOFIBULAR ELBOW: RADIUS: HEAD NECK OSTEONECROSIS: IDIOPATHIC, DRUG INDUCED, SPRAIN, ANKLE, DELTOID POST TRAUMATIC, OTHER CAUSE SPRAIN, ANKLE, TIB-FIB LIGAMENT (HIGH ANKLE) ELBOW: OLECRANON WITH OR WITHOUT INTRA ARTICULAR EXTENSION SUBLUXATION OF ANKLE, -
Clinical Excellence Series Volume V an Evidence-Based Approach to Traumatic Emergencies
Clinical Excellence Series n Volume V An Evidence-Based Approach To Traumatic Emergencies Inside Neck Trauma: Don’t Put Your Neck On The Line Orthopedic Sports Injuries: Off The Sidelines And Into The Emergency Department Blunt Abdominal Trauma: Priorities, Procedures, And Pragmatic Thinking Wrist Injuries: Emergency Imaging And Management Brought to you exclusively by the publisher of: An Evidence-Based Approach To Traumatic Emergencies CEO: Robert Williford President & Publisher: Stephanie Ivy Associate Editor & CME Director: Jennifer Pai • Associate Editor: Dorothy Whisenhunt Director of Member Services: Liz Alvarez • Marketing & Customer Service Coordinator: Robin Williford Direct all questions to EB Medicine: 1-800-249-5770 • Fax: 1-770-500-1316 • Non-U.S. subscribers, call: 1-678-366-7933 EB Medicine • 5550 Triangle Pkwy Ste 150 • Norcross, GA 30092 E-mail: [email protected] • Web Site: www.ebmedicine.net The Emergency Medicine Practice Clinical Excellence Series, Volume V: An Evidence-Based Approach To Traumatic Emergencies is published by EB Practice, LLC, 5550 Triangle Pkwy Ste 150, Norcross, GA 30092. Opinions expressed are not necessarily those of this publication. Mention of products or services does not constitute endorsement. This publication is intended as a general guide and is intended to supplement, rather than substitute, professional judgment. It covers a highly technical and complex subject and should not be used for making specific medical decisions. The materials contained herein are not intended to establish policy, procedure, or standard of care. Emergency Medicine Practice, The Emergency Medicine Practice Clinical Excel- lence Series, and An Evidence-Based Approach to Traumatic Emergencies are trademarks of EB Practice, LLC. -

Upper Extremity
Upper Extremity Shoulder Elbow Wrist/Hand Diagnosis Left Right Diagnosis Left Right Diagnosis Left Right Adhesive capsulitis M75.02 M75.01 Anterior dislocation of radial head S53.015 [7] S53.014 [7] Boutonniere deformity of fingers M20.022 M20.021 Anterior dislocation of humerus S43.015 [7] S43.014 [7] Anterior dislocation of ulnohumeral joint S53.115 [7] S53.114 [7] Carpal Tunnel Syndrome, upper limb G56.02 G56.01 Anterior dislocation of SC joint S43.215 [7] S43.214 [7] Anterior subluxation of radial head S53.012 [7] S53.011 [7] DeQuervain tenosynovitis M65.42 M65.41 Anterior subluxation of humerus S43.012 [7] S43.011 [7] Anterior subluxation of ulnohumeral joint S53.112 [7] S53.111 [7] Dislocation of MCP joint IF S63.261 [7] S63.260 [7] Anterior subluxation of SC joint S43.212 [7] S43.211 [7] Contracture of muscle in forearm M62.432 M62.431 Dislocation of MCP joint of LF S63.267 [7] S63.266 [7] Bicipital tendinitis M75.22 M75.21 Contusion of elbow S50.02X [7] S50.01X [7] Dislocation of MCP joint of MF S63.263 [7] S63.262 [7] Bursitis M75.52 M75.51 Elbow, (recurrent) dislocation M24.422 M24.421 Dislocation of MCP joint of RF S63.265 [7] S63.264 [7] Calcific Tendinitis M75.32 M75.31 Lateral epicondylitis M77.12 M77.11 Dupuytrens M72.0 Contracture of muscle in shoulder M62.412 M62.411 Lesion of ulnar nerve, upper limb G56.22 G56.21 Mallet finger M20.012 M20.011 Contracture of muscle in upper arm M62.422 M62.421 Long head of bicep tendon strain S46.112 [7] S46.111 [7] Osteochondritis dissecans of wrist M93.232 M93.231 Primary, unilateral -

What Is the Best Way to Evaluate an Acute Traumatic Knee Injury?
From the CLINICAL INQUIRIES Family Physicians Inquiries Network Matthew L. Silvis, MD, C. Randall Clinch, DO, MS, What is the best way and Janine S. Tillet, MSLS Wake Forest University, to evaluate an acute Winston-Salem, NC traumatic knee injury? Evidence-based answer Use the Ottawa Knee Rules. When there or ligamentous injury (SOR: C, based on is a possibility of fracture, they can guide studies of intermediate outcomes). the use of radiography in adults who Sonographic examination of a present with isolated knee pain. However, traumatized knee can accurately detect information on use of these rules in the internal knee derangement (SOR: C, pediatric population is limited (strength based on studies of intermediate of recommendation [SOR]: A, based on outcomes). Magnetic resonance imaging systematic review of high-quality studies (MRI) of the knee is the noninvasive and a validated clinical decision rule). standard for diagnosing internal knee Specific physical examination maneuvers derangement, and it is useful for both adult (such as the Lachman and McMurray tests) and pediatric patients (SOR: C, based on FAST TRACK may be helpful when assessing for meniscal studies of intermediate outcomes). Employ the Clinical commentary Ottawa Knee Rules Ottawa rules for ankles—yes, test, Drawer sign, and McMurray test to determine but they’re good for knees, too are useful in diagnosing the presence of whether plain The evidence presented here suggests internal ligamentous injuries without MRI, x-rays are needed a number of practical and useful and an ultrasound can help to detect knee to rule out fracture approaches for the evaluation of acute effusion when it is not clinically obvious. -
EM Cases Digest Vol. 1 MSK & Trauma
THE MAGAZINE SERIES FOR ENHANCED EM LEARNING Vol. 1: MSK & Trauma Copyright © 2015 by Medicine Cases Emergency Medicine Cases by Medicine Cases is copyrighted as “All Rights Reserved”. This eBook is Creative Commons Attribution-NonCommercial- NoDerivatives 3.0 Unsupported License. Upon written request, however, we may be able to share our content with you for free in exchange for analytic data. For permission requests, write to the publisher, addressed “Attention: Permissions Coordinator,” at the address below. Medicine Cases 216 Balmoral Ave Toronto, ON, M4V 1J9 www.emergencymedicinecases.com This book has been authored with care to reflect generally accepted practices. As medicine is a rapidly changing field, new diagnostic and treatment modalities are likely to arise. It is the responsibility of the treating physician, relying on his/her experience and the knowledge of the patient, to determine the best management plan for each patient. The author(s) and publisher of this book are not responsible for errors or omissions or for any consequences from the application of the information in this book and disclaim any liability in connection with the use of this information. This book makes no guarantee with respect to the completeness or accuracy of the contents within. OUR THANKS TO... EDITORS IN CHIEF Anton Helman Taryn Lloyd PRODUCTION EDITOR Michelle Yee PRODUCTION MANAGER Garron Helman CHAPTER EDITORS Niran Argintaru Michael Misch PODCAST SUMMARY EDITORS Lucas Chartier Keerat Grewal Claire Heslop Michael Kilian PODCAST GUEST EXPERTS Andrew Arcand Natalie Mamen Brian Steinhart Mike Brzozowski Hossein Mehdian Arun Sayal Ivy Cheng Sanjay Mehta Laura Tate Walter Himmel Jonathan Pirie Rahim Valani Dave MacKinnon Jennifer Riley University of Toronto, Faculty of Medicine EM Cases is a venture of the Schwartz/ Reisman Emergency Medicine Institute. -

2014 Newsletter – Winter
NEWS ISSUE 14 I WINTER 2014 Welcome to our Winter edition of Orthosports News Winter is the time when Alpine Injuries present themselves WHO ORTHOSPORTS – Dr Doron Sher covers the most common types of alpine ARE WE? LOCATIONS injuries. Dr Kwan Yeoh takes a look at Mallet Finger and Orthosports is > Concord 02 9744 2666 “Imaging of the knee” is covered by Dr Sher in our Key a professional > Hurstville 02 9580 6066 Examination Points Section. association of > Penrith 02 4721 7799 Many GPs have attended our Category 1 Education Modules; AOA Orthopaedic > Randwick 02 9399 5333 A USTRAL I A N ORTHOPA EDIC Surgeons based Or visit our website there are 4 remaining dates for our 2014 RACGP approved A S S O CIA T I O N modules. See page 4 for details. in Sydney. www.orthosports.com.au We hope you enjoy this issue – The Team at Orthosports elbow injuries and more comminuted clavicle fractures. Alpine Injuries Shoulder dislocation is also very common. Snowboarders do not usually injure their legs when both feet are attached Skiing and snowboarding are exhilarating sports. They to the board but injuries to the knee are not uncommon are physically demanding and require co-ordination, getting on and off lifts when only one foot is bound to the strength, fitness and lots of specialized equipment. More board (more common in beginners). If they do injure their people ski than snowboard and snowboarders are generally knee, it is almost always in a terrain park landing from younger than skiers. Skiing and snowboarding injuries a big jump. -

Hughston Health Alert US POSTAGE PAID the Hughston Foundation, Inc
HughstonHughston HealthHealth AlertAlert 6262 Veterans Parkway, PO Box 9517, Columbus, GA 31908-9517 • www.hughston.com/hha VOLUME 26, NUMBER 4 - FALL 2014 Fig. 1. Knee Inside... anatomy and • Rotator Cuff Disease ACL injury. Extended (straight) knee • Bunions and Lesser Toe Deformities Femur • Tendon Injuries of the Hand (thighbone) Patella In Perspective: (kneecap) Anterior Cruciate Ligament Tears Medial In 1992, Dr. Jack C. Hughston (1917-2004), one of the meniscus world’s most respected authorities on knee ligament surgery, MCL LCL shared some of his thoughts regarding injuries to the ACL. (medial “You tore your anterior cruciate ligament.” On hearing (lateral collateral collateral your physician speak those words, you are filled with a sense ligament) of dread. You envision the end of your athletic life, even ligament) recreational sports. Today, a torn ACL (Fig. 1) has almost become a household Tibia word. Through friends, newspapers, television, sports Fibula (shinbone) magazines, and even our physicians, we are inundated with the hype that the knee joint will deteriorate and become arthritic if the ACL is not operated on as soon as possible. You have been convinced that to save your knee you must Flexed (bent) knee have an operation immediately to repair the ligament. Your surgery is scheduled for the following day. You are scared. Patella But there is an old truism in orthopaedic surgery that says, (kneecap) “no knee is so bad that it can’t be made worse by operating Articular Torn ACL on it.” cartilage (anterior For many years, torn ACLs were treated as an emergency PCL cruciate and were operated on immediately, even before the initial (posterior ligament) pain and swelling of the injury subsided. -

Knee Injuries
6/11/2019 Tintinalli’s Emergency Medicine: A Comprehensive Study Guide, 8e Chapter 274: Knee Injuries Rachel R. Bengtzen; Jerey N. Glaspy; Mark T. Steele ANATOMY The knee consists of two joints, the tibiofemoral joint and the patellofemoral joint. Within the tibiofemoral joint, the distal femur (comprised of the medial and lateral femoral condyles) articulates with the proximal tibia (comprised of the medial and lateral tibial condyles) (Figure 274-1). The medial and lateral menisci are situated between the articular surfaces, and the menisci provide cushion, lubrication, and resistance to articular wear (Figure 274-2). In the patellofemoral joint, the patella articulates with the distal femur along the anterior depression called the patellofemoral groove during flexion and extension of the knee. The patella is stabilized by the patellar tendon and medial retinaculum. FIGURE 274-1. The supracondylar and condylar areas of the femur, and the medial and subcondylar areas of the tibia. 1/29 6/11/2019 FIGURE 274-2. Ligaments of the right knee joint. The articular capsule and the patella have been removed. 2/29 6/11/2019 There are four ligaments in the knee: the anterior cruciate ligament, the posterior cruciate ligament, and the medial and lateral collateral ligaments (Figure 274-2). These ligaments provide strength and stability to the knee. The posterior aspect of the knee, the popliteal fossa, contains the popliteal artery and vein, the common peroneal nerve, and the tibial nerve (Figure 274-3). FIGURE 274-3. Posterior knee: popliteal fossa anatomy. 3/29 6/11/2019 CLINICAL FEATURES Determine the mechanism of knee injury and review all prior orthopedic injuries or surgical procedures. -

Hand Rehabilitation Current Awareness Newsletter
1 Hand Rehabilitation Current Awareness Newsletter JANUARY 2016 2 Your Local Librarian Whatever your information needs, the library is here to help. As your outreach librarian I offer literature searching services as well as training and guidance in searching the evidence and critical appraisal – just email me at library @uhbristol.nhs.uk OUTREACH: Your Outreach Librarian can help facilitate evidence-based practise for all in the Orthogeriatrics team, as well as assisting with academic study and research. We can help with literature searching, obtaining journal articles and books, and setting up individual current awareness alerts. We also offer one-to-one or small group training in literature searching, accessing electronic journals, and critical appraisal. Get in touch: [email protected] LITERATURE SEARCHING: We provide a literature searching service for any library member. For those embarking on their own research it is advisable to book some time with one of the librarians for a 1 to 1 session where we can guide you through the process of creating a well-focused literature research and introduce you to the health databases access via NHS Evidence. Please email requests to [email protected] 3 Contents New from Cochrane Database of Systematic Reviews ........................................................................... 4 Abstract .................................................................................................................................................. 4 New Activity in Up-to-Date .................................................................................................................... -
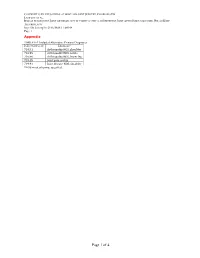
Page 1 of 4 COPYRIGHT © by the JOURNAL of BONE and JOINT SURGERY, INCORPORATED LAMPLOT ET AL
COPYRIGHT © BY THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED LAMPLOT ET AL. RISK OF SUBSEQUENT JOINT ARTHROPLASTY IN CONTRALATERAL OR DIFFERENT JOINT AFTER INDEX SHOULDER, HIP, OR KNEE ARTHROPLASTY http://dx.doi.org/10.2106/JBJS.17.00948 Page 1 Appendix TABLE E-1 Included Alternative Primary Diagnoses ICD-9-CM Code Diagnosis* 716.91 Arthropathy NOS, shoulder 716.95 Arthropathy NOS, pelvis 716.96 Arthropathy NOS, lower leg 719.45 Joint pain, pelvis 719.91 Joint disease NOS, shoulder *NOS = not otherwise specified. Page 1 of 4 COPYRIGHT © BY THE JOURNAL OF BONE AND JOINT SURGERY, INCORPORATED LAMPLOT ET AL. RISK OF SUBSEQUENT JOINT ARTHROPLASTY IN CONTRALATERAL OR DIFFERENT JOINT AFTER INDEX SHOULDER, HIP, OR KNEE ARTHROPLASTY http://dx.doi.org/10.2106/JBJS.17.00948 Page 2 TABLE E-2 Excluded Diagnoses* ICD-9- ICD-9- ICD-9- ICD-9- CM Code Diagnosis CM Code Diagnosis CM Code Diagnosis CM Code Diagnosis 274 Gouty arthropathy NOS 696 Psoriatic 711.03 Pyogen 711.38 Dysenter arthropathy arthritis- arthritis NEC forearm 274.01 Acute gouty arthropathy 696.1 Other psoriasis 711.04 Pyogen 711.4 Bact arthritis- arthritis-hand unspec 274.02 Chr gouty arthropathy 696.2 Parapsoriasis 711.05 Pyogen 711.46 Bact arthritis- w/o tophi arthritis-pelvis l/leg 274.03 Chr gouty arthropathy w 696.3 Pityriasis rosea 711.06 Pyogen 711.5 Viral arthritis- tophi arthritis-l/leg unspec 274.1 Gouty nephropathy NOS 696.4 Pityriasis rubra 711.07 Pyogen 711.55 Viral arthritis- pilaris arthritis-ankle pelvis 274.11 Uric acid nephrolithiasis 696.5 Pityriasis NEC & 711.08