Sitakunda Upazila Chittagong District Bangladesh
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Annual Report 2016-17 CONTENTS
Annual Report 2016-17 CONTENTS Introduction 03 Vision & Mission 04 Our Values 05 Transmittal Letter 06 Notice of the 11th Annual General Meeting 07 Corporate Information 08-09 Board of Directors Prole 10-15 Management Team 17 Chairman's Message 18-19 Message from the Managing Director 20-21 Comparative Graphical Presentation 22-23 Board of Directors' Report (English Version) 24-30 Board of Directors' Report (Bengali Version) 31-36 Annexure to Directors' Report 37-46 Audit Committee Report 47 Value Added Statement 48 Statutory Auditors' Report along with Financial Statements 49-84 Certicates 85-88 Events Album 89-93 News Board 94 Form of Proxy 95-96 02 Annual Report 2016-17 GOD FEARING PLAIN LIVING HIGH THINKING "In the beginning God created man" and after thousand years of intelligence, precision, hard work and innovation, man created steel - one of the greatest innovations of all time. This super-strong, carbonized and alloyed form of iron is an element without which modern life is literally unimaginable. From skyscrapers and planes to syringes and forks, steel is an essential part of our everyday life. GPH ispat ltd. One of the leaders of Bangladesh in manufacturing steel promises a super strong future and economy with its world class products. Not only structural bar, but GPH Ispat Ltd is also one of the producers of low & medium carbon and low alloy steel billets in Bangladesh, the main ingredients of manufacturing graded steel bar. As GPH is ensuring the highest quality products in Bangladesh as per various international and national standards, GPH steel billets and bars are getting exported to other countries after nourishing national demand. -

Bangladesh Workplace Death Report 2020
Bangladesh Workplace Death Report 2020 Supported by Published by I Bangladesh Workplace Death Report 2020 Published by Safety and Rights Society 6/5A, Rang Srabonti, Sir Sayed Road (1st floor), Block-A Mohammadpur, Dhaka-1207 Bangladesh +88-02-9119903, +88-02-9119904 +880-1711-780017, +88-01974-666890 [email protected] safetyandrights.org Date of Publication April 2021 Copyright Safety and Rights Society ISBN: Printed by Chowdhury Printers and Supply 48/A/1 Badda Nagar, B.D.R Gate-1 Pilkhana, Dhaka-1205 II Foreword It is not new for SRS to publish this report, as it has been publishing this sort of report from 2009, but the new circumstances has arisen in 2020 when the COVID 19 attacked the country in March . Almost all the workplaces were shut about for 66 days from 26 March 2020. As a result, the number of workplace deaths is little bit low than previous year 2019, but not that much low as it is supposed to be. Every year Safety and Rights Society (SRS) is monitoring newspaper for collecting and preserving information on workplace accidents and the number of victims of those accidents and publish a report after conducting the yearly survey – this year report is the tenth in the series. SRS depends not only the newspapers as the source for information but it also accumulated some information from online media and through personal contact with workers representative organizations. This year 26 newspapers (15 national and 11 regional) were monitored and the present report includes information on workplace deaths (as well as injuries that took place in the same incident that resulted in the deaths) throughout 2020. -

BANGABANDHU SHEIKH MUJIB SHILPANAGAR Mirsarai-Sitakundu-Sonagazi Chattogram-Feni
BANGABANDHU SHEIKH MUJIB SHILPANAGAR Mirsarai-Sitakundu-Sonagazi Chattogram-Feni Bangladesh Economic Zones Authority (BEZA) BANGABANDHU SHEIKH MUJIB SHILPANAGAR EDITORIAL BOARD Paban Chowdhury, Executive Chairman, BEZA Md. Harunur Rashid, Executive Member, BEZA Mohammad Hasan Arif, General Manager, BEZA Shenjuti Barua, Deputy Manager, BEZA Md. Abdul Quader Khan, Social Consultant, BEZA PUBLISHED IN May 2020 PUBLISHER Bangladesh Economic Zones Authority (BEZA) Prime Minister’s Office DESIGN AND PRINTING Nymphea Publication © Bangladesh Economic Zones Authority (BEZA) All rights reserved. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form or by any means, electronic, mechanical, photocopying recording or otherwise without prior permission of the publisher. The book is sold subject to the condition that it shall not, by way of trade or otherwise, be lent, re-sold, or otherwise circulated without the publisher's prior consent in any form of binding or cover, other than that in which it is published. 4 Bangabandhu Sheikh Mujib Shilpanagar gyw³i msMªv‡gi †P‡qI †`k Movi msMÖvg KwVb, ZvB †`k Movi Kv‡R Avgv‡`i me©kw³ wb‡qvM Ki‡Z n‡e - e½eÜz †kL gywReyi ingvb PRIME MINISTER Government of the People’s Republic of Bangladesh 10 Falgun 1426 MESSAGE 23 February 2020 I am happy to know that Bangladesh Economic Zones Authority (BEZA) is the establishment of Bangabandhu Sheikh Mujib Shilpanagar (BSMSN) publishing a book on the development scenario of Bangabandhu Shekih comprising Mirsarai, Feni and Sitakunda Economic Zones, on 30,000 Mujib Shilpanagar (BSMSN) covering some excellent accomplishments acres of land has created a hilarious prospect among the local and experienced so far. -
Brahmanbaria District Joint Need Assessment Report, 2013
Tornado in North Eastern Bangladesh: Brahmanbaria District Joint Need Assessment Report, 2013 Assessment conducted jointly by Shelter Cluster WASH Cluster Early Recovery Cluster 1 Table of Contents Executive Summary....................................................................................................... 6 Recommended Interventions......................................................................................... 8 Background.................................................................................................................... 10 Assessment Methodology.............................................................................................. 12 Key Findings.................................................................................................................. 14 Priorities identified by Upazila Officials.......................................................................... 18 Detailed Assessment Findings...................................................................................... 20 Shelter........................................................................................................................ 20 Water Sanitation & Hygiene....................................................................................... 20 Livelihoods.................................................................................................................. 21 Education.................................................................................................................... 24 -

IPP: Bangladesh: Second Chittagong Hill Tracts Rural Development Project
Second Chittagong Hill Tracts Rural Development Project (RRP BAN 42248) Indigenous Peoples Plan March 2011 BAN: Second Chittagong Hill Tracts Rural Development Project Prepared by ANZDEC Ltd for the Ministry of Chittagong Hill Tracts Affairs and Asian Development Bank. CURRENCY EQUIVALENTS (as of 16 March 2011) Currency unit – taka (Tk) Tk1.00 = $0.0140 $1.00 = Tk71.56 ABBREVIATIONS ADB – Asian Development Bank ADR – alternative dispute resolution AP – affected person CHT – Chittagong Hill Tracts CHTDF – Chittagong Hill Tracts Development Facility CHTRC – Chittagong Hill Tracts Regional Council CHTRDP – Chittagong Hill Tracts Rural Development Project CI – community infrastructure DC – deputy commissioner DPMO – district project management office GOB – Government of Bangladesh GPS – global positioning system GRC – grievance redress committee HDC – hill district council INGO – implementing NGO IP – indigenous people IPP – indigenous peoples plan LARF – land acquisition and resettlement framework LCS – labor contracting society LGED – Local Government Engineering Department MAD – micro agribusiness development MIS – management information system MOCHTA – Ministry of Chittagong Hill Tracts Affairs NOTE (i) In this report, "$" refers to US dollars. This indigenous peoples plan is a document of the borrower. The views expressed herein do not necessarily represent those of ADB's Board of Directors, Management, or staff, and may be preliminary in nature. In preparing any country program or strategy, financing any project, or by making any designation of or reference to a particular territory or geographic area in this document, the Asian Development Bank does not intend to make any judgments as to the legal or other status of any territory or area. 1 CONTENTS Page A. Executive Summary 3 B. -
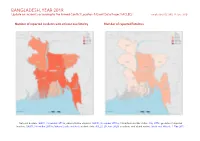
Bangladesh, Year 2019: Update on Incidents According to the Armed Conflict Location & Event Data Project (ACLED)
BANGLADESH, YEAR 2019: Update on incidents according to the Armed Conflict Location & Event Data Project (ACLED) compiled by ACCORD, 29 June 2020 Number of reported incidents with at least one fatality Number of reported fatalities National borders: GADM, November 2015b; administrative divisions: GADM, November 2015a; China/India border status: CIA, 2006; geodata of disputed borders: GADM, November 2015b; Natural Earth, undated; incident data: ACLED, 20 June 2020; coastlines and inland waters: Smith and Wessel, 1 May 2015 BANGLADESH, YEAR 2019: UPDATE ON INCIDENTS ACCORDING TO THE ARMED CONFLICT LOCATION & EVENT DATA PROJECT (ACLED) COMPILED BY ACCORD, 29 JUNE 2020 Contents Conflict incidents by category Number of Number of reported fatalities 1 Number of Number of Category incidents with at incidents fatalities Number of reported incidents with at least one fatality 1 least one fatality Protests 930 1 1 Conflict incidents by category 2 Riots 405 107 122 Development of conflict incidents from 2010 to 2019 2 Violence against civilians 257 184 195 Battles 99 43 63 Methodology 3 Strategic developments 15 0 0 Conflict incidents per province 4 Explosions / Remote 7 2 2 violence Localization of conflict incidents 4 Total 1713 337 383 Disclaimer 6 This table is based on data from ACLED (datasets used: ACLED, 20 June 2020). Development of conflict incidents from 2010 to 2019 This graph is based on data from ACLED (datasets used: ACLED, 20 June 2020). 2 BANGLADESH, YEAR 2019: UPDATE ON INCIDENTS ACCORDING TO THE ARMED CONFLICT LOCATION & EVENT DATA PROJECT (ACLED) COMPILED BY ACCORD, 29 JUNE 2020 Methodology GADM. Incidents that could not be located are ignored. -

Bandarban-S.Pdf
92°5'0"E 92°10'0"E 92°15'0"E 92°20'0"E 92°25'0"E UPAZILA MAP UPAZILA BANDARBAN SADAR DISTRICT BANDARBAN z# UPAZILA RAJASTHALI Rajbila z# DISTRICT RANGAMATI N " 0 z#T$ ' 0 N $T $ z# 2 " T ° 0 2 ' 2 0 2 ° 2 2 UPAZILA RANGUNIA Jhonka Islamp$Tur Bazar DISTRICT CHATTOGRAM z# z# z# z# z# z# z# z# z# z# z# Ñ z# Ñ N " 0 UPAZILA CHANDANAISH z#Chemi Dolupara Bazar ' $TT$ 5 1 N " z# ° 0 2 ' DISTRICT CHATTOGRAM z# Ghungru Bazar 2 5 1 $T ° 2 z# 2 z# z# Bagmz#ara Bazar z# S# L E G E N D Kuhz#a$Tlongz# Administrative Boundary z# z# } } } International Boundary Balaghata Bazar(M.A) Goaliakhola Bazar $T $T z# z# Division Boundary z# BANDARBAN z# T$ Ñ District Boundary z# z# z# z# Marma Baza$Tr(Mz#.A) Upazila Boundary z#[% T$ z# z# cz#$Tz#þ z#{# $T z# Union Boundary Bandarban Bazarz#(M.A) x% z# z# z#Kaz#lagata Bazar(M.A) Municipal Boundary z# z# z# z# N Administrative Headquarters z# " 0 ' z# 0 1 N " [% District ° 0 2 ' T$ BANDARBAN SADAR 2 0 z# 1 Upazila T$ ° Y# 2 S#Y# 2 $T Union Raicha Bazar z# UPAZILA ROWANGCHHARI Suaz#lock Physical Infrastructures $TMajer Para Bazar $Tz# |# National Highways S# Suwalok Bazar z# Regional Highways z# z# Zila Road VagT$gokul Bazar Upazila Road (Pucca) z#$T Upazila Road (Katcha) UPAZILA SATK ANIA z# Ñ DISTRICT CHATTOGRAM Union Road (Pucca) z# Union Road (Katcha) Village Road A (Pucca) z# z# N " 0 ' Village Road A (Katcha) 5 ° N " 2 0 2 ' 5 Village Road B (Pucca) ° 2 2 Village Road B (Katcha) z# Railway Network Embankment Chimbuk 16 Mile Baz$Tar Natural Features z# Wide River with Sandy Area z# Small River/ Khal Water Bodies -

Performance of Sweet Pepper Under Protective
INTERNATIONAL JOURNAL OF ENVIRONMENT Volume-3, Issue-1, Dec-Feb 2013/14 ISSN 2091-2854 Received:17 January Revised:11February Accepted:17Feburary INVENTORY OF THREATENED PLANTS OF BANGLADESH AND THEIR CONSERVATION MANAGEMENT M. Harun-ur-Rashid, M. Enamur Rashid and M. Atiqur Rahman* Department of Botany, University of Chittagong Chittagong 4331, Bangladesh *Corresponding author: [email protected] Abstract The study aimed at inventorying of threatened plant species of Bangladesh to determine their status of occurrence for emphasizing the setting-up of national conservation strategies and sustainable management. Complete inventory of two families, the Apocynaceae and Vitaceae, has been made and recognized 28 threatened species facing environmental threats, and need sustainable conservation management. The study was based on long-term field investigation, survey of relevant floristic literature and examination of herbarium specimens. An enumeration of threatened taxa is prepared with updated field data on conservation status to include into Red Data Book of Bangladesh. Key words: Inventory, threatened plant species, conservation, management, Bangladesh. Introduction Global biodiversity is depleting at an alarming rate due to human interferences and environmental degradation, causing high risk of extinction. Human impact on nature has reached at such a high proportion that the world is today witnessing an unprecedented rate of species loss. Many more species are disappearing from the nature before their discovery and determination. The 1997 IUCN Red List of Threatened Plants revealed that 12.5% or c.34,000 of the world’s vascular plant species are at risk of extinction, including 7% of family International Journal of Environment ISSN 2091-2854 141 | P a g e Apocynaceae and 5% of Vitaceae (Walter & Gillett, 1998). -

Bangladesh – BGD34387 – Lalpur – Sonapur – Noakhali – Dhaka – Christians – Catholics – Awami League – BNP
Refugee Review Tribunal AUSTRALIA RRT RESEARCH RESPONSE Research Response Number: BGD34387 Country: Bangladesh Date: 25 February 2009 Keywords: Bangladesh – BGD34387 – Lalpur – Sonapur – Noakhali – Dhaka – Christians – Catholics – Awami League – BNP This response was prepared by the Research & Information Services Section of the Refugee Review Tribunal (RRT) after researching publicly accessible information currently available to the RRT within time constraints. This response is not, and does not purport to be, conclusive as to the merit of any particular claim to refugee status or asylum. This research response may not, under any circumstance, be cited in a decision or any other document. Anyone wishing to use this information may only cite the primary source material contained herein. Questions 1. Please update on the situation for Catholics in Dhaka. 2. Are there any reports to suggest that Christians (or Catholics) tend to support or be associated with the BNP or AL generally, or whether this might depend on local conditions? 3. Are there any reports of a Catholic community in Lalpur (village) or Sonapur (local area) of Noakhali; in particular, their size and whether they are long-established? 4. If so, is there any material to indicate their mistreatment or serious incidents? 5. Please update on the treatment of BNP ‘field workers’ or supporters following the election of the AL Government. Any specific references to Dhaka or Noakhali would be useful. RESPONSE 1. Please update on the situation for Catholics in Dhaka. Question 2 of recent RRT Research Response BGD34378 of 17 February 2009 refers to source information on the situation of Catholics in Dhaka. -
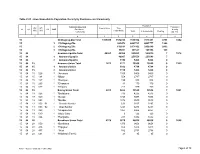
Chittagong C01.Pdf
Table C-01 : Area, Households, Population, Density by Residence and Community Population Administrative Unit Population UN / MZ / Area in Acres Total ZL UZ Vill RMO Residence density WA MH Households Community Total In Households Floating [sq. km] 1 2 3 4 5 6 7 8 15 Chittagong Zila Total 1305438 1532014 7616352 7611401 4951 1442 15 1 Chittagong Zila 863472 4463723 4461777 1946 15 2 Chittagong Zila 632691 2971102 2968240 2862 15 3 Chittagong Zila 35851 181527 181384 143 15 04 Anowara Upazila Total 40551 49966 259022 259015 7 1578 15 04 1 Anowara Upazila 48807 253556 253549 7 15 04 3 Anowara Upazila 1159 5466 5466 0 15 04 15 Anowara Union Total 1871 2171 10260 10260 0 1355 15 04 15 1 Anowara Union 1012 4794 4794 0 15 04 15 3 Anowara Union 1159 5466 5466 0 15 04 15 026 3 *Anowara 1159 5466 5466 0 15 04 15 134 1 *Bilpur 559 2747 2747 0 15 04 15 147 1 *Boalgaon 199 938 938 0 15 04 15 295 1 *Dhanpura 41 170 170 0 15 04 15 537 1 *Khilpara 213 939 939 0 15 04 19 Bairag Union Total 4013 5662 30545 30538 7 1881 15 04 19 026 1 *Badalpura 736 4235 4235 0 15 04 19 040 1 *Bairag 1740 9498 9498 0 15 04 19 053 1 *Bandar 1872 9530 9530 0 15 04 19 053 01 1 Dakshin Bandar 631 3297 3297 0 15 04 19 053 02 1 Uttar Bandar 1241 6233 6233 0 15 04 19 363 1 *Guapanchak 1067 6064 6057 7 15 04 19 510 1 *Majer Char 6 126 126 0 15 04 19 806 1 *Rangadia 241 1092 1092 0 15 04 28 Barakhain Union Total 4378 5679 28836 28836 0 1628 15 04 28 050 1 *Barakhain 1970 9658 9658 0 15 04 28 416 1 *Hajigaon 652 3478 3478 0 15 04 28 457 1 *Jhiyri 582 2798 2798 0 15 04 28 631 1 *Naidandi (Part-Ii) 21 95 95 0 RMO: 1 = Rural, 2 = Urban and 3 = Other Urban Page 1 of 79 Table C-01 : Area, Households, Population, Density by Residence and Community Population Administrative Unit Population UN / MZ / Area in Acres Total ZL UZ Vill RMO Residence density WA MH Households Community Total In Households Floating [sq. -

Nzfðs¡A¿»£ H¡Wm¡Cn Pll¡L
Government of the People’s Republic of Bangladesh Bangladesh Meteorological Department (Agro-meteorology Division) Meteorological Complex, Agargaon, Dhaka-1207. Agm-3 (2)/2013/41 Issue date: 02-11-2014 Forecast for the period: 02.11.2014 to 08.11.2014 Spatial distribution of Rainfall Accumulative Rainfall forecast Extended Outlook for accumulative rainfall (Period: 22-10-2014 to 31-10-2014) (Period: 02-11-2014 to 08-11-2014) (Period: 09-11-2014 to 15-11-2014) 27 26 Rangpur Dinajpur 0 0 8 25 Bogra Sylhet 7 Mymensingh 1 0 6 Rajshahi Trace Tangail Srimongal Ishurdi Trace 5 4 1 24 8 Dhaka Chuadanga Faridpur 4 1 Comilla 3 1 Chandpur Jessore Madaripur 3 4 Feni 3 M.Court 23 1 Khulna 1 Satkhira BarisalBhola 7 2 Sitakunda 3Sandwip Rangamati 1 1 2 Hatiya Patuakhali2 1 ChittagongTrace 2 2 0 Khepupara1 5 22 Kutubdia 0 0 Coxs_Bazar4 -1 1 21 Teknaf 0 88 89 90 91 92 93 Highlights: Country average of bright sunshine hour was 6.56 hours per day during the last week. Country average of free water loss during the previous week was averaged 3.20 mm per day. Weather forecast and Advisory for the period of 02.11.2014 to 08.11.2014. Bright sunshine hour is expected to be between 6.0 to 7.0 hours per day during this week. Average of free water loss during the next week is expected to be between 3.00 mm to 3.50 mm per day. • Seasonal low lies over South Bay. • Weather may remain mainly dry southern part of the country during the first half of this period. -

Accord Final Report
The Bangladesh Accord Foundation has provided the information on this signatory supplier list as of 7th October 2013 “as is” without any representations or warranties, express or implied. Approximate Approximate Total number of Factories: Total number of 1557 workers: 2,025,897 Number of Number of separate Floors of the Number of Factory housing Factory housing workers Phone City Phone buildings Number of stories of each building which Active Account ID Factory Name Address District Division Postal Code Phone in multi‐purpose in multi‐factory employed by Code Extension belonging to building the factory Members in building building factory (all production occupies Factory buildings) facility 9758 4 Knitwear Ltd Pathantuli,Godnail Narayanganj Dhaka 1400 2 7641780 No No 450 1 9965 4 You Clothing Ltd 367/1 Senpara parbota Mirpur Dhaka Dhaka Dhaka 1216 2 8020125 1/10; No No 2000 1 9552 4A YARN DYEING LTD. Kaichabari, Savar Dhaka Dhaka 2 79111568 3 1/5; 2/1; 3/1; No No 1250 3 10650 4S Park Style Ltd Durgapur, Ashulia, Savar. Dhaka Dhaka Dhaka 1341 2 9016954 1 6 no No 1/10 1200 1 10562 A Class Composite Ltd. East Isdair, Beside LGED Office, Fatullah, Narayanganj Dhaka 2 7642798 No No 1 Narayanganj 10086 A J Super Garments Ltd. Goshbag, Post‐ Zirabo, Thana ‐ Savar Dhaka Dhaka 1341 2 7702200 1 1/6; No No 2700 1 10905 A Plus Ind.Ltd. Plot‐28, Milk Vita Rd., Section‐07, Mirpur, Dhaka Dhaka Dhaka 1216 2 9338091 1 1/6; No Yes 1/0,3,4,5; 2200 1 10840 A&A Trousers Ltd Haribari Tak, Pubail Collage Gate, Pubail, Gazipur Dhaka 2 224255 1 1/5; Yes Yes 1/5‐2/5; 1200 1 Gazipur, Sadar, Gazipur 9229 A&B Outerwear Ltd Plot #29‐32, Sector # 4, CEPZ, Chittagong.