Electroconvulsive Therapy Her Health
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Delirium & Delirious Mania
Delirium & Delirious Mania; Differential Diagnosis. Delirium & Delirious Mania; Differential Diagnosis. Author: Eline Janszen. (s894226) Thesis-Supervisor: Ruth Mark Bachelorthesis Clinical Health Psychology Department of Neuropsychology, University of Tilburg September, 2011. 1 Delirium & Delirious Mania; Differential Diagnosis. ABSTRACT In the last few years, delirium in hospitals and in the elderly population has become an important subject of various studies, resulting in the recognition of several subtypes; hyperactive delirium, hypoactive delirium and mixed delirium. The first one of these subtypes, hyperactive delirium, shows a lot of overlap with another syndrome: Delirious mania. The current literature review examines both syndromes, discussing the overlap and the differences of their symptoms, while also looking at the neurological structures involved. Search engines including Sciencedirect, PSYCHinfo and medline were used to find the relevant literature. The data found in this examination reveals that, in spite of the several overlapping symptoms, delirious mania and hyperactive delirium are different syndromes; hyperactive delirium is associated with symptoms like hyperactivity, circardian rhythm disturbances and neurological abnormalities that include lesions of the hippocampus and dysfunction of the orbitofrontal cortex while delirious mania shows distinctive symptoms like pouring water and denudativeness (disrobing) with neurological abnormalities that also include orbitofrontal cortex dysfunction, but suffer mostly from an overall frontal circuitry dysfunction. This distinction is important for clinical outcome, seeing as that hyperactive delirium is treated with haloperidol and the preferred treatment for delirious mania is ECT. Keywords: delirium, hyperactive delirium, delirious mania. 2 Delirium & Delirious Mania; Differential Diagnosis. INTRODUCTION In recent years there has been a lot of research focused on diagnosing delirium. Since patients with delirium display fluctuating symptoms, the distinction from other conditions can be difficult. -
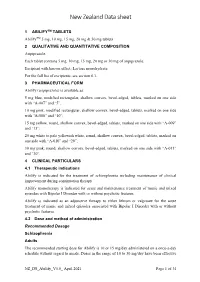
New Zealand Data Sheet
New Zealand Data sheet 1 ABILIFYTM TABLETS AbilifyTM 5 mg, 10 mg, 15 mg, 20 mg & 30 mg tablets 2 QUALITATIVE AND QUANTITATIVE COMPOSITION Aripiprazole. Each tablet contains 5 mg, 10 mg, 15 mg, 20 mg or 30 mg of aripiprazole. Excipient with known effect: Lactose monohydrate For the full list of excipients, see section 6.1. 3 PHARMACEUTICAL FORM Abilify (aripiprazole) is available as: 5 mg blue, modified rectangular, shallow convex, bevel-edged, tablets, marked on one side with “A-007” and “5”; 10 mg pink, modified rectangular, shallow convex, bevel-edged, tablets, marked on one side with “A-008” and “10”; 15 mg yellow, round, shallow convex, bevel-edged, tablets, marked on one side with “A-009” and “15”; 20 mg white to pale yellowish white, round, shallow convex, bevel-edged, tablets, marked on one side with “A-010” and “20”; 30 mg pink, round, shallow convex, bevel-edged, tablets, marked on one side with “A-011” and “30”. 4 CLINICAL PARTICULARS 4.1 Therapeutic indications Abilify is indicated for the treatment of schizophrenia including maintenance of clinical improvement during continuation therapy. Abilify monotherapy is indicated for acute and maintenance treatment of manic and mixed episodes with Bipolar I Disorder with or without psychotic features. Abilify is indicated as an adjunctive therapy to either lithium or valproate for the acute treatment of manic and mixed episodes associated with Bipolar I Disorder with or without psychotic features. 4.2 Dose and method of administration Recommended Dosage Schizophrenia Adults The recommended starting dose for Abilify is 10 or 15 mg/day administered on a once-a-day schedule without regard to meals. -
A Dictionary of Neurological Signs
FM.qxd 9/28/05 11:10 PM Page i A DICTIONARY OF NEUROLOGICAL SIGNS SECOND EDITION FM.qxd 9/28/05 11:10 PM Page iii A DICTIONARY OF NEUROLOGICAL SIGNS SECOND EDITION A.J. LARNER MA, MD, MRCP(UK), DHMSA Consultant Neurologist Walton Centre for Neurology and Neurosurgery, Liverpool Honorary Lecturer in Neuroscience, University of Liverpool Society of Apothecaries’ Honorary Lecturer in the History of Medicine, University of Liverpool Liverpool, U.K. FM.qxd 9/28/05 11:10 PM Page iv A.J. Larner, MA, MD, MRCP(UK), DHMSA Walton Centre for Neurology and Neurosurgery Liverpool, UK Library of Congress Control Number: 2005927413 ISBN-10: 0-387-26214-8 ISBN-13: 978-0387-26214-7 Printed on acid-free paper. © 2006, 2001 Springer Science+Business Media, Inc. All rights reserved. This work may not be translated or copied in whole or in part without the written permission of the publisher (Springer Science+Business Media, Inc., 233 Spring Street, New York, NY 10013, USA), except for brief excerpts in connection with reviews or scholarly analysis. Use in connection with any form of information storage and retrieval, electronic adaptation, computer software, or by similar or dis- similar methodology now known or hereafter developed is forbidden. The use in this publication of trade names, trademarks, service marks, and similar terms, even if they are not identified as such, is not to be taken as an expression of opinion as to whether or not they are subject to propri- etary rights. While the advice and information in this book are believed to be true and accurate at the date of going to press, neither the authors nor the editors nor the publisher can accept any legal responsibility for any errors or omis- sions that may be made. -
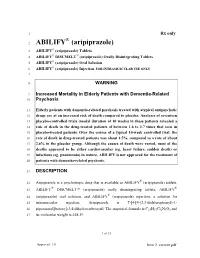
ABILIFY (Aripiprazole)
1 Rx only ® 2 ABILIFY (aripiprazole) 3 ABILIFY® (aripiprazole) Tablets 4 ABILIFY® DISCMELT™ (aripiprazole) Orally Disintegrating Tablets 5 ABILIFY® (aripiprazole) Oral Solution ® 6 ABILIFY (aripiprazole) Injection FOR INTRAMUSCULAR USE ONLY 7 8 WARNING 9 Increased Mortality in Elderly Patients with Dementia-Related 10 Psychosis 11 Elderly patients with dementia-related psychosis treated with atypical antipsychotic 12 drugs are at an increased risk of death compared to placebo. Analyses of seventeen 13 placebo-controlled trials (modal duration of 10 weeks) in these patients revealed a 14 risk of death in the drug-treated patients of between 1.6 to 1.7 times that seen in 15 placebo-treated patients. Over the course of a typical 10-week controlled trial, the 16 rate of death in drug-treated patients was about 4.5%, compared to a rate of about 17 2.6% in the placebo group. Although the causes of death were varied, most of the 18 deaths appeared to be either cardiovascular (eg, heart failure, sudden death) or 19 infectious (eg, pneumonia) in nature. ABILIFY is not approved for the treatment of 20 patients with dementia-related psychosis. 21 DESCRIPTION ® 22 Aripiprazole is a psychotropic drug that is available as ABILIFY (aripiprazole) tablets, ® ® 23 ABILIFY DISCMELT™ (aripiprazole) orally disintegrating tablets, ABILIFY ® 24 (aripiprazole) oral solution, and ABILIFY (aripiprazole) injection, a solution for 25 intramuscular injection. Aripiprazole is 7-[4-[4-(2,3-dichlorophenyl)-1- 26 piperazinyl]butoxy]-3,4-dihydrocarbostyril. The empirical formula is C23H27Cl2N3O2 and 27 its molecular weight is 448.39. 1 of 53 Approved 1.0 Item 2 current.pdf 28 The chemical structure is: Cl Cl N N CH2CH2CH2CH2O N O H 29 30 ABILIFY tablets are available in 2-mg, 5-mg, 10-mg, 15-mg, 20-mg, and 30-mg 31 strengths. -
SPEECH DISORDERS Amr Hassan, MD,FEBN Associate Professor of Neurology Cairo University
NOTE: To change the image on this slide, select the picture and delete it. Then click the Pictures icon in the placeholde r to insert your own image. SPEECH DISORDERS Amr Hassan, MD,FEBN Associate professor of Neurology Cairo University Definition of Speech Speech is the communication of meanings by means of symbols, which usually take the form of spoken or written words. Mechanisms of Speech : 1. Central Mechanisms: Depending on the integration of the higher brain centers for symbolization (speech centers), mainly in the dominant hemisphere. Lesion leads to Dysphasia or Aphasia. 2. Peripheral Mechanisms: A. Articulation: Lesion leads to Dysarthria or Anarthria. B. Phonation: Lesion leads to Dysphonia or Aphonia. Aphonia . Phonation is lost but articulation is preserved . The patient talks in whisper Types and Causes: A. Hysterical (can phonate when coughing) B. Organic 1. Bilateral paralysis of the vocal cords 2. Diseases of larynx 3. Paresis of respiratory movements 4. Spastic dysphonia 5. Glottis spasm Dysarthria Dysarthria=Disorder of articulation Types and Causes: 1. LMN Dysarthria 2. UMN (spastic) Dysarthria 3. Extra-pyramidal Dysarthria a. Rigid dysarthria: Parkinsonism b. Hiccup speech: Chorea and myoclonus 4. Cerebellar Dysarthria a. Syllabic (or scanning) b. Explosive c. Stacatto Mechanisms of Speech : 1. Central Mechanisms: Depending on the integration of the higher brain centers for symbolization (speech centers), mainly in the dominant hemisphere. Lesion leads to Dysphasia or Aphasia. 2. Peripheral Mechanisms: A. Articulation: Lesion leads to Dysarthria or Anarthria. B. Phonation: Lesion leads to Dysphonia or Aphonia. Speech Centers I. Sensory Centers: A. Visual Centers: Area 17 for visual reception. -
Late Modernist Schizophrenia: from Phenomenology to Cultural Pathology
LATE MODERNIST SCHIZOPHRENIA: FROM PHENOMENOLOGY TO CULTURAL PATHOLOGY A Dissertation Submitted to the Temple University Graduate Board In Partial Fulfillment of the Requirements for the Degree DOCTOR OF PHILOSOPHY by Jonathan Gagas May 2014 Examining Committee Members: Daniel T. O'Hara, Advisory Chair, Department of English Sheldon Brivic, Department of English Alan Singer, Department of English Robert L. Caserio, External Member, The Pennsylvania State University, Department of English © Copyright 2014 by Jonathan Gagas All Rights Reserved ii ABSTRACT My dissertation explains the problematic nature of using the diagnostic category schizophrenia as a cultural metaphor, whether the disorder is stigmatized or romanticized, and demonstrates how representations of schizophrenic characters in novels can combat widespread misuses of psychiatric terms and help readers empathize with mentally ill people if we read these novels with some understanding of psychiatry and the psychoanalysis that influenced them. Public understanding of psychiatry and psychology has played an increasingly important role in mentally ill people’s prospects for recovery as inpatient care has given way to outpatient care supplemented by patients’ families and communities during the past half century. Many people with severe mental illnesses end up homeless or in prison not only because of cuts to services that help them work toward autonomy and social integration, but also because of how their communities treat them, from ignorance and misunderstanding of mental health issues to the stigma that often accompanies mental illness. Contemporary scholars and artists have much to learn about changing attitudes toward mental disorder through an examination of the schizophrenia concept’s migration from the mental health professions to fiction and cultural theory. -

Malignant Catatonia Due to Anti-NMDA-Receptor Encephalitis in a 17-Year-Old Girl
Consoli et al. Child and Adolescent Psychiatry and Mental Health 2011, 5:15 http://www.capmh.com/content/5/1/15 CASEREPORT Open Access Malignant catatonia due to anti-NMDA-receptor encephalitis in a 17-year-old girl: case report Angèle Consoli1, Karine Ronen1, Isabelle An-Gourfinkel2, Martine Barbeau1, Donata Marra3, Nathalie Costedoat-Chalumeau3, Delphine Montefiore5, Philippe Maksud4, Olivier Bonnot1, Adrien Didelot6, Zahir Amoura3, Marie Vidailhet2 and David Cohen1* Abstract Anti-NMDA-Receptor encephalitis is a severe form of encephalitis that was recently identified in the context of acute neuropsychiatric presentation. Here, we describe the case of a 17-year-old girl referred for an acute mania with psychotic features and a clinical picture deteriorated to a catatonic state. Positive diagnosis of anti-NMDA- receptor encephalitis suggested specific treatment. She improved after plasma exchange and immunosuppressive therapy. Post-cognitive sequelae (memory impairment) disappeared within 2-year follow-up and intensive cognitive rehabilitation. Keywords: Anti-NMDA-Receptor encephalitis, Adolescence, Malignant catatonia Background encephalitis over a 3-year period [4]. The exact incidence NMDA receptors are ligand-gated cation channels that of anti-NMDAR encephalitis is unknown, but it seems to play an important role in synaptic plasticity [1] and seem be more frequent than any other known paraneoplastic to be implicated in the physiopathology of neuropsychia- encephalitis [4]. It predominantly affects children and tric disorders [2]. NMDA receptors are heteromers of young adults and may occur with or without tumor asso- NR1 and NR2 subunits (A, B, C or D) that bind glycine ciation [4]. Eighty percent of the patients are women. -

A Double Dissociation Between Two Psychotic Phenotypes: Periodic Catatonia and Cataphasia
Prog Neuropsychopharmaco Biol Psych 2018 Aug 30;86:363-369 doi: 10.1016/j.pnpbp.2018.03.008 A Double Dissociation Between Two Psychotic Phenotypes: Periodic Catatonia and Cataphasia Foucher Jack René*,1,2, Zhang Yi Fan1, Roser Mathilde1,2, Lamy Julien1, De Sousa Paulo Loureiro1, Weibel Sébastien3,4, Vidailhet Pierre3,4, Mainberger Olivier1,2, Berna Fabrice3,4 1. ICube – CNRS UMR 7357, Neurophysiology, FMTS, University of Strasbourg, France. 2. CEMNIS – Noninvasive Neuromodulation Center, University Hospital Strasbourg, France. 3. Physiopathologie et Psychopathologie Cognitive de la Schizophrénie – INSERM 1114, FMTS, University of Strasbourg, France. 4. Pôle de Psychiatrie, Santé Mentale et Addictologie, University Hospital Strasbourg, France. Abstract: Schizophrenia as a single liability model was confronted to the multiple psychotic phenotypes model proposed by the Wernicke-Kleist-Leonhard school, focusing on two: periodic catatonia (PC) and cataphasia (C). Both are stable and heritable psychotic phenotypes with no crossed liability and are coming with the buildup of specific residual symptoms: impairment of psychomotricity for PC and a specific disorganization of thought and language in C. Regional cerebral blood flow (rCBF) was used as a biomarker. We attempted to refute the single phenotype model by looking at relevant and specific rCBF anomalies for PC and C, that would exceed anomalies in common relative to controls (CTR), i.e. looking for a double dissociation. Twenty subjects with PC, 9 subjects with C and 27 matched controls had two MRI QUIPSS-II arterial spin labeling sequences converted in rCBF. One SPM analysis was performed for each rCBF measurement and the results were given as the conjunction of both analysis. -

A Review of Automated Speech and Language Features for Assessment of Cognitive and Thought Disorders Rohit Voleti, Student Member, IEEE, Julie M
IEEE JOURNAL OF SELECTED TOPICS IN SIGNAL PROCESSING (JSTSP), SPECIAL ISSUE 1 A Review of Automated Speech and Language Features for Assessment of Cognitive and Thought Disorders Rohit Voleti, Student Member, IEEE, Julie M. Liss, Visar Berisha, Member, IEEE, Abstract—It is widely accepted that information derived from Initial analyzing speech (the acoustic signal) and language production Prompt (words and sentences) serves as a useful window into the health of an individual’s cognitive ability. In fact, most neuropsychological Record testing batteries have a component related to speech and language Subject where clinicians elicit speech from patients for subjective evalu- Response ation across a broad set of dimensions. With advances in speech signal processing and natural language processing, there has been ASR or Manual recent interest in developing tools to detect more subtle changes Transcription in cognitive-linguistic function. This work relies on extracting a set of features from recorded and transcribed speech for objective assessments of speech and language, early diagnosis of Natural Language Speech Signal neurological disease, and tracking of disease after diagnosis. With Processing Processing an emphasis on cognitive and thought disorders, in this paper Lexical Complexity Pause Rate we provide a review of existing speech and language features used in this domain, discuss their clinical application, and Syntactic Complexity Prosody & Rate highlight their advantages and disadvantages. Broadly speaking, the review is split into two categories: language features based on Semantic Coherence Articulation natural language processing and speech features based on speech signal processing. Within each category, we consider features Machine that aim to measure complementary dimensions of cognitive- Learning linguistics, including language diversity, syntactic complexity, Model semantic coherence, and timing. -

Edward Shorter's Comment on Jack R. Foucher Et Al.'S Wernicke-Kleist- Leonhard Phenotypes of Endogenous Psychoses: a Review
1 Edward Shorter’s comment on Jack R. Foucher et al.’s Wernicke-Kleist- Leonhard phenotypes of endogenous psychoses: a review of their validity Pfuhlman B, Gawlik M, Roth JN, de Billy CdeC, Jeanjean LC, Obrecht A, Mainberger O, Clauss JME, Elowe J, Weibel S, Schorr B, Cetkovich M, Morra C, Rebok F, Ban TA, Bollmann B, Roser MM, Hanke MS, Jabs BE, Franzek EJ, Berna F. and Foucher J’s reply Our first follow-up response to Edward Shorter’s comment on our recent review of Wernicke, Kleist and Leonhard (WKL) school (Foucher, Gawlik, Roth et al. 2020b) had to address the issue of IDC-DSM vs WKL concepts of catatonia as it is illustrative of the kind of misunderstandings that ensue the interpretation of the latter with the views of the former (and vice versa). “I was dismayed to see “periodic catatonia” described as another of the “non- system schizophrenias.” It has been with so much trouble that psychiatry has recently detached catatonia from schizophrenia and made it a disease of its own. Now, for the authors to reinsert catatonia in schizophrenia, and to claim that it is response to antipsychotics, is to weep. Antipsychotics are counter-indicated in catatonia; the remedies of choice are the benzodiazepines and convulsive therapy (Shorter and Fink 2018).” This example embeds some of the most profound dissimilarities between the two frameworks which if unclarified might let the DSM and the WKL communities talking past each other, somewhat in the sense of an incommensurability (Kuhn 1996). DSM-descriptive vs WKL-theoretical concepts Indeed, as both research programs were looking for categorical pathological entities, these were defined in completely different ways. -

Sociodemographic, Circumstantial, and Psychopathological Predictors of Involuntary Admission of Patients with Acute Psychosis
Article Sociodemographic, Circumstantial, and Psychopathological Predictors of Involuntary Admission of Patients with Acute Psychosis Johanna Seifert * , Christian Ihlefeld , Tristan Zindler , Christian K. Eberlein , Maximilian Deest, Stefan Bleich, Sermin Toto and Catharina Meissner Department of Psychiatry, Social Psychiatry and Psychotherapy, Hannover Medical School, 30625 Hannover, Germany; [email protected] (C.I.); [email protected] (T.Z.); [email protected] (C.K.E.); [email protected] (M.D.); [email protected] (S.B.); [email protected] (S.T.); [email protected] (C.M.) * Correspondence: [email protected] Abstract: Studies have consistently determined that patients with acute psychosis are more likely to be involuntarily admitted, although few studies examine specific risk factors of involuntary admission (IA) among this patient group. Data from all patients presenting in the psychiatric emergency department (PED) over a period of one year were extracted. Acute psychosis was identified using specific diagnostic criteria. Predictors of IA were determined using logistic regression analysis. Out of 2533 emergency consultations, 597 patients presented with symptoms of acute psychosis, of whom 118 were involuntarily admitted (19.8%). Involuntarily admitted patients were more likely to arrive via Citation: Seifert, J.; Ihlefeld, C.; police escort (odds ratio (OR) 10.94) or ambulance (OR 2.95), live in a psychiatric residency/nursing Zindler, T.; Eberlein, C.K.; Deest, M.; home (OR 2.76), report non-adherence to medication (OR 2.39), and were less likely to suffer from Bleich, S.; Toto, S.; Meissner, C. (comorbid) substance abuse (OR 0.53). -

Catatonia in Patients with Autism: Prevalence and Management
CNS Drugs (2014) 28:205–215 DOI 10.1007/s40263-014-0143-9 THERAPY IN PRACTICE Catatonia in Patients with Autism: Prevalence and Management Luigi Mazzone • Valentina Postorino • Giovanni Valeri • Stefano Vicari Published online: 7 February 2014 Ó Springer International Publishing Switzerland 2014 Abstract Although recent studies have shown that catato- occurring in the context of various medical and neuro- nia can occur in patients with autism spectrum disorders psychiatric conditions [1–3]. This syndrome, firstly (ASDs), the overlap of the behavioral features between these described by Kahlbaum as a separate disorder [4], was disorders raises many diagnostic challenges. In fact, in clin- subsequently incorporated by Kraepelin in the equation of ical practice it is common to misinterpret catatonic symp- ‘catatonia = schizophrenia’ leading to decades of mis- toms, including mutism, stereotypic speech, repetitive conception that all catatonic symptoms indicated schizo- behaviors, echolalia, posturing, mannerisms, purposeless phrenia [1]. Currently, prevalence estimates of catatonia in agitation and rigidity, as features of ASDs. The current psychiatric populations range from 0.6 % for adolescents, medical treatment algorithm for catatonia in ASDs recom- to between 6.9 % and 10 % for adult psychiatric inpatients mends the use of benzodiazepines. Electroconvulsive therapy [5–7]. In clinical practice it is common to misinterpret (ECT) is indicated when patients are unresponsive, or catatonic symptoms, such as mutism, stereotypic speech, insufficiently responsive, to benzodiazepines. Other phar- repetitive behaviors, echolalia, posturing, mannerisms, macological options are also described for the treatment of purposeless agitation and rigidity, as features of autism catatonic patients resistant to benzodiazepines and ECT, and spectrum disorders (ASDs) [5, 8, 9].