SAVE the CHILDREN NEPAL FIELD OFFICE Siraha District Child Survival 7 Midterm Evaluation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

1 Fao/Global Environment Facility Project Document
FAO/GLOBAL ENVIRONMENT FACILITY PROJECT DOCUMENT Project title: Reducing vulnerability and increasing adaptive capacity to respond to impacts of climate change and variability for sustainable livelihoods in agriculture sector in Nepal Project Symbol: GCP/NEP/071/LDF Recipient Country: Nepal Resource Partner: Global Environment Facility (GEF) FAO Project ID: 616181 GEF Project ID: 5111 Government/other counterparts: Ministry of Agricultural Development (MOAD), Department of Agriculture (DOA), Department of Livestock Services (DLS), Nepal Agricultural Research Council (NARC) and Department of Hydrology and Meteorology (DHM) Expected OED (Starting Date): January 2015 Expected NTE (End date): December 2018 Contribution to FAO’s Strategic objective/Organizational Result: SO2: Increase and improve Strategic Framework: provision of goods and services from agriculture, forestry and fisheries in a sustainable manner. Organizational Outcomes 1 (output 1.1 and 1.2) Country Programming Framework Outcome: 4.3 (CLIMATE CHANGE): Institutional and technical capacities for adaptation to climate change in agriculture strengthened and adaptive capacity of vulnerable communities enhanced. GEF Focal Area/LDCF/SCCF: Least Developed Country Fund GEF/LDCF/SCCF Strategic Objectives: CCA1: Reducing vulnerability – Reduce vulnerability to the adverse impacts of climate change, including variability, at local, national, regional and global level CCA2: Increasing Adaptive Capacity: Increase adaptive capacity to respond to the impacts of climate change, including variability, at local, national, regional and global level CCA3: Adaptation Technology Transfer: Promote transfer and adoption of adaptation technology Environment impact assessment Category: A B C √ Financing Plan: GEF/LDCF/SCCF allocation USD 2,689,498 Co-financing FAO/UTF USD 8,620,000 FAO/MTF USD 1,170,000 Government USD 3,200,000 Sub-total Co-Financing: USD 12,990,000 1 EXECUTIVE SUMMARY Nepal is one of the most vulnerable countries to climate change impacts. -

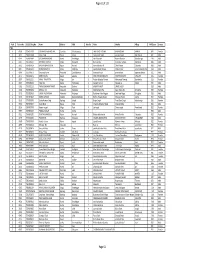
Code Under Name Girls Boys Total Girls Boys Total 010290001
P|D|LL|S G8 G10 Code Under Name Girls Boys Total Girls Boys Total 010290001 Maiwakhola Gaunpalika Patidanda Ma Vi 15 22 37 25 17 42 010360002 Meringden Gaunpalika Singha Devi Adharbhut Vidyalaya 8 2 10 0 0 0 010370001 Mikwakhola Gaunpalika Sanwa Ma V 27 26 53 50 19 69 010160009 Phaktanglung Rural Municipality Saraswati Chyaribook Ma V 28 10 38 33 22 55 010060001 Phungling Nagarpalika Siddhakali Ma V 11 14 25 23 8 31 010320004 Phungling Nagarpalika Bhanu Jana Ma V 88 77 165 120 130 250 010320012 Phungling Nagarpalika Birendra Ma V 19 18 37 18 30 48 010020003 Sidingba Gaunpalika Angepa Adharbhut Vidyalaya 5 6 11 0 0 0 030410009 Deumai Nagarpalika Janta Adharbhut Vidyalaya 19 13 32 0 0 0 030100003 Phakphokthum Gaunpalika Janaki Ma V 13 5 18 23 9 32 030230002 Phakphokthum Gaunpalika Singhadevi Adharbhut Vidyalaya 7 7 14 0 0 0 030230004 Phakphokthum Gaunpalika Jalpa Ma V 17 25 42 25 23 48 030330008 Phakphokthum Gaunpalika Khambang Ma V 5 4 9 1 2 3 030030001 Ilam Municipality Amar Secondary School 26 14 40 62 48 110 030030005 Ilam Municipality Barbote Basic School 9 9 18 0 0 0 030030011 Ilam Municipality Shree Saptamai Gurukul Sanskrit Vidyashram Secondary School 0 17 17 1 12 13 030130001 Ilam Municipality Purna Smarak Secondary School 16 15 31 22 20 42 030150001 Ilam Municipality Adarsha Secondary School 50 60 110 57 41 98 030460003 Ilam Municipality Bal Kanya Ma V 30 20 50 23 17 40 030460006 Ilam Municipality Maheshwor Adharbhut Vidyalaya 12 15 27 0 0 0 030070014 Mai Nagarpalika Kankai Ma V 50 44 94 99 67 166 030190004 Maijogmai Gaunpalika -

Contract for Consultant's Services
1-2 Province Government Province No.2 Ministry of Physical Infrastructure Development Janakpurdham REQUEST FOR PROPOSALS for Selection of Consulting Services for: Feasibility Study of Madheshi Sahid Marg (East-West Highway) RFP No.: MoPID/P2/FS/R/03/2077/078 Financing Agency: Province Government Package No.: Three Chainage: From 162+600 to 238+430 Km District: Sarlahi and Rautahat Road Section: Sarlahi and Rautahat Consultant's Name and address: May 2021 TABLE OF CONTENTS Section 1 – Letter of Invitation Section 2 – Instructions to Consultants and Data Sheet Section 3 – Technical Proposal – Standard Forms Section 4 – Financial Proposal – Standard Forms Section 5 – Eligible Countries Section 6 – Corrupt and Fraudulent Practices Section 7–Terms of Reference Section 8– Conditions of Contract and Contract Forms ii TABLE OF CLAUSES PART I Section 1. Letter of Invitation Section 2. Instructions to Consultants and Data Sheet A. General Provisions 1.Definitions 2.Introduction 3.Conflict of Interest 4.Unfair Competitive Advantage 5.Corrupt and Fraudulent Practices 6.Eligibility B. Preparation of Proposals 7.General Considerations 8.Cost of Preparation of Proposal 9.Language 10.Documents Comprising the Proposal 11.Only One Proposal 12.Proposal Validity 13.Clarification and Amendment of RFP 14.Preparation of Proposals – Specific Considerations 15.Technical Proposal Format and Content 16.Financial Proposal C. Submission, Opening and Evaluation 17.Submission, Sealing, and Marking of Proposals 18.Confidentiality 19.Opening of Technical Proposals 20.Proposals Evaluation 21.Evaluation of Technical Proposals 22.Financial Proposals for QBS 23.Public Opening of Financial Proposals (for QCBS, FBS, and LCS methods) 24.Correction of Errors 25.Taxes iii 1-iv 26.Conversion to Single Currency 27.Combined Quality and Cost Evaluation 28.Negotiations 29.Conclusion of Negotiations 30.Award of Contract D. -

Food Insecurity and Undernutrition in Nepal
SMALL AREA ESTIMATION OF FOOD INSECURITY AND UNDERNUTRITION IN NEPAL GOVERNMENT OF NEPAL National Planning Commission Secretariat Central Bureau of Statistics SMALL AREA ESTIMATION OF FOOD INSECURITY AND UNDERNUTRITION IN NEPAL GOVERNMENT OF NEPAL National Planning Commission Secretariat Central Bureau of Statistics Acknowledgements The completion of both this and the earlier feasibility report follows extensive consultation with the National Planning Commission, Central Bureau of Statistics (CBS), World Food Programme (WFP), UNICEF, World Bank, and New ERA, together with members of the Statistics and Evidence for Policy, Planning and Results (SEPPR) working group from the International Development Partners Group (IDPG) and made up of people from Asian Development Bank (ADB), Department for International Development (DFID), United Nations Development Programme (UNDP), UNICEF and United States Agency for International Development (USAID), WFP, and the World Bank. WFP, UNICEF and the World Bank commissioned this research. The statistical analysis has been undertaken by Professor Stephen Haslett, Systemetrics Research Associates and Institute of Fundamental Sciences, Massey University, New Zealand and Associate Prof Geoffrey Jones, Dr. Maris Isidro and Alison Sefton of the Institute of Fundamental Sciences - Statistics, Massey University, New Zealand. We gratefully acknowledge the considerable assistance provided at all stages by the Central Bureau of Statistics. Special thanks to Bikash Bista, Rudra Suwal, Dilli Raj Joshi, Devendra Karanjit, Bed Dhakal, Lok Khatri and Pushpa Raj Paudel. See Appendix E for the full list of people consulted. First published: December 2014 Design and processed by: Print Communication, 4241355 ISBN: 978-9937-3000-976 Suggested citation: Haslett, S., Jones, G., Isidro, M., and Sefton, A. (2014) Small Area Estimation of Food Insecurity and Undernutrition in Nepal, Central Bureau of Statistics, National Planning Commissions Secretariat, World Food Programme, UNICEF and World Bank, Kathmandu, Nepal, December 2014. -

Of Hetauda-Dhalkebar-Duhabi 400 Kv TL
Updated Resettlement Action Plan (RAP) of Hetauda-Dhalkebar-Duhabi 400 kV TL Submitted To: Nepal India Electricity Transmission and Trade Project Hetauda-Dhalkebar-Duhabi 400 kV Transmission Line Nepal Electricity Authority Kharipati, Bhaktapur Prepared And Submitted By: Environment and Social Studies Department Engineering Services Directorate Nepal Electricity Authority Kharipati, Bhaktapur May, 2017 Updated Resettlemention Action Plan i ABBREVIATIONS CBO Community Based Organization CDO Chief District Officer CDC Compensation Determination Committee CFUG Community Forest User Group DADO District Agriculture Development Office DDC District Development Committee DFO District Forest Office DHO District Health Office EIA Environmental Impact Assessment EMF Electromagnetic Fields ESMF Environmental and Social Management Framework ESSD Environment and Social Studies Department FGD Focus Group Discussion GON Government of Nepal HEP Hydro Electric Project HH Household HDD-ESMU Hetauda-Dhalkebar-Duhabi Environnent & Social Mgmt. Unit INPS Integrated Nepal Power System IPP Independent Power Producers IRPA International Radiation Protection Association KIIs Key Informant Interviews km Kilometer kV Kilovolt LCF Local Consultative Forum LDO Local Development Officer LARU Land Acquisition and Rehabilitation Unit NEA Nepal Electricity Authority NRs. Nepalese Rupees NGO Non Governmental Organization PAF Project Affected Family PAP Project Affected Person PCU Program Coordination Unit PRA Participatory Rapid Appraisal RAP Resettlement Action Plan ROW -

Resettlement Action Plan (RAP) of Hetauda-Dhalkebar-Duhabi 400 Kv and Dhalkebar-Bhittamod 400 Kv TL Project
Resettlement Action Plan (RAP) of Hetauda-Dhalkebar-Duhabi 400 Public Disclosure Authorized kV And Dhalkebar-Bhittamod 400 kV TL Project (Angle Tower, Sub-stations and Structures) Public Disclosure Authorized Prepared And Submitted By: Public Disclosure Authorized Environment And Social Studies Department Engineering Services Nepal Electricity Authority Kharipati, Bhaktapur February, 2011 Public Disclosure Authorized Resettlemention Action Plan ABBREVIATIONS CBO Community Based Organization CDO Chief District Officer CDC Compensation Determination Committee CFUG Community Forest User Group DADO District Agriculture Development Office DDC District Development Committee DFO District Forest Office DHO District Health Office EIA Environmental Impact Assessment EMF Electromagnetic Fields ESMF Environmental and Social Management Framework ESSD Environment and Social Studies Department FGD Focus Group Discussion GON Government of Nepal HEP Hydro Electric Project HH Household HDD~ESMU Hetauda-D.halkebar-Duhabi Environnent & Social Mgmt. Unit INPS Integrated Nepal Power System IPP Independent Power Producers IRPA International Radiation Protection Association KlIs Key Informant Interviews km Kilometer kV Kilovolt LCF Local Consultative Forum LDO Local Development Officer LARU Land Acquisition and Rehabilitation Unit NEA Nepal Electricity Authority NRs. Nepalese Rupees NGO Non Governmental Organization PAF Project Affected Family PAP Project Affected Person PCU Program Coordination Unit PRA Participatory Rapid Appraisal RAP Resettlement Action -

ZSL National Red List of Nepal's Birds Volume 5
The Status of Nepal's Birds: The National Red List Series Volume 5 Published by: The Zoological Society of London, Regent’s Park, London, NW1 4RY, UK Copyright: ©Zoological Society of London and Contributors 2016. All Rights reserved. The use and reproduction of any part of this publication is welcomed for non-commercial purposes only, provided that the source is acknowledged. ISBN: 978-0-900881-75-6 Citation: Inskipp C., Baral H. S., Phuyal S., Bhatt T. R., Khatiwada M., Inskipp, T, Khatiwada A., Gurung S., Singh P. B., Murray L., Poudyal L. and Amin R. (2016) The status of Nepal's Birds: The national red list series. Zoological Society of London, UK. Keywords: Nepal, biodiversity, threatened species, conservation, birds, Red List. Front Cover Back Cover Otus bakkamoena Aceros nipalensis A pair of Collared Scops Owls; owls are A pair of Rufous-necked Hornbills; species highly threatened especially by persecution Hodgson first described for science Raj Man Singh / Brian Hodgson and sadly now extinct in Nepal. Raj Man Singh / Brian Hodgson The designation of geographical entities in this book, and the presentation of the material, do not imply the expression of any opinion whatsoever on the part of participating organizations concerning the legal status of any country, territory, or area, or of its authorities, or concerning the delimitation of its frontiers or boundaries. The views expressed in this publication do not necessarily reflect those of any participating organizations. Notes on front and back cover design: The watercolours reproduced on the covers and within this book are taken from the notebooks of Brian Houghton Hodgson (1800-1894). -
Environmental Assessment Document Initial Environmental Examination
Environmental Assessment Document Initial Environmental Examination Loan Number: 2102 NEP August 2009 Nepal: Community-Managed Irrigated Agricultural Sector Project Mainawati Irrigation Sub-Project, Siraha Prepared by the Government of Nepal The Environmental Assessment is a document of the borrower. The views expressed herein do not necessarily represent those of ADB’s Board of Directors, Management, or staff, and may be preliminary in nature. Appendix J : Initial Environmental Examination (IEE) INITIAL ENVIRONMENTAL EXAMINATION MAINAWATI IRRIGATION SUB-PROJECT, SIRAHA DISTRICT I. EXECUTIVE SUMMARY 1. This initial environmental examination (IEE) was undertaken for the Mainawati Irrigation Subproject under Community Managed Irrigated Agriculture Sector Project under ADB Loan 2102 NEP to meet the Asian Development Bank’s (ADB) requirements for environmental assessment process and documentation prior to Subproject approval, following the procedures in ADB’s Environmental Assessment Guidelines (2003), and the Project’s Environmental Assessment and Review Procedures. 2. The subproject does not pass through any environmentally sensitive ecological area. It is the rehabilitation of the existing irrigation scheme where the system is already in operation since many years. Apart from some construction related impacts, the subproject will have minimal impact on the environment. Hence the subproject has been categorized under Category B as per the Environment Assessment Policy, 2002. 3. This Initial Environmental Examination (IEE) was based on data collected during the Joint Walkthrough Survey. The objective of the IEE is to analyze the adverse environmental impacts arising from site selection, design, construction and operation of the subproject. The mitigation of any such effect to acceptable levels was sought through implementation of a set of clearly defined and costed mitigation measures which have been included in the cost estimates. -
Natural Resource, Market Demand and Target Group Analysis of Siraha District-Development Management Institute
Published by: Micro-Enterprise Development Programme Ministry of Industry United Nations Development Programme June 2013 Copyright © 2013 Micro-Enterprise Development Programme (MEDEP)/UNDP All rights are reserved. No part of this edited volume may be reproduced by any means, nor transmitted, nor translated into a machine language without the written permission of the publisher. ISBN: 978-99946-916-6-1 Printed in Nepal at : Office Support Service Centre Chhapakhana P. Ltd. Teku, Kathmandu Tel.: 4240571 Email.: [email protected] Natural Resource, Market Demand and Target Group Analysis of Siraha District1 Abstract MEDEP was piloted in 1998. It expanded to 36 districts by 2010 in its third phase (2008-13). The development objective of the programme was to contribute to reduce poverty among low-income families in rural areas, and to ensure the institutional development and capacity building of local service delivery organizations to work as catalysts in the development of rural micro-enterprise sector. In order to reach its target group, MEDEP conducts natural resource, market demand and target group surveys in the new programme districts. As Siraha was added as a new programme district in the third phase, this study was conducted to furnish these information. On the basis of the major findings, this study concluded that Siraha district has a high potential of developing micro- enterprises to create employment and income-generating opportunities for the MEDEP's target groups. For implementation effectiveness and better results, MEDEP should concentrate its programme on 32 new VDCs clustered around six market centres. Entrepreneurs should be supported in marketing skill development, market survey and marketing. -

School Governance and Accountability Situation: A
HAMRO SHIKSHYA PROJECT School Governance and Accountability Situation: A Comprehensive Assessment of Dhanusha, Mahottari and Siraha Districts Final Report NATIONAL CAMPAIGN FOR EDUCATION NEPAL December, 2016 Research Team Dr. Megh Raj Dangal (Team Leader) Mr. Rebat Kumar Dhakal (Research Coordinator) Mr. Kul Prasad Khanal (Researcher) Ms. Rupa Munakarmi (Researcher) Acknowledgements This study has been possible with the support and contribution of a large number of people. The study team gratefully acknowledges the support and help of all those who contributed to the study. We would like to express our special gratitude and thanks to National Campaign for Education Nepal (NCE-Nepal), Search for Common Ground and GoGo Foundation for their trust in us and for the opportunity given to us in conducting and reporting this study. Particularly, we are grateful to Dr. Bhola Prasad Dahal and Mr. Ram Gaire for providing us with necessary guidelines and support during the entire period of this research. Our thanks and appreciations also go to Mr. Salikram Kalathoki and Ms. Reeza Shrestha who helped in reaching the field and meeting with the local project staffs, who in turn, supported us in accessing the gatekeepers and participants as well as providing us with timely support. Further, we would like to thank the entire team of GoGo Foundation. We heartily acknowledge Mr. Alok Thakur's, regional representative from Search for Common Ground, help in providing us with all the important information and documents during consultation meetings and interviews. The District Education Officials in Dhanusha, Mahottari and Siraha also deserve our sincere thanks. Finally, we thank all the participants for their active participation and sharing useful information with us. -
TSLC PMT Result
Page 62 of 132 Rank Token No SLC/SEE Reg No Name District Palika WardNo Father Mother Village PMTScore Gender TSLC 1 42060 7574O15075 SOBHA BOHARA BOHARA Darchula Rithachaupata 3 HARI SINGH BOHARA BIMA BOHARA AMKUR 890.1 Female 2 39231 7569013048 Sanju Singh Bajura Gotree 9 Gyanendra Singh Jansara Singh Manikanda 902.7 Male 3 40574 7559004049 LOGAJAN BHANDARI Humla ShreeNagar 1 Hari Bhandari Amani Bhandari Bhandari gau 907 Male 4 40374 6560016016 DHANRAJ TAMATA Mugu Dhainakot 8 Bali Tamata Puni kala Tamata Dalitbada 908.2 Male 5 36515 7569004014 BHUVAN BAHADUR BK Bajura Martadi 3 Karna bahadur bk Dhauli lawar Chaurata 908.5 Male 6 43877 6960005019 NANDA SINGH B K Mugu Kotdanda 9 Jaya bahadur tiruwa Muga tiruwa Luee kotdanda mugu 910.4 Male 7 40945 7535076072 Saroj raut kurmi Rautahat GarudaBairiya 7 biswanath raut pramila devi pipariya dostiya 911.3 Male 8 42712 7569023079 NISHA BUDHa Bajura Sappata 6 GAN BAHADUR BUDHA AABHARI BUDHA CHUDARI 911.4 Female 9 35970 7260012119 RAMU TAMATATA Mugu Seri 5 Padam Bahadur Tamata Manamata Tamata Bamkanda 912.6 Female 10 36673 7375025003 Akbar Od Baitadi Pancheswor 3 Ganesh ram od Kalawati od Kalauti 915.4 Male 11 40529 7335011133 PRAMOD KUMAR PANDIT Rautahat Dharhari 5 MISHRI PANDIT URMILA DEVI 915.8 Male 12 42683 7525055002 BIMALA RAI Nuwakot Madanpur 4 Man Bahadur Rai Gauri Maya Rai Ghodghad 915.9 Female 13 42758 7525055016 SABIN AALE MAGAR Nuwakot Madanpur 4 Raj Kumar Aale Magqar Devi Aale Magar Ghodghad 915.9 Male 14 42459 7217094014 SOBHA DHAKAL Dolakha GhangSukathokar 2 Bishnu Prasad Dhakal -

District Hospital, Sirha COVID 19 PCR LAB NEW REPORT LIST-16/05/2021
District Hospital, sirha Province - 2, Sirha, Nepal COVID 19 PCR LAB NEW REPORT LIST-16/05/2021 TOTAL NUMBER OF SAMPLE TESTED - POSITIVE RESULT - Collection Report Date S. No. Patient Id Name A.yr/G Address District Contact Result Date 1 21/05/10 21/05/14 SH 1585 Janki Kr Sah 45/f Bhagwanpur-4 Siraha Negative 2 21/05/10 21/05/12 SH 1586 Ramchandra Sah 58/m Bhagwanpur-4 Siraha Negative 3 21/05/10 21/05/12 SH 1587 Aasharam Kamait 14/m Sukhipur-10 Siraha Negative 4 21/05/10 21/05/12 SH 1588 Sanjib kamait 16/m Sukhipur-10 Siraha Negative 5 21/05/10 21/05/12 SH 1589 Sunita Kumari Mahato 45/f Mirchaiya-1 Siraha Negative 6 21/05/10 21/05/12 SH 1590 Ramesh mukhiya 44/m Dhangadhimai-1 Siraha Negative 7 21/05/10 21/05/12 SH 1591 Bijay Kumari sahani 34/m Dhangadhimai-1 Siraha Negative 8 21/05/10 21/05/12 SH 1592 Punita Sahani 29/f Dhangadhimai-1 Siraha Negative 9 21/05/10 21/05/12 SH 1593 Rambilas Sah 70/m Bastipur Siraha Negative 10 21/05/10 21/05/12 SH 1594 Shivsaran Sada 30/m Golbazar-6 Siraha Negative 11 21/05/10 21/05/12 SH 1595 Sharmila shrestha 29/m Golbazar-6 Siraha Negative 12 21/05/10 21/05/12 SH 1596 Ramcharitra Yadav 52/m Siraha-7 Siraha Negative 13 21/05/10 21/05/12 SH 1597 Rubi Ku yadav 20/f Siraha-7 Siraha Negative 14 21/05/10 21/05/12 SH 1598 Rambaran yadav 51/m Bishnupur-2 Siraha Negative 15 21/05/10 21/05/12 SH 1599 Shailendra Kr Sah 25/m Kalyan pur-3 Siraha Negative 16 21/05/10 21/05/12 SH 1600 Santosh Kr Purbey 25/m Mirchaiya-12 Siraha Negative 17 21/05/10 21/05/12 SH 1601 Dinesh Mandal 44/m Sirah-14 Siraha Negative 18 21/05/10